ORIF - Palmar bridge plate
1. Preliminary remarks
Fracture assessment and decision making
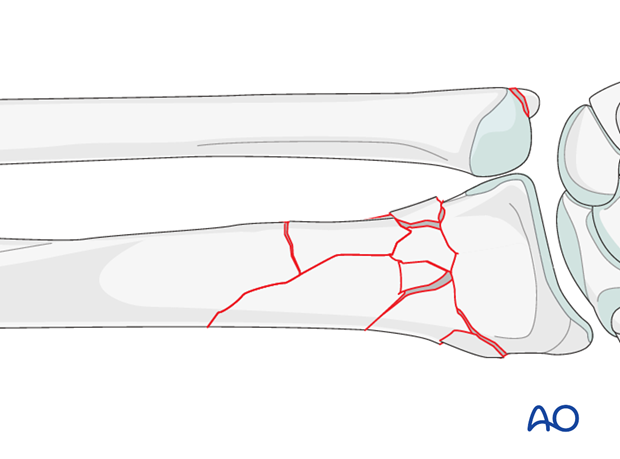
These fractures are extraarticular but multifragmentary. They may often be associated with an ulnar styloid fracture.
Because of extensive comminution, fixation should aim to restore length, axis and rotation. The function of the plate is bridging the comminution and promoting secondary healing with callus formation.
As these injuries are often associated with disruption of the DRUJ, before starting the operation, the uninjured side should be tested as a reference for the injured side.
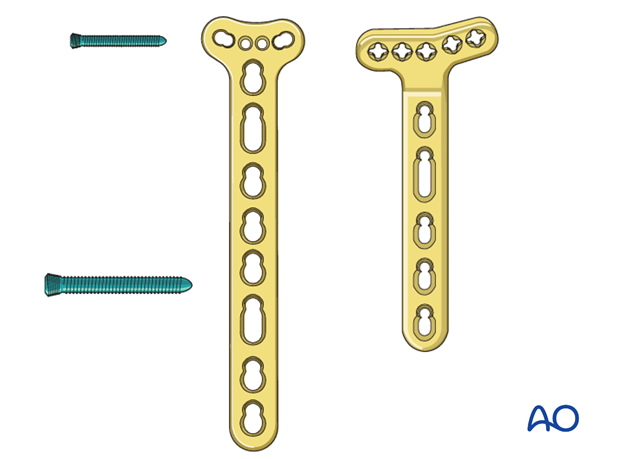
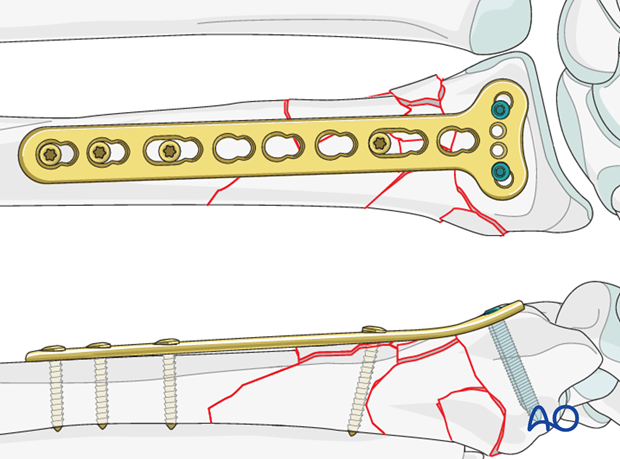
Bridge plating of the distal radius - plate choice
In the presence of extensive metaphyseal comminution, conventional plates do not allow for enough purchase particularly in the proximal fragment. Specially designed, longer, angular stable plates have been developed to allow stable fixation of the distal fragment and metaphyseal bridging of the comminution.
2. Patient preparation and approach
Patient preparation
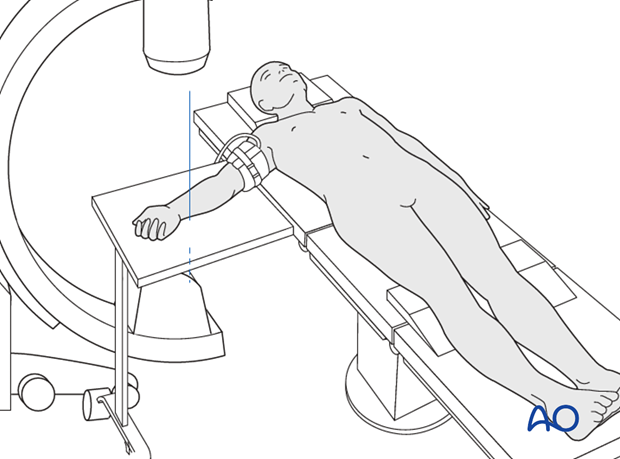
This procedure is normally performed with the patient in a supine position for palmar approaches.
Approach
The radial shaft is approached using a classical Henry’s palmar (anterior) approach.
A thorough knowledge of the anatomy around the wrist is essential. Read more about the anatomy of the distal forearm.
3. Radial plate fixation
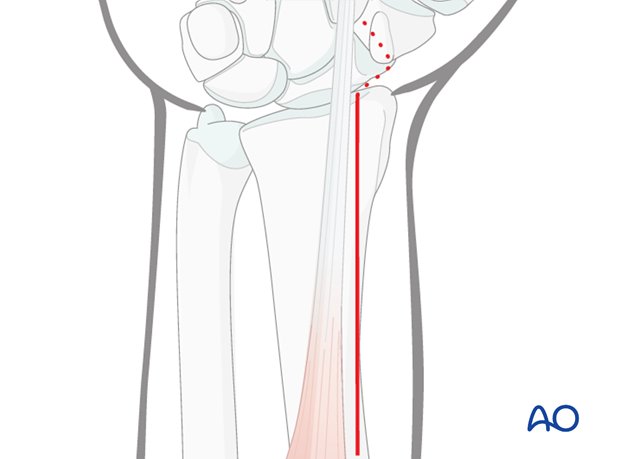
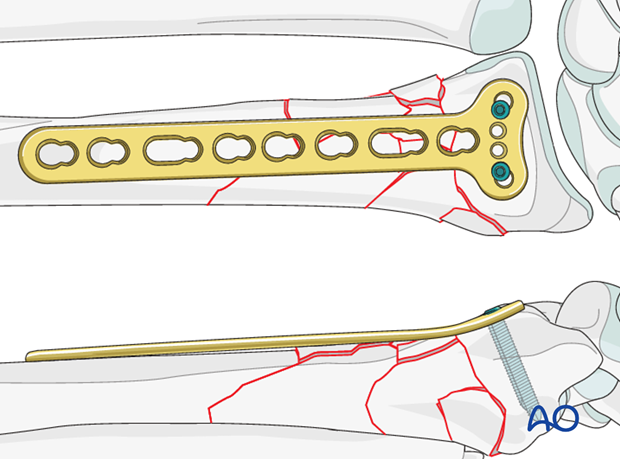
The plate is pre-contoured distally, so it is already adapted to the palmar curvature of the distal radius.

Plate insertion
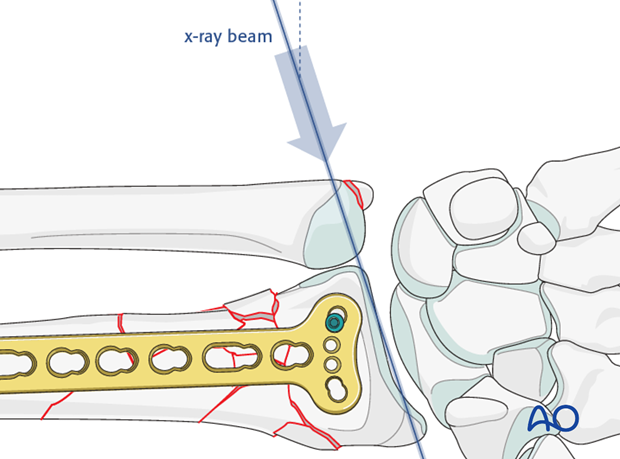
The plate is first positioned distally on the flat intact palmar surface of the distal radius and fixed with distal locking screws parallel to the articular surface. The distal end of the plate should end at the anatomic watershed zone of the distal radius.
The first screw inserted is in the hole on the ulnar side of the plate and its position should be checked under image intensification with the hand elevated 20-30° off the table – in lunate facet view.
The other distal screws should be inserted in a way that the radial inclination of approximately 20° is restored.
Restoring radial length
The correct length of the radius in relation to the ulna should be established preoperatively by taking radiograph of the opposite wrist. The length of the radius in relation to the ulna is then achieved by inserting a unicortical screw just proximal to the proximal end of the plate, and then using a spreader, as illustrated, to move the plate gently distally.
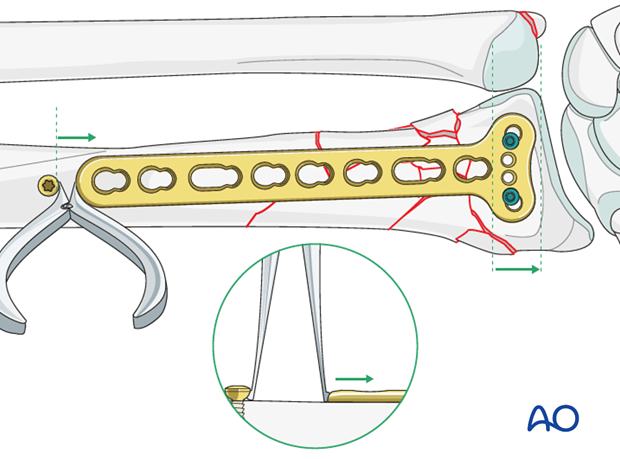
Once the correct length is achieved, the plate is provisionally fixed proximally with standard screws.
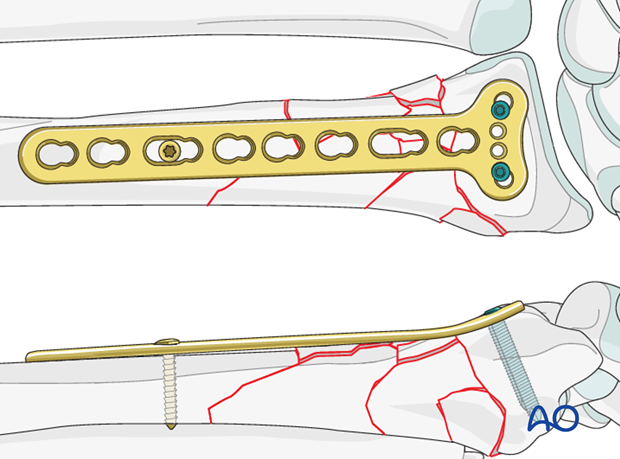
The relationship of the radius to the distal ulna is checked under image intensification before the plate is fixed with additional proximal screws
4. Assessment of Distal Radioulnar Joint (DRUJ)
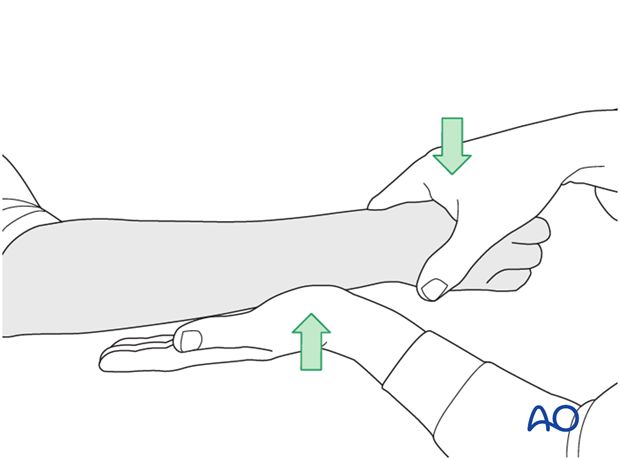
Before starting the operation, the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
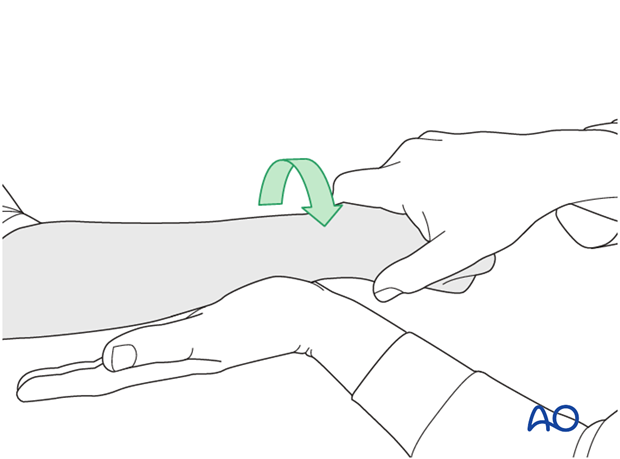
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
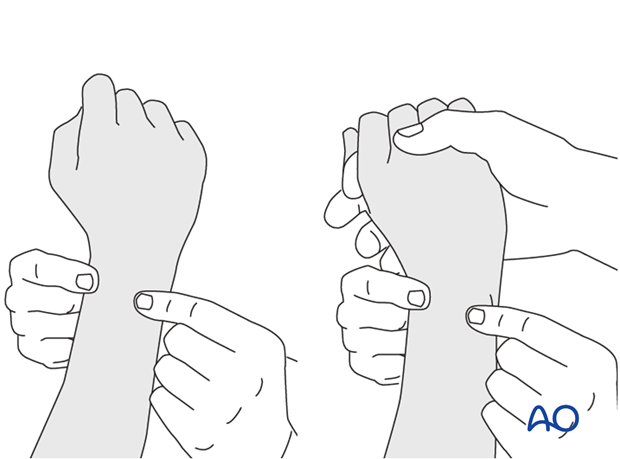
This is repeated with the wrist in full supination and full pronation.
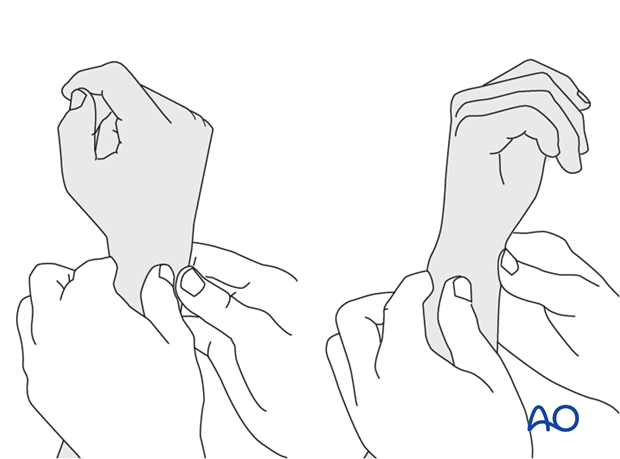
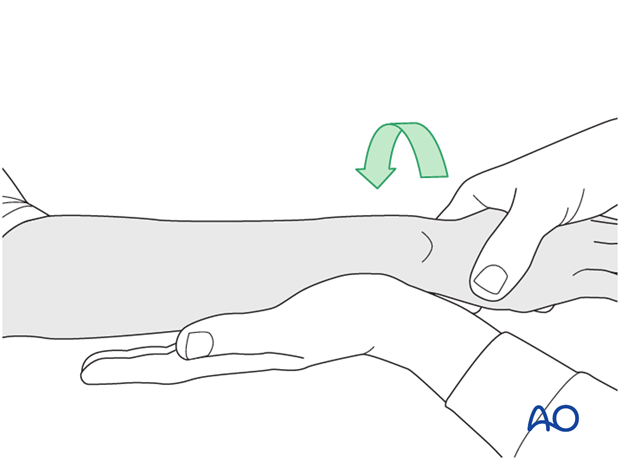
Method 2
To test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
...while the forearm is passively put through full supination...
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
5. Aftercare
Functional exercises
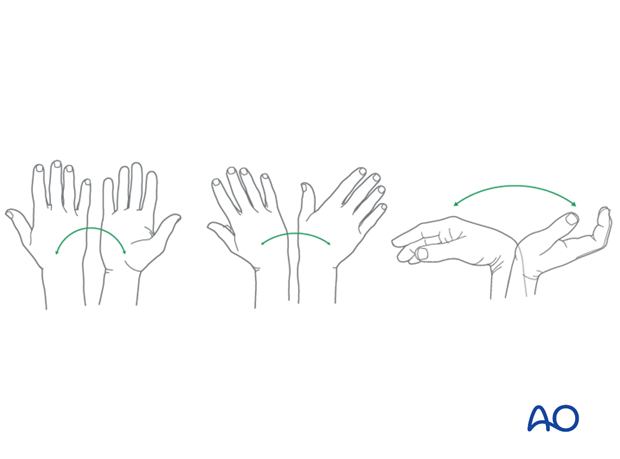
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
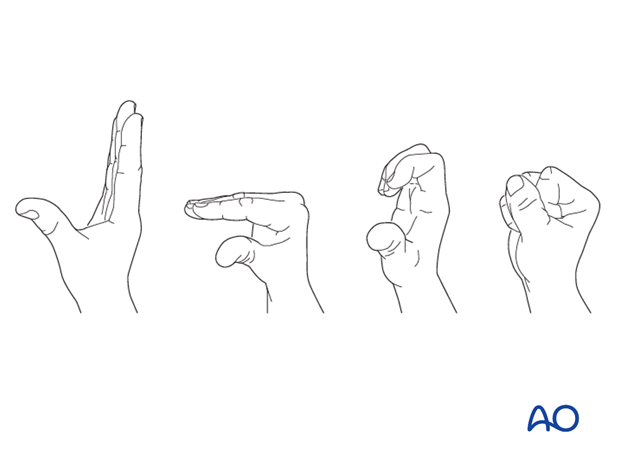
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.
6. Case
Extra articular distal radial fracture in a 20-year-old, with dorsal displacement.
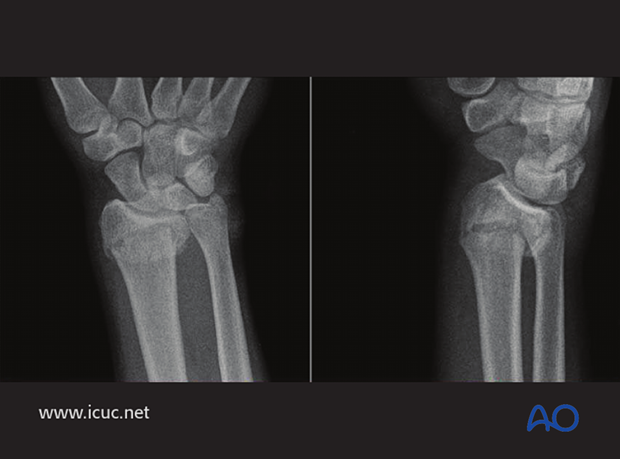
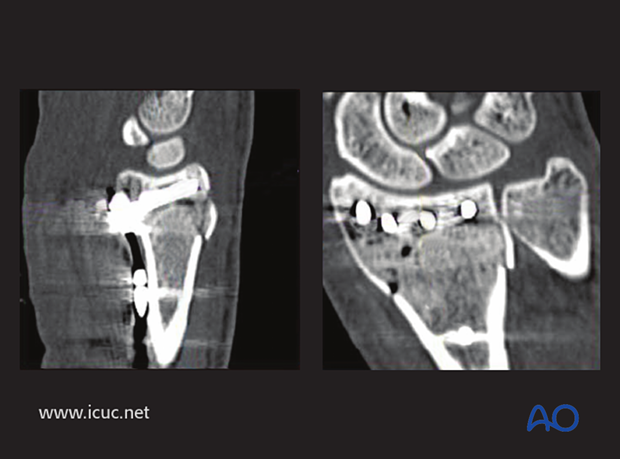
On these CT images, this appears to be an extra-articular facture with some dorsal comminution.
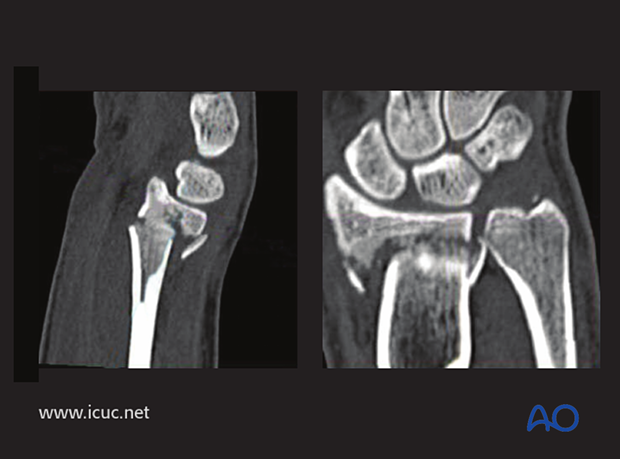
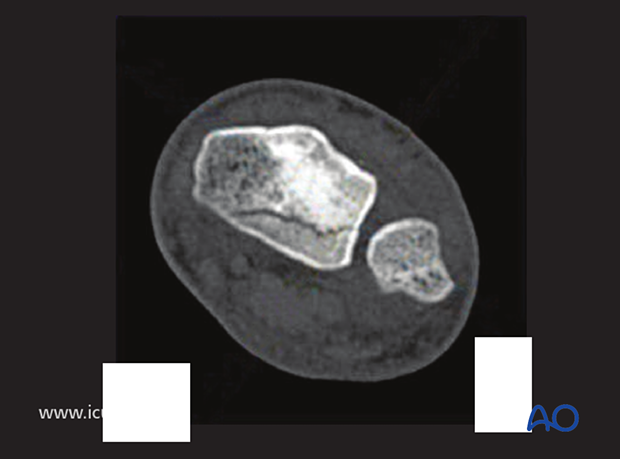
On this image, there is a small coronal fracture in the distal radius, but with minimal displacement.
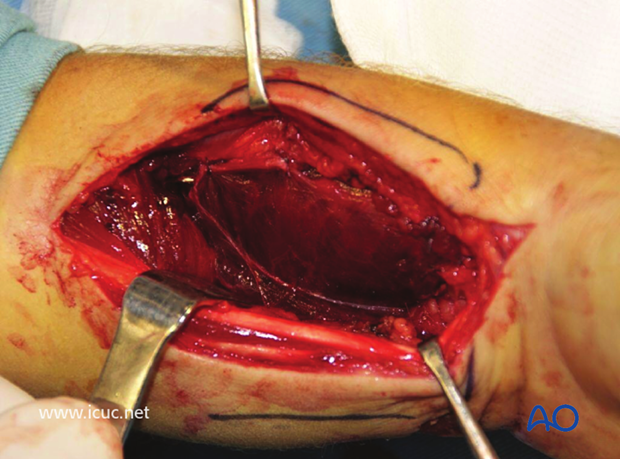
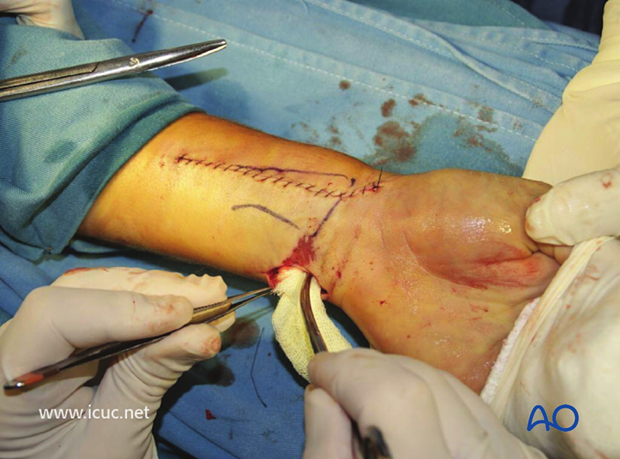
Volar Henry approach through the flexor carpi radialis.
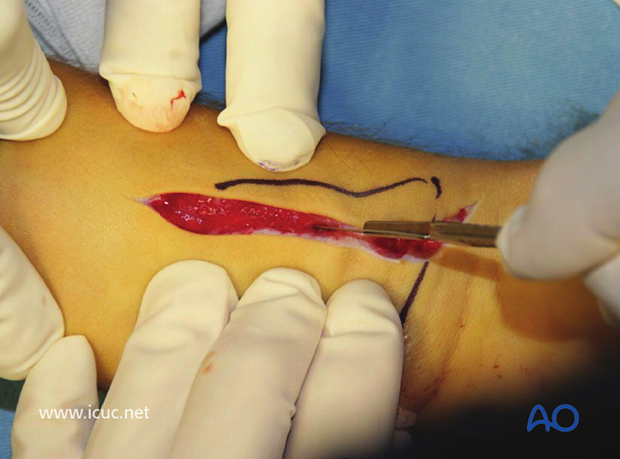
The flexor sheath is opened.

Deep to the flexor sheath lies the pronator quadratus on the volar distal radius.
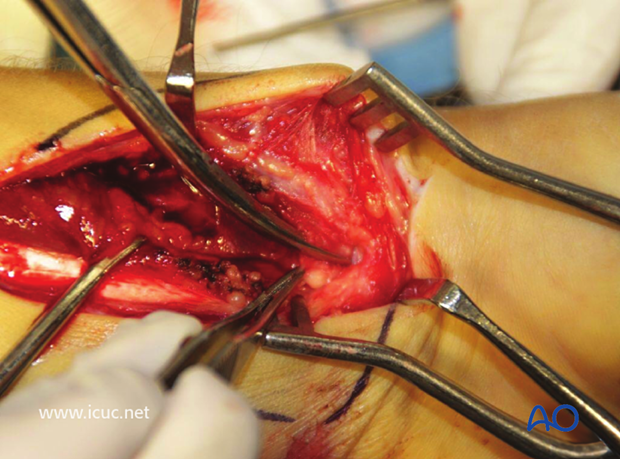
Pronator quadratus has been subperiosteally dissected and reflected, exposing the fracture beneath.
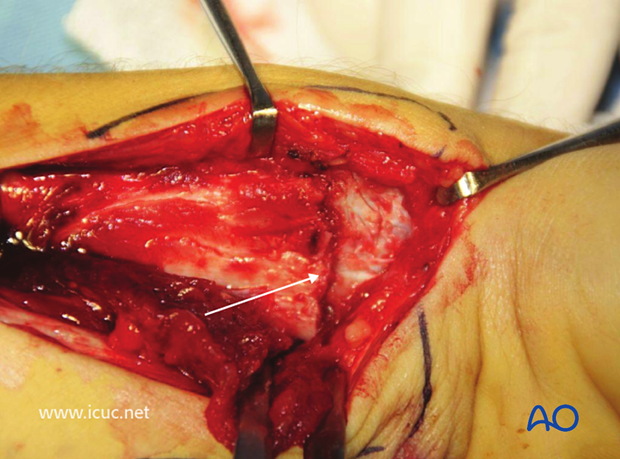
The fracture has been reduced.
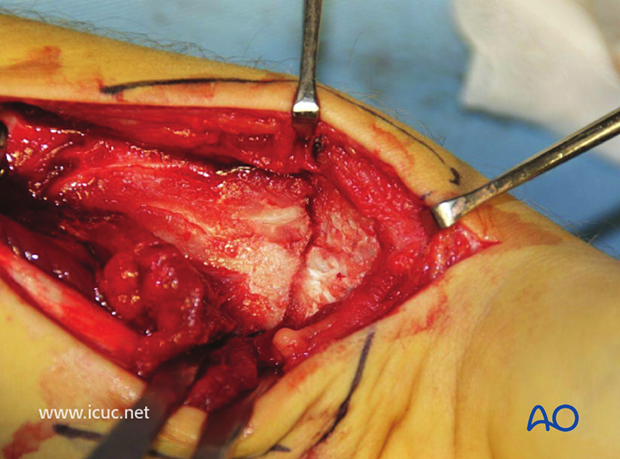
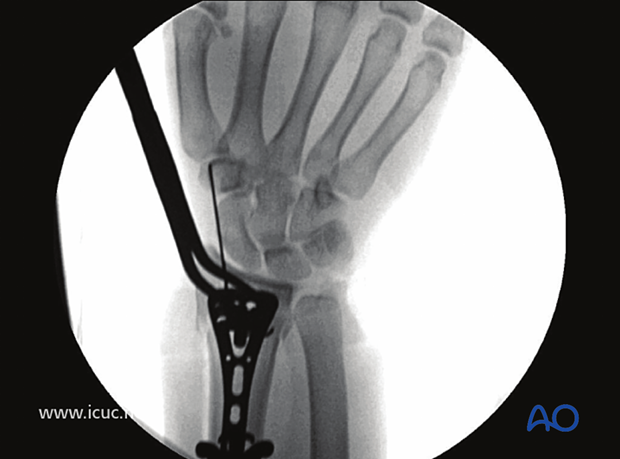
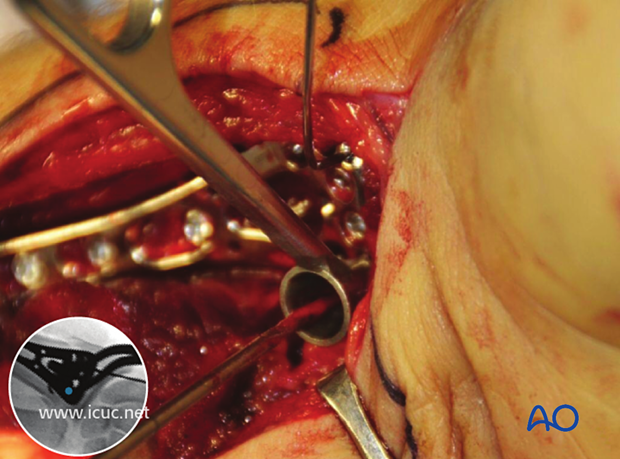
A variable angle plate has been placed on the distal radius with a K-wire used for targeting.

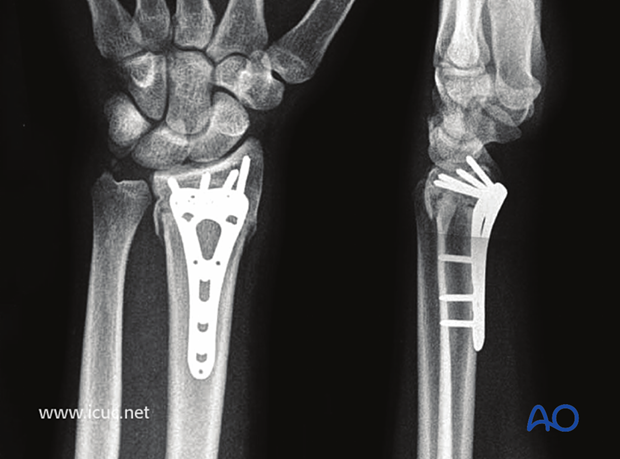
X-ray image demonstrating satisfactory reduction and plate positioning.
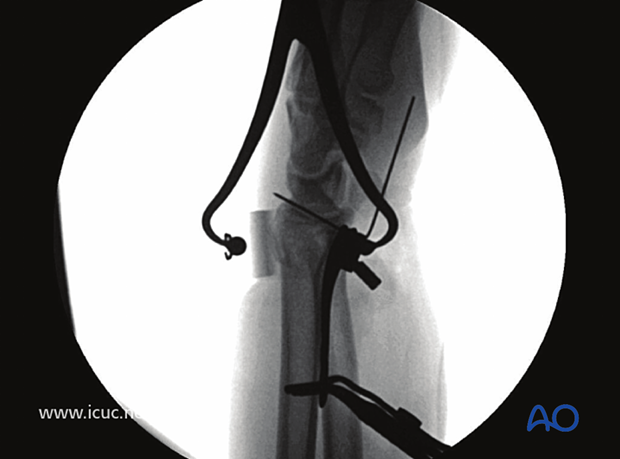
Lateral image under fluoroscopy showing variable angle plate with reduction clamp and dorsal adjunct to ensure reduction is obtained.
The first screw is inserted in the proximal end of the plate, ensuring that the plate is positioned correctly. If it is too distal, the distal screws may compromise the joint.

A variable angle drill guide is used in the distal most screw holes, taking care that the screw trajectory will be subchondral and not into the joint.
Fluoroscopic image demonstrating all distal screws are extraarticular.
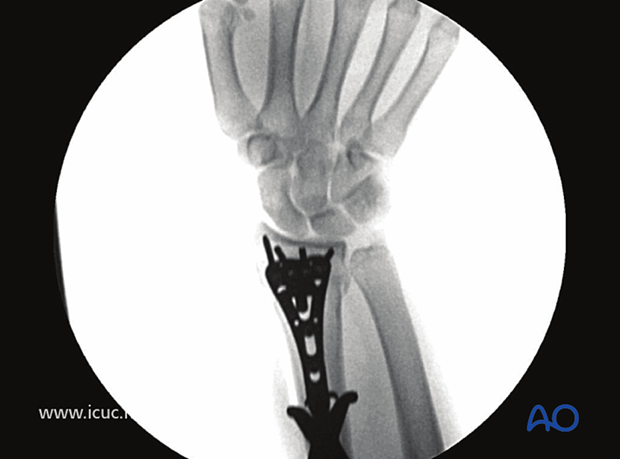
Lateral fluoroscopic image demonstrating that the screws are extra-articular. To ensure the radial styloid screw is extra articular, a styloid view with 20° of angulation must be performed.

Initial closure with the volar plate covered with the pronator quadratus.
Final closure of the Henry approach. This injury was accompanied by a small volar open wound.
Postoperative CT showing extraarticular position of variable angle screws.
5 weeks postoperative images showing healing of the distal radius
10 weeks clinical images showing flexion, extension, and rotation is returning.
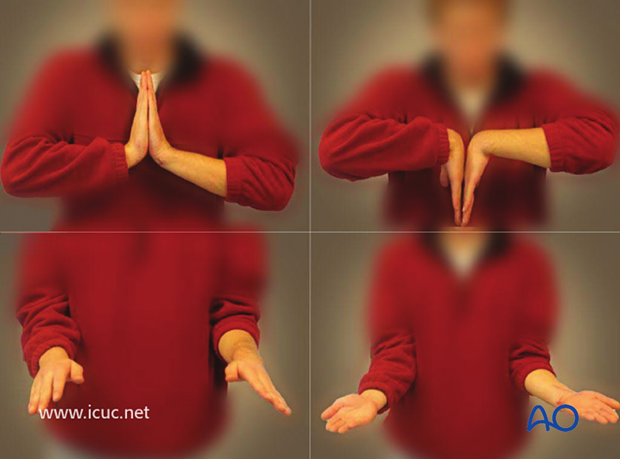
At 1 year, movement has returned almost to normal.














