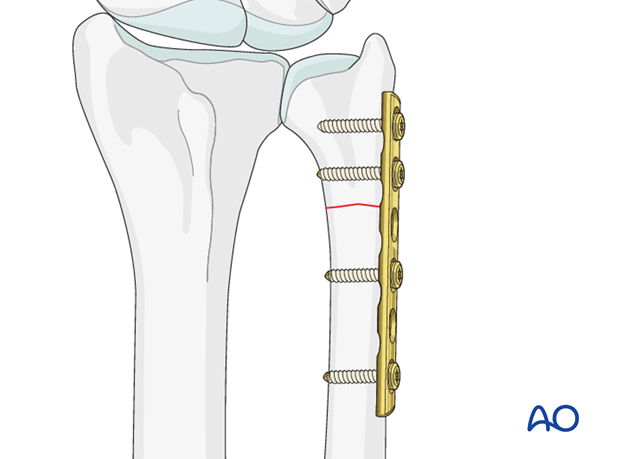
ORIF - Compression plate
1. Preliminary remark
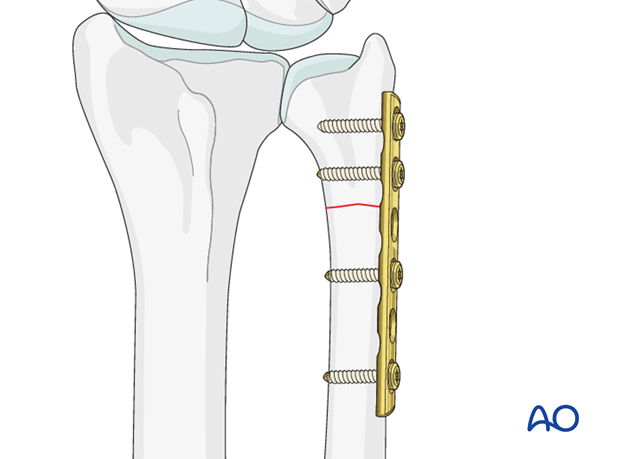
If the ulnar fracture is transverse, or a very short oblique fracture, it is not possible to insert a lag screw across the fracture plane. In such a case, the fracture is treated by axial compression by eccentric screw placement in the plate holes, so that as the screws are tightened the fracture is compressed.
2. Patient preparation and approach
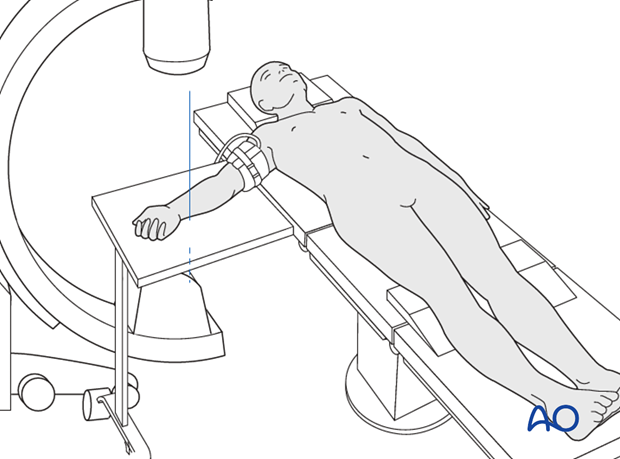
Patient preparation
This procedure is normally performed with the patient in a supine position for distal ulnar fractures.
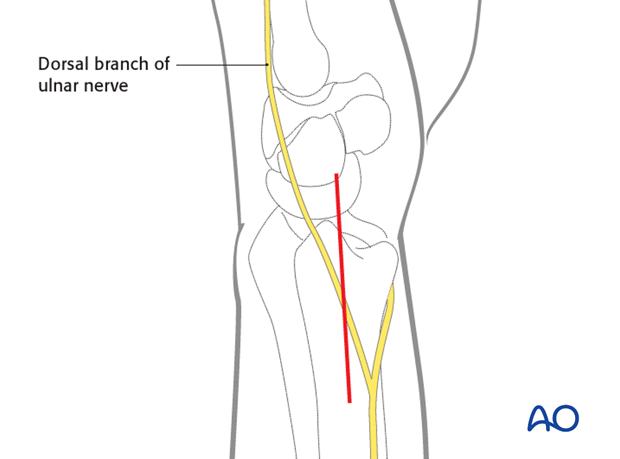
Approach
For this procedure an ulnar approach is normally used.
3. Plate selection and contouring
If available, a low profile plate should be used, as soft tissue irritation is a common postoperative problem.
If the distal fragment is small, fixation may be more secure if a condylar T-plate is used.
The plate is contoured so that as it sits on the bone, with the fracture reduced anatomically, its central portion overlying the fracture stands about 1 mm off the cortex. This ensures that as the screws are tightened, and the plate is pulled to the bone, compressive force is also applied to the far cortex.
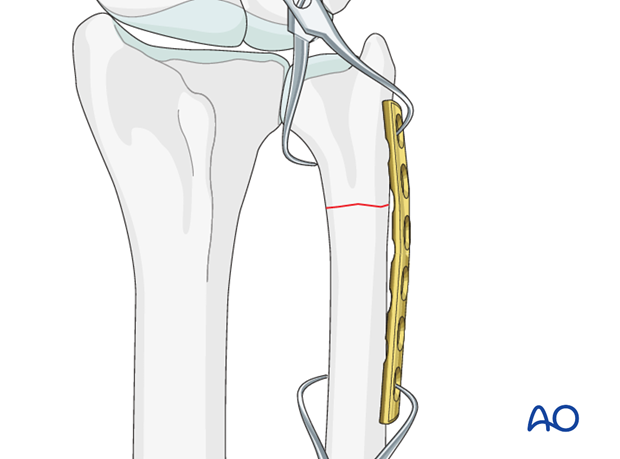
4. Reduction and fixation
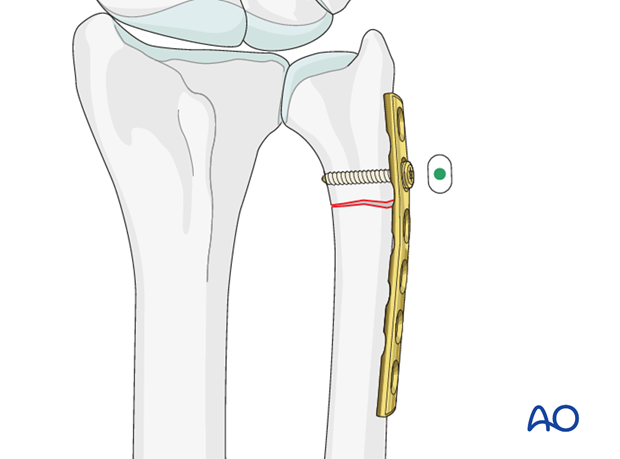
Insertion of neutral screw
The plate is fixed to the distal fragment using one standard neutral cortical screw through the plate hole nearest the fracture.
If locking plates are available locking screws are recommended in the distal fragment.
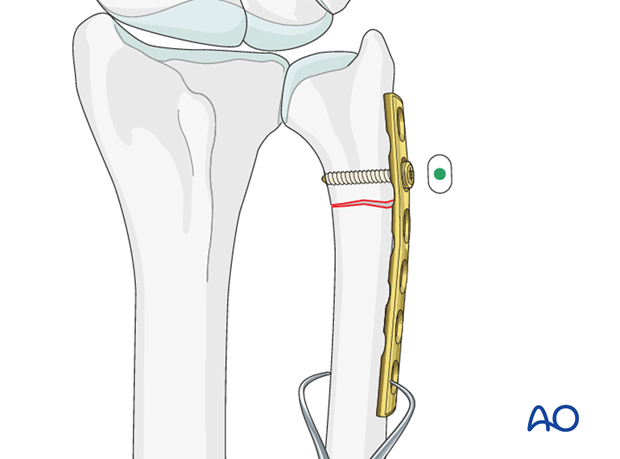
Check fracture alignment
The alignment of the fracture, and the lie of the plate along the long axes of the fragments are checked and the plate held to the proximal fragment using a bone holding clamp.
Compression by eccentric insertion of second screw
The next step is carefully to insert a screw in the plate hole nearest to the fracture – this is a load screw and so the hole is drilled eccentrically.
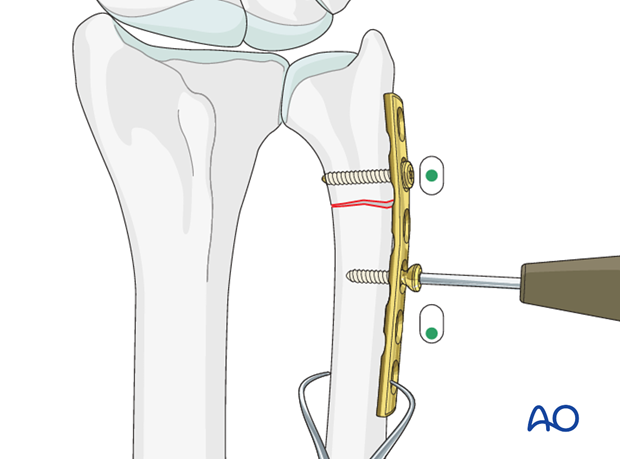
Before tightening the compression screw, the distal fixation may be made more secure by inserting the distal screw(s).
As the load screw is tightened, the fracture site is compressed – the clamp is released to allow the relative plate/bone movement to produce the compression.
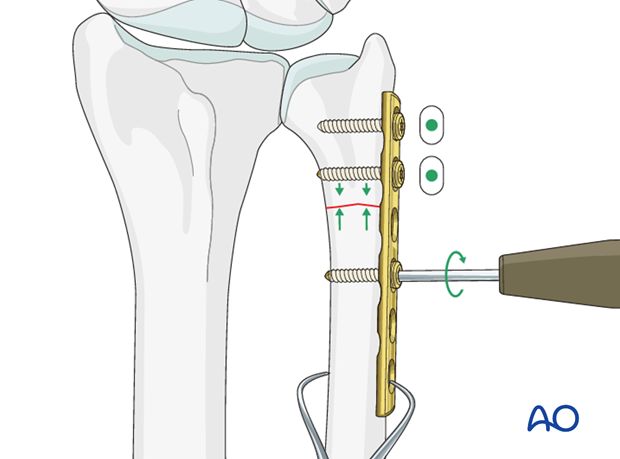
Complete fixation
The remaining screws are then added using the neutral insertion technique.
5. Aftercare
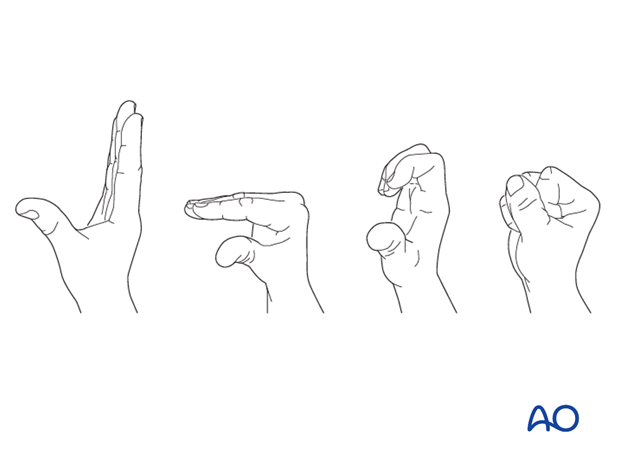
Functional exercises
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
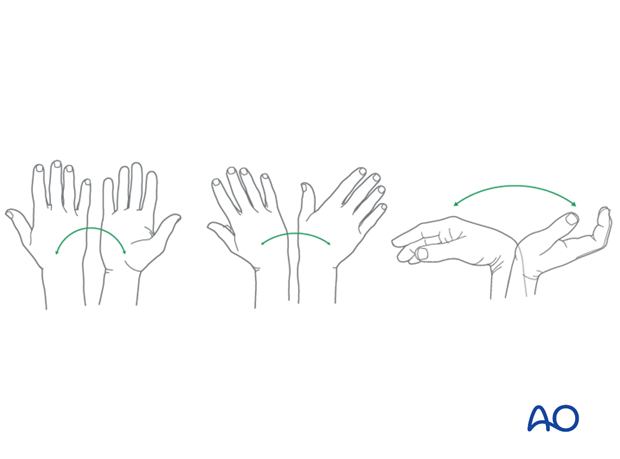
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.













