ORIF - Cerclage wire
1. Preliminary remarks
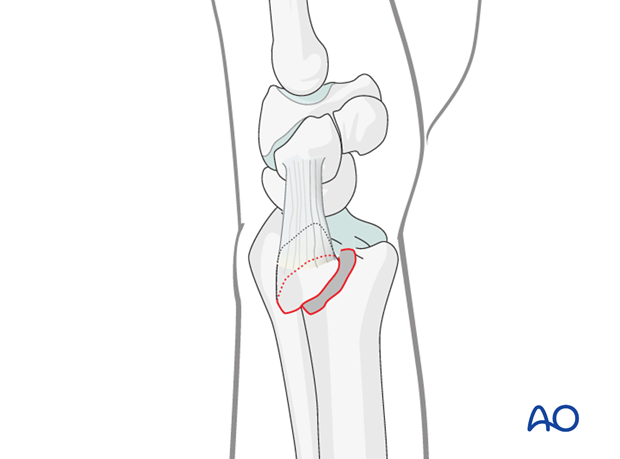
Fracture assessment
Ulnar styloid fractures can extend from the very distal tip to fractures at the base of the styloid, and may or may not be associated with instability of the distal radioulnar joint.
They may also be associated with injury to the triangular fibrocartilaginous complex (TFCC).
Indications
In the rare cases with significant instability, fixation of an ulnar styloid fragment should be considered. This may be with a cerclage wire, or if the ulnar styloid fragment is sufficiently large, screw fixation may be an option.
This wire was referred to as a “Tension band wire”. We now prefer the term “Cerclage wire”.
2. Patient preparation and approach
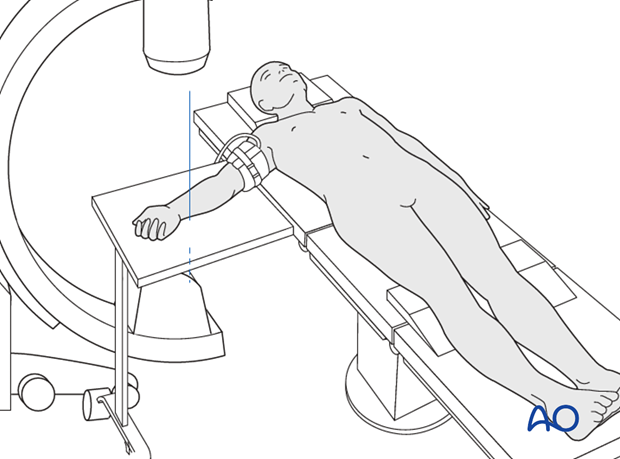
Patient preparation
This procedure is normally performed with the patient in a supine position for distal ulnar fractures.
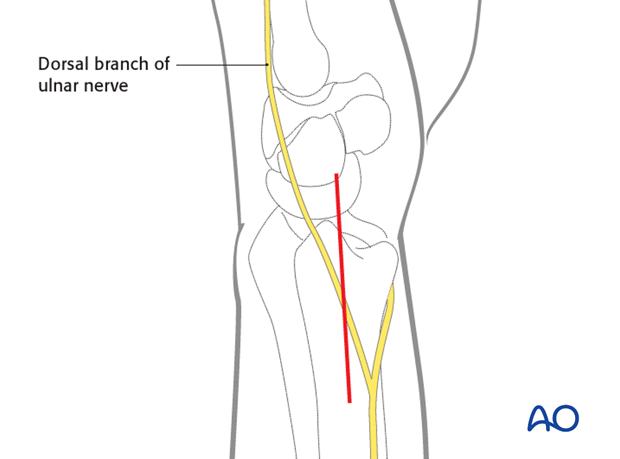
Approach
For this procedure an ulnar approach is normally used.
3. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation, the uninjured side should be tested as a reference for the injured side.
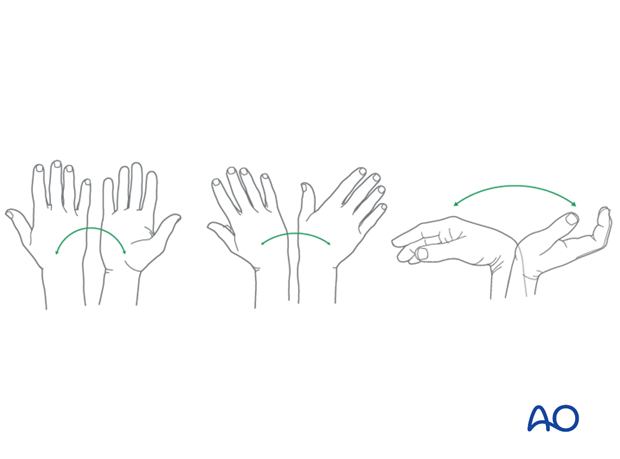
The distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
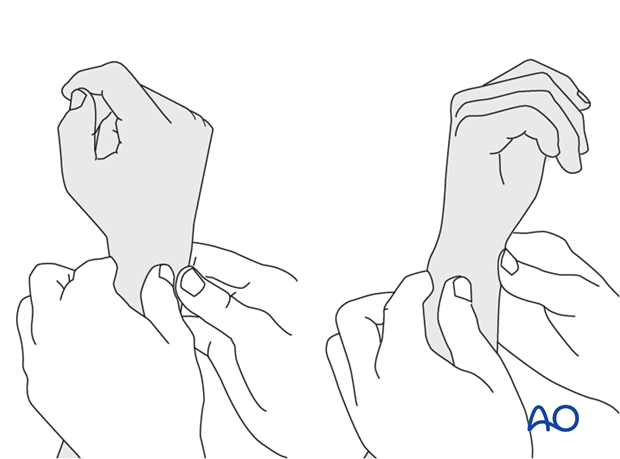
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
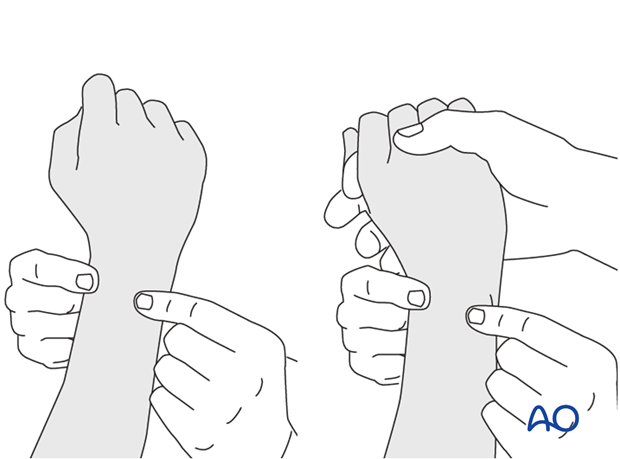
This is repeated with the wrist in full supination and full pronation.
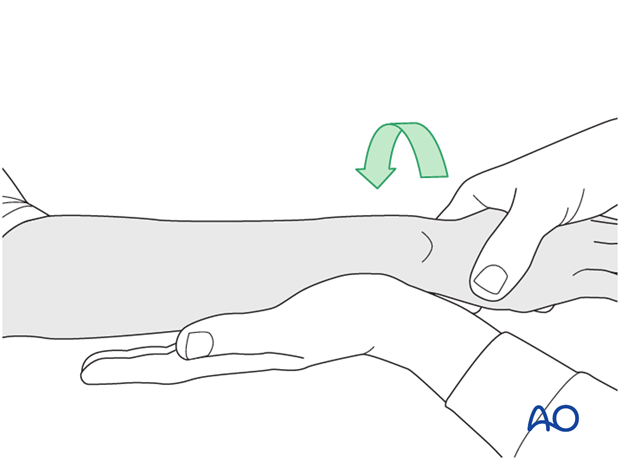
Method 2
To test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
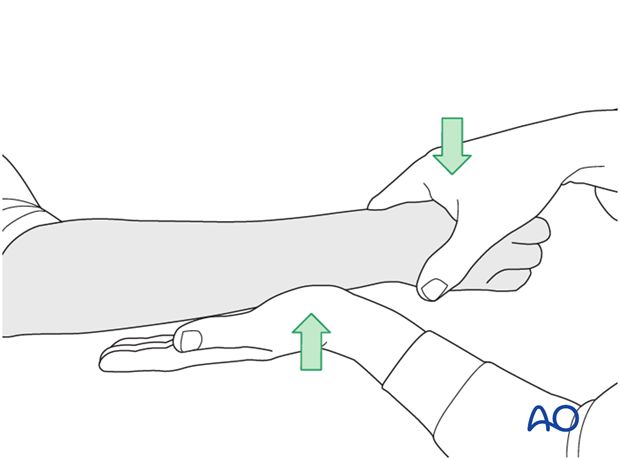
...while the forearm is passively put through full supination...
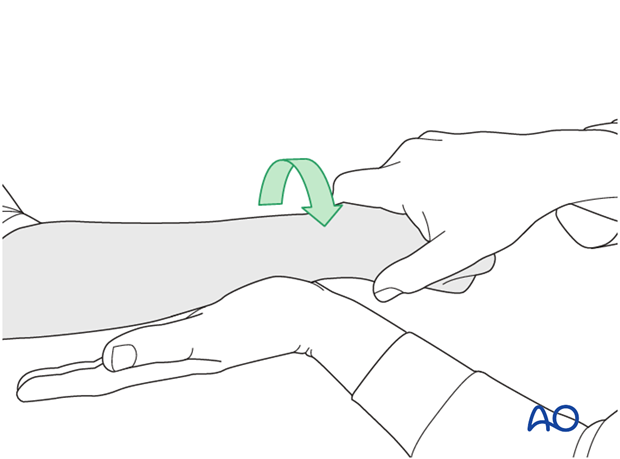
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
4. Direct reduction
Irrigate and clean the fracture site of hematoma.
The fragment is reduced by direct manipulation, aided using a small pointed reduction clamp. It is important to recognize that the ulnar styloid is occasionally more palmar than it would appear in a radiograph.
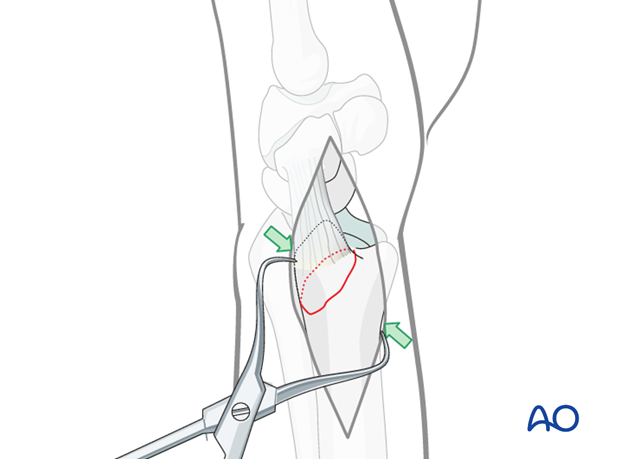
Reduction with stay suture
A strong stay suture can be inserted around the tip of the styloid, analogous to the application of a cerclage wire.
By pulling proximally on this suture, the ulnar styloid is reduced.
Alternatively, the fracture may be reduced using a dental pick.
The ulnar styloid must not be overreduced, to avoid overtension of the TFCC, which may cause restriction of forearm rotation.
5. Insertion of a cerclage wire
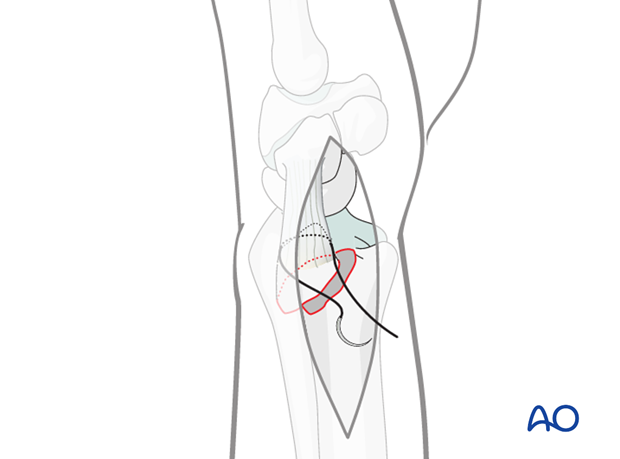
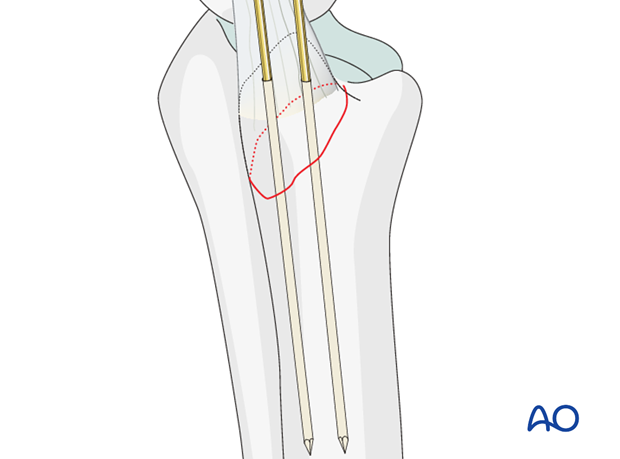
Insert the K-wires
If there is enough room, insert two smooth K-wires from the tip of the styloid in such a direction as to engage their tips in the opposite cortex of the ulna proximal to the DRUJ.
Check the position of the K-wires using image intensification. Check that full rotation is possible.
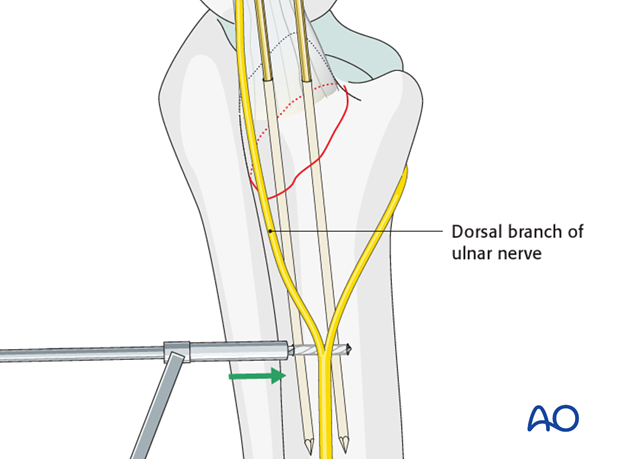
Drill hole
Drill a hole through the ulna from dorsal to palmar approximately 2 cm proximal from the tip of the styloid. Care needs to be taken to avoid injury to the dorsal cutaneous branch of the ulnar nerve.
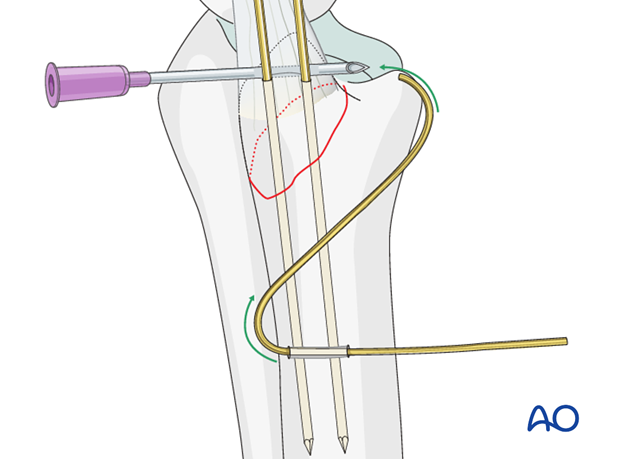
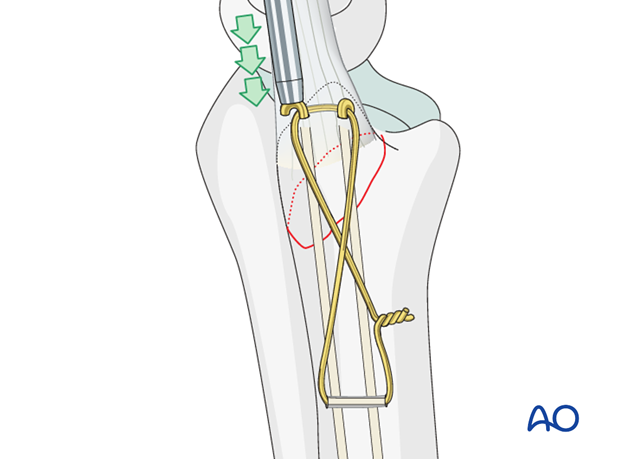
Insert the wire
Pass a wire through the drill hole and, using a hypodermic needle as a guide, the wire is passed around the K-wires distally, to create a figure-of-eight loop.
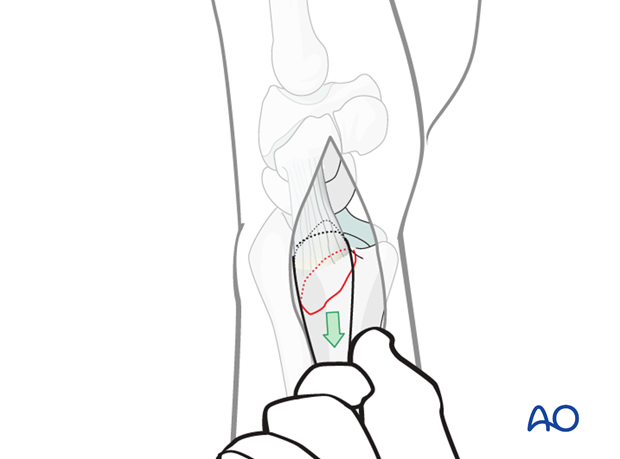
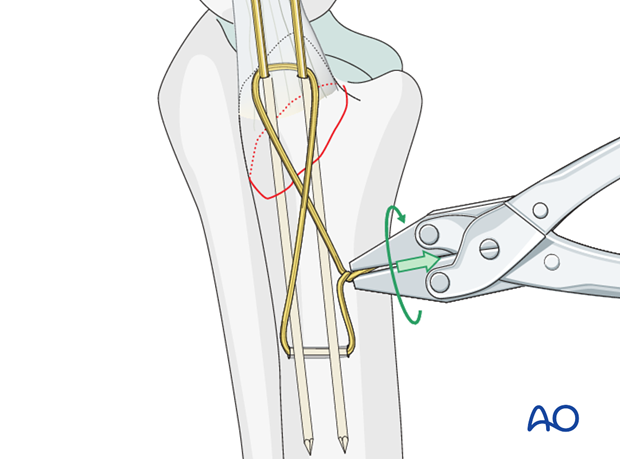
Apply tension to the wire
The wire twist is begun, ensuring that each end of the wire spirals equally. The wire is tensioned by pulling on the twist until the desired tension is achieved, and then twisted to take up the slack created.
Cut the twist and bend it towards the bone, so as not to irritate the soft tissues.
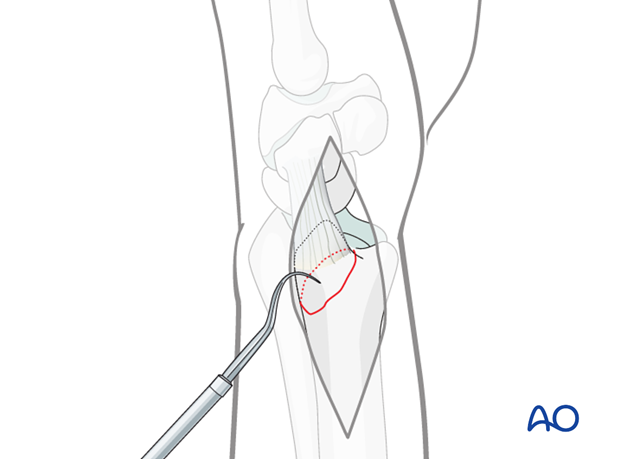
Bury the K-wires
Using the bending iron for K-wires, the wires are bent at the level of the tip of the styloid through 180º, and cut short.
They are then impacted into the bone using a small punch, or other appropriate tool.
Confirm using image intensification to ensure that the proximal tips of the wires are not in the interosseous space.
Pearl
An alternative to a steel wire figure of eight, a heavy suture may be used. This is less likely to cause soft-tissue irritation.
6. Aftercare
Functional exercises
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
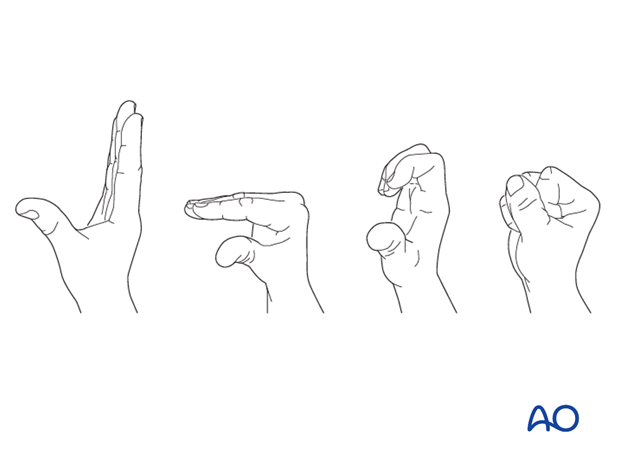
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.













