ORIF - Lag screw and protection plate
1. Principles
Fracture assessment
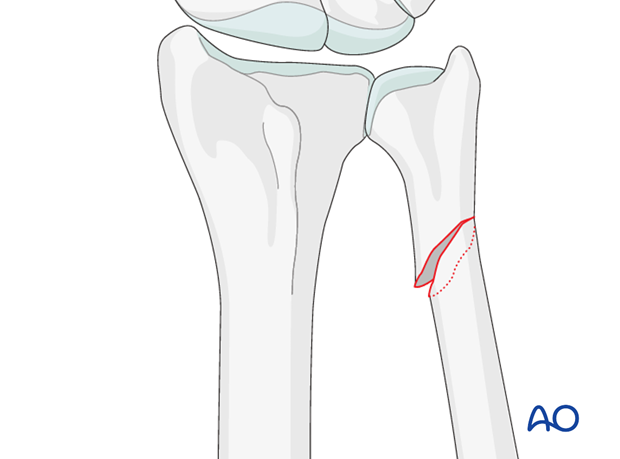
Internal fixation of ulnar shaft fractures restores the length of the ulna and congruency of the distal radioulnar joint (DRUJ). Oblique and spiral fractures may be fixed with a lag screw and a protection plate. If the distal ulnar fragment is short, a locking plate, or mini condylar plate may be used.
In transverse ulnar fractures (“defense fractures”) a pre-contoured compression plate is used.
These fractures are not usually associated with DRUJ injuries, but it is good practice to assess the joint after fixation in all cases.
2. Patient preparation and approach
Patient preparation
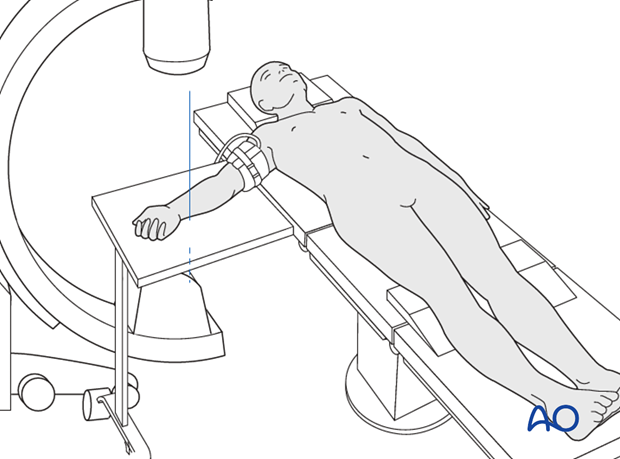
This procedure is normally performed with the patient in a supine position for distal ulnar fractures.
Approach
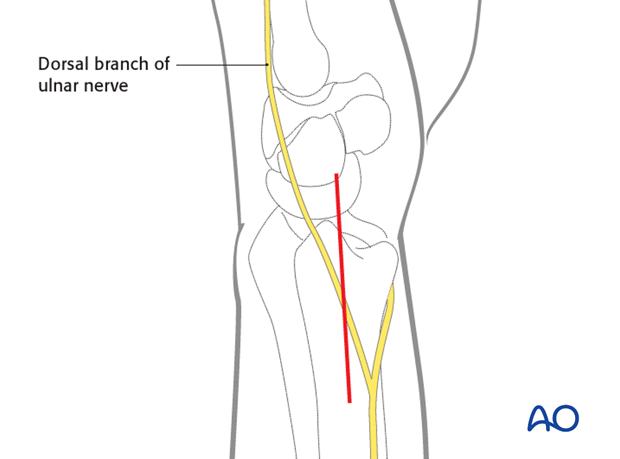
For this procedure an ulnar approach is normally used.
3. Reduction and preliminary fixation with lag screws
Reduction
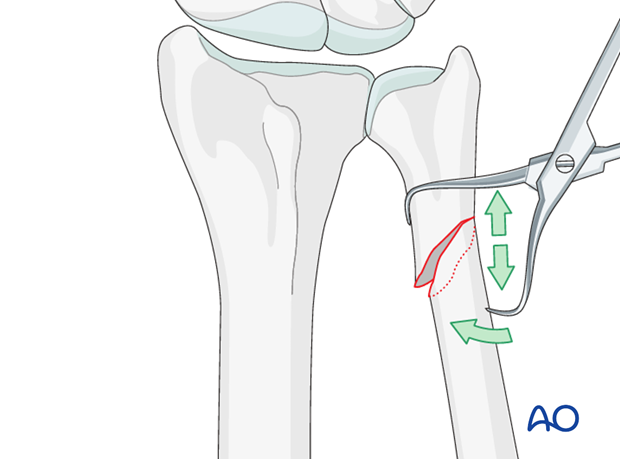
Anatomical reduction is achieved using a pointed reduction forceps.
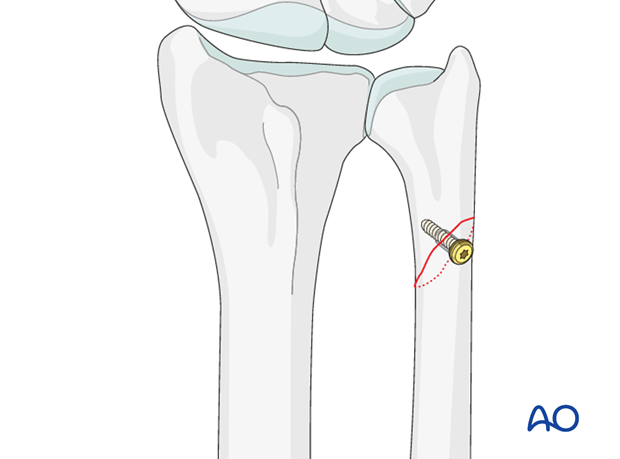
Insertion of a lag screw
After anatomical reduction, the fracture is fixed with one or two interfragmentary lag screws, depending on the length of the fracture zone.
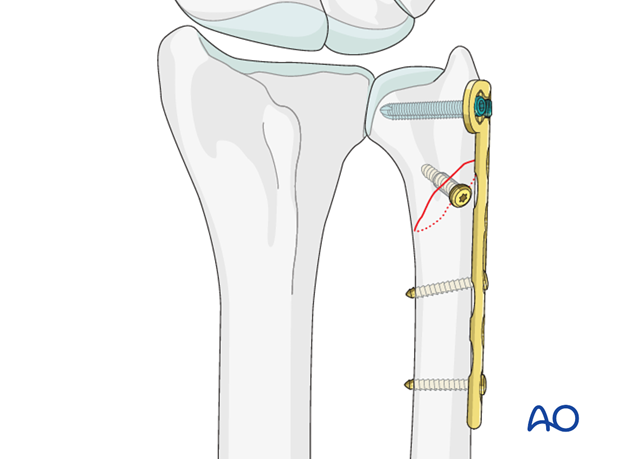
4. Insertion of a protection plate
If available, a low profile plate should be used, as soft tissue irritation is a common postoperative problem.
The plate is applied without axial compression, to protect the lag screw fixation. At least 2 screws must gain a hold in the distal fragment.
In osteoporotic bone, the use of locking screws improves the purchase.
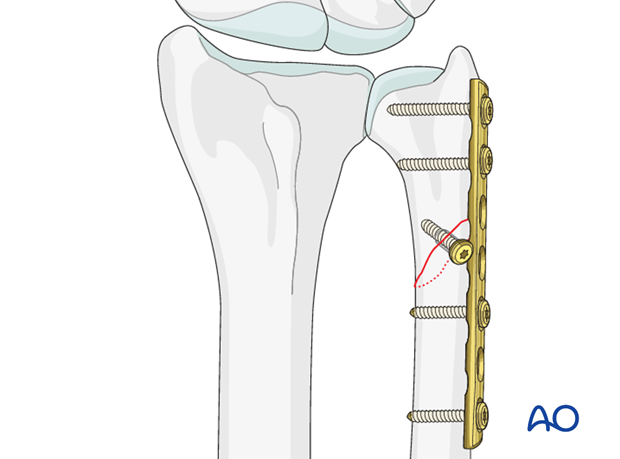
If the distal fragment is very short, a condylar or a T-plate with two locking screws may give more secure fixation.
5. Assessment of Distal Radioulnar Joint (DRUJ)
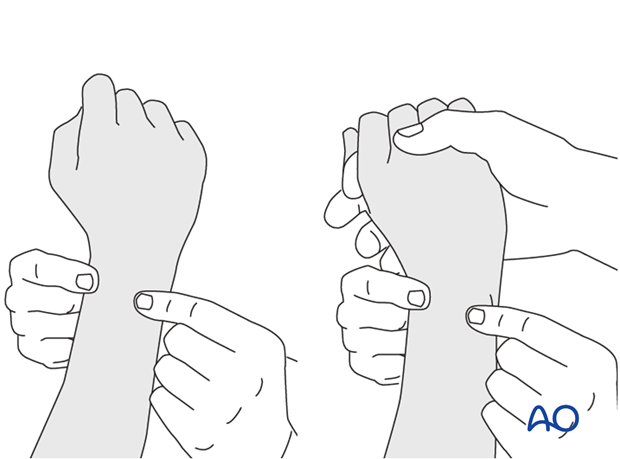
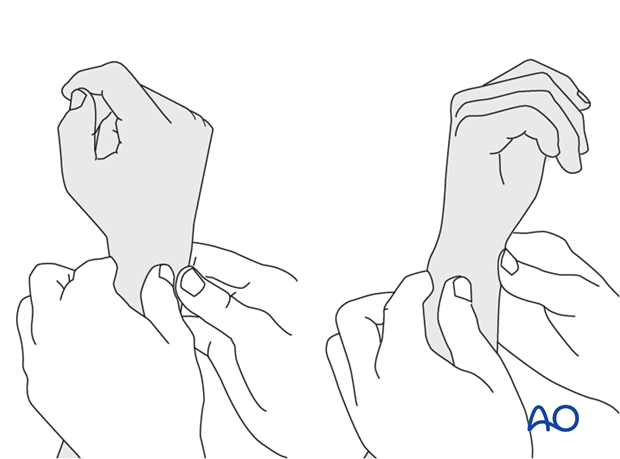
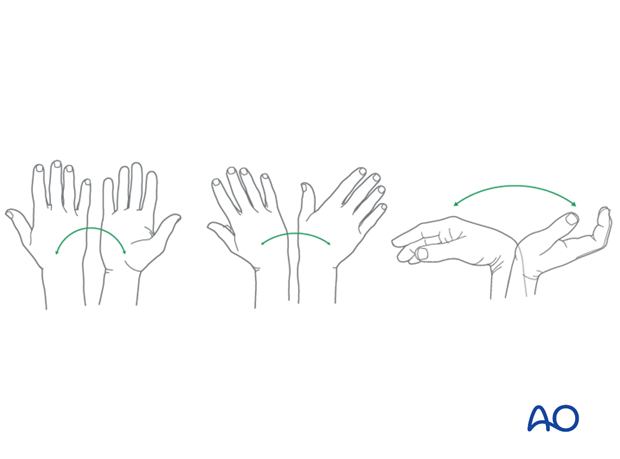
Before starting the operation, the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
This is repeated with the wrist in full supination and full pronation.
Method 2
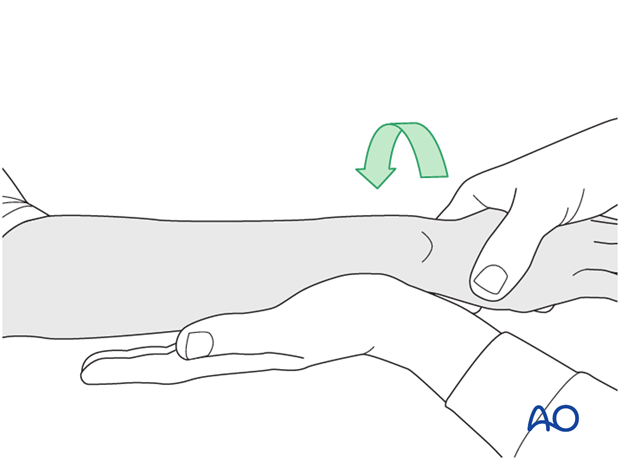
To test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
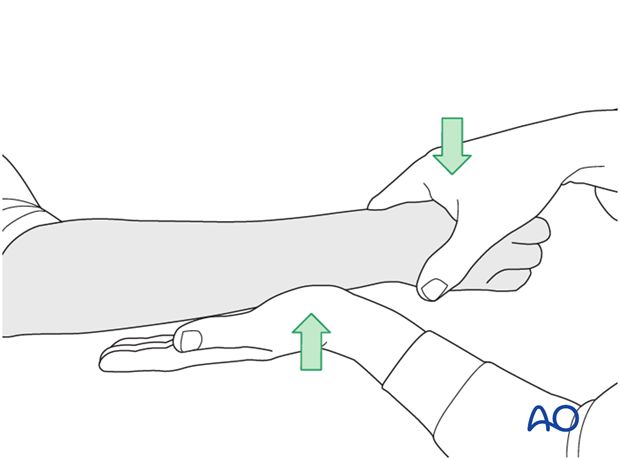
...while the forearm is passively put through full supination...
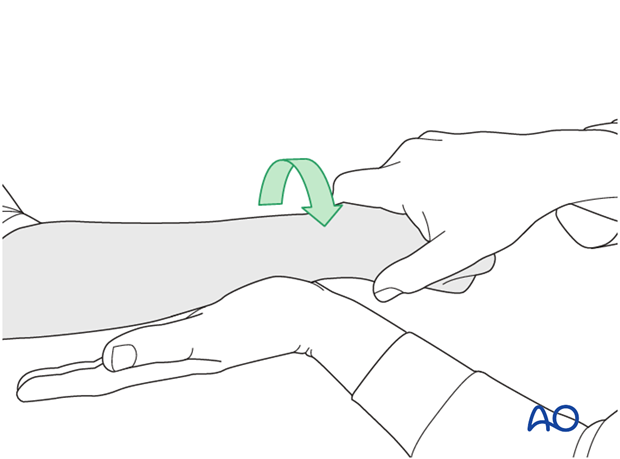
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
6. Aftercare
Functional exercises
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
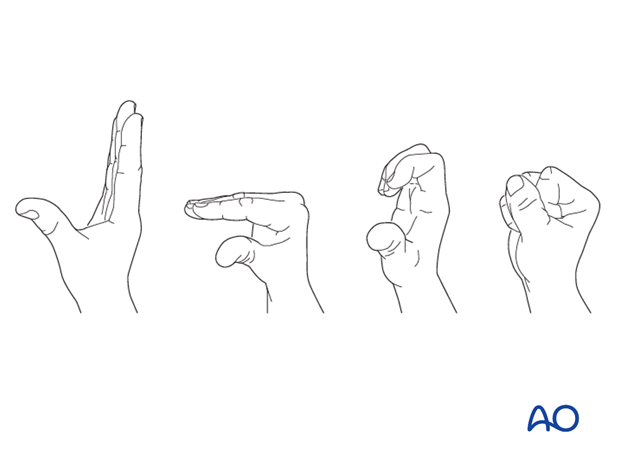
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.













