ORIF - Palmar plate
1. Preliminary remarks
Fracture assessment and decision making
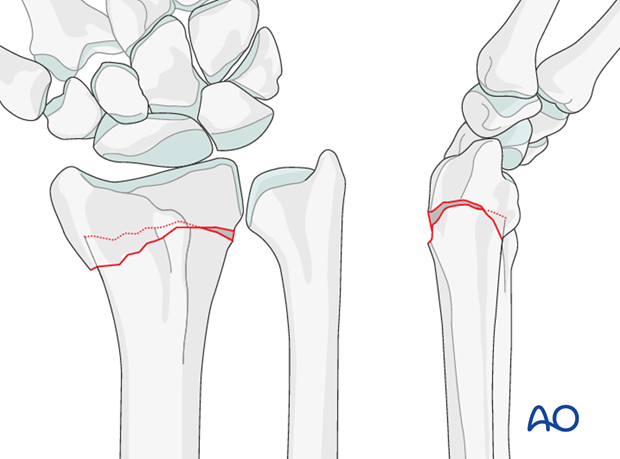
In these injuries, there is a fracture of the distal metaphysis with dorsal displacement. These are often referred to as Pouteau or Colles fractures.
Fractures angulated dorsally >25° associated with osteoporosis or residual void after reduction may prove unstable. Therefore, primary palmar plating may be chosen.
Before palmar plating became a commonly used treatment, most of these fractures were treated with closed reduction, which was then maintained either with K-wires or a plaster cast. Many surgeons now treat most of these fractures with a palmar plate and often use the plate as an aid to reduction.
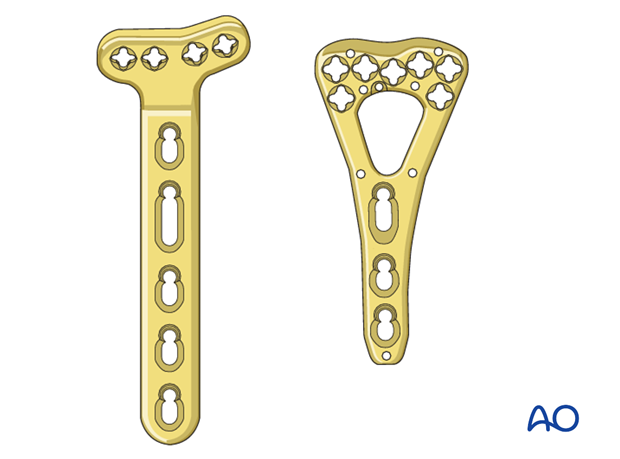
Palmar plate
Advances in plate design have provided angular stable fixation. This allows enhanced stability and ease of application, even in the presence of osteoporotic bone. Plates with variable angle locking screw options may be useful.
Provisional reduction in displaced fractures
Reduction is achieved by applying longitudinal traction either manually or using Chinese finger traps.
The reduction is maintained by a temporary splint.
If definitive surgery is planned, but cannot be performed within a reasonable time scale, a temporary external fixator may be helpful.

2. Associated injuries
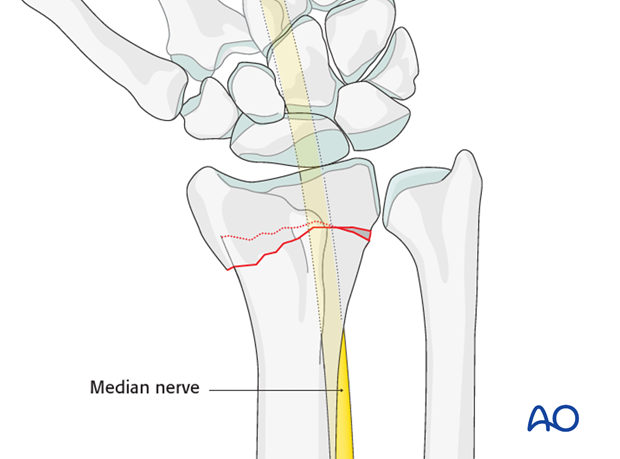
Median nerve decompression
If there is dense sensory loss, or other signs of median nerve compression, the median nerve should be decompressed.
3. Patient preparation and approach
Patient preparation
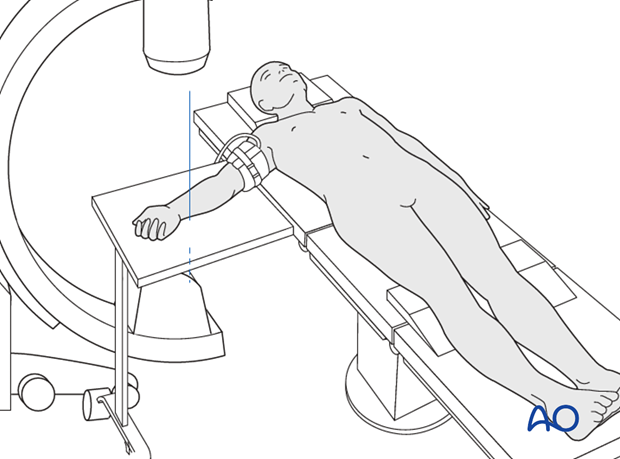
This procedure is normally performed with the patient in a supine position for palmar approaches.
Approach
There are two palmar surgical approaches to the distal radius – a modified Henry approach to the radius and a more ulnar approach, designed to expose the median nerve as well as the distal radius.
A thorough knowledge of the anatomy around the wrist is essential. Read more about the anatomy of the distal forearm.
4. Reduction and fixation
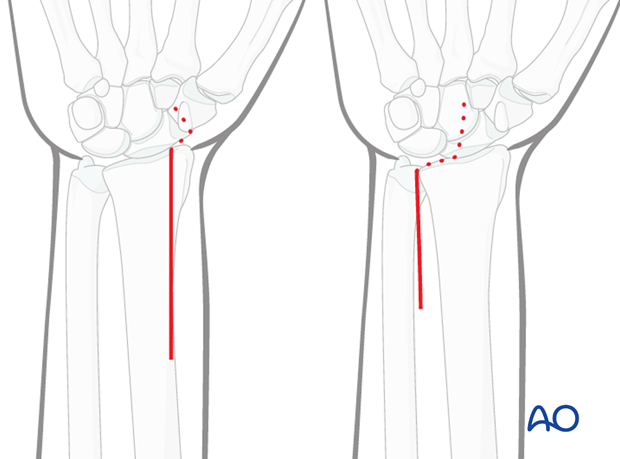
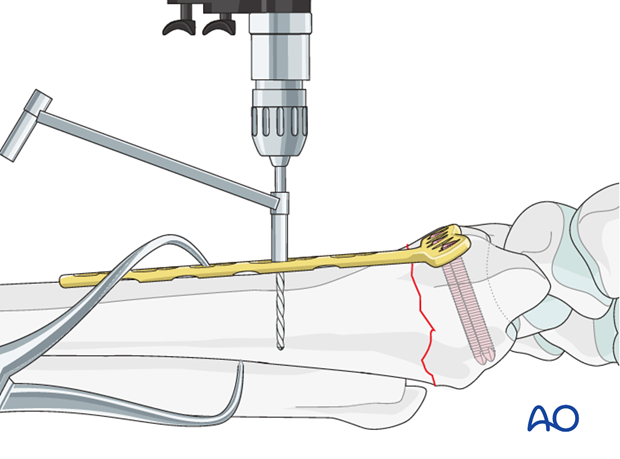
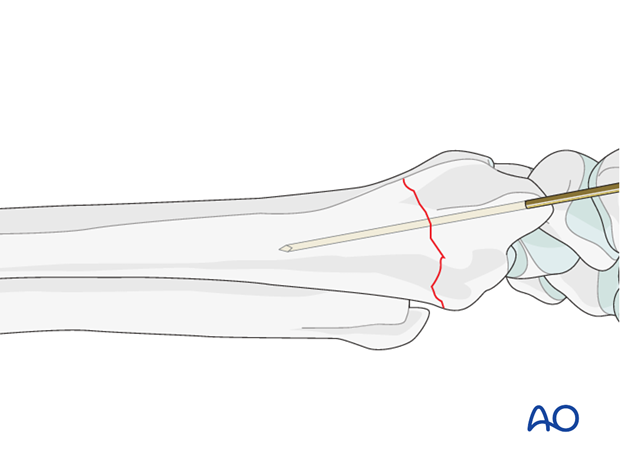
Insert K-wire
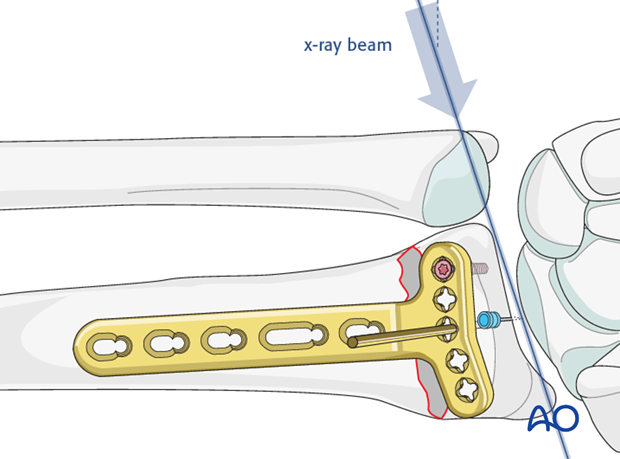
Insert a small smooth K-wire or needle to mark the level and plane of the radiocarpal joint.
If there are fragments blocking reduction they may be removed with a dental pick.
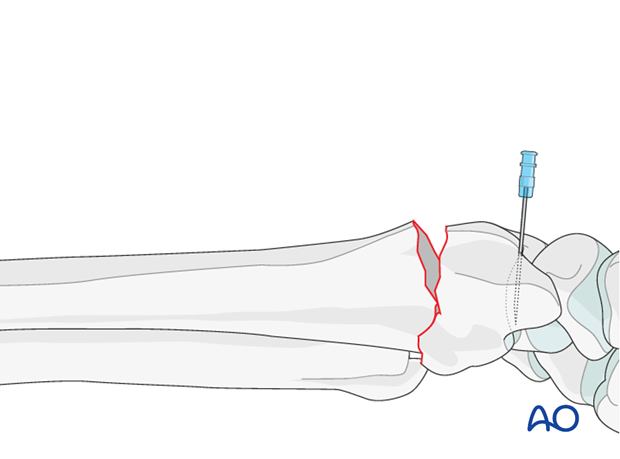
Reduction with plate
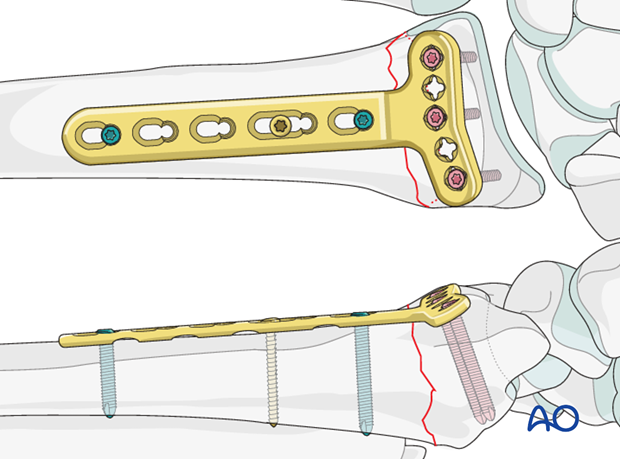
Apply the plate to the distal fragment. The distal end of the plate should end at the anatomic watershed zone of the distal radius.
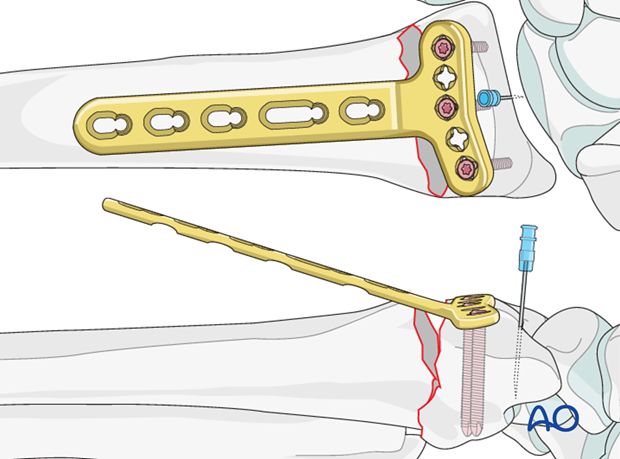
Insert a K-wire through a screw hole, as close to the subchondral bone as possible and parallel to the articular surface.
The angle of the plate to the shaft should equal the angle of the displacement.
Confirm using image intensification.
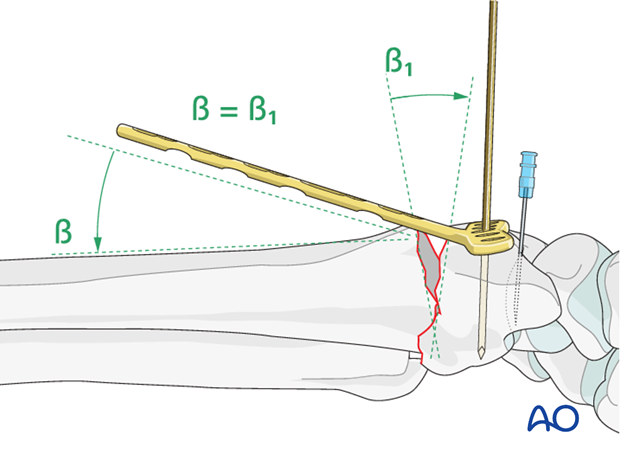
The initial screw is inserted in the most ulnar screw hole. The reason for this is that if the initial screw is placed on the radial side it will block accurate imaging of the ulnar screw placement. Choose a locking head screw, 2-4 mm shorter than measured.
Provided the screw is parallel to the K-wire, it should not enter the radiocarpal joint.
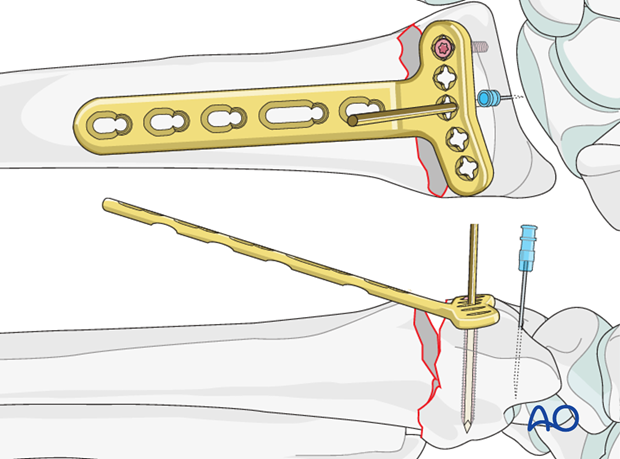
Confirm screw position with a lateral view under image intensification, with the beam aimed at an angle of 20° to the true lateral, clearly showing the joint surface.
Insert at least two other distal locking head screws.
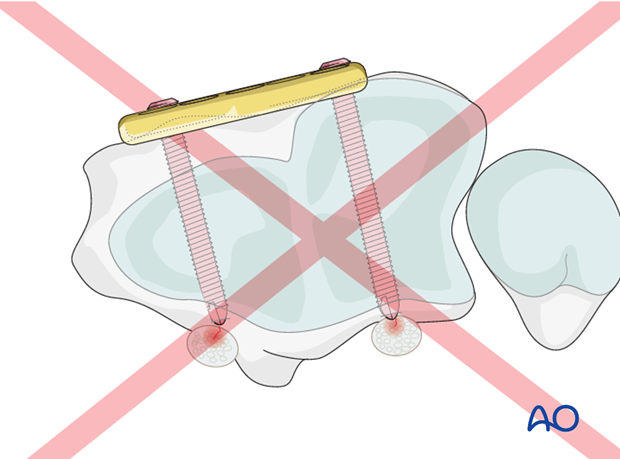
Pitfall: Screw tip protrusion
Due to the prominence of Lister’s tubercle, as seen on the lateral image projection, a screw placed on either side of the tubercle may appear not to protrude through the far cortex.
Protrusion of such a screw may result in extensor tendon irritation and rupture.
Bring the plate onto the shaft and hold it with a clamp. Obtain check radiographs and adjust the position of the distal fragment if necessary by moving the plate.
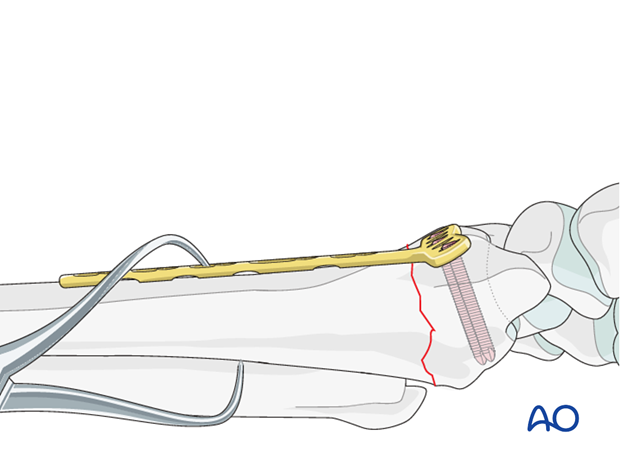
Once satisfactory reduction is confirmed, insert a self-tapping, non-locking screw through the oblong plate hole.
Insert at least two further proximal screws.
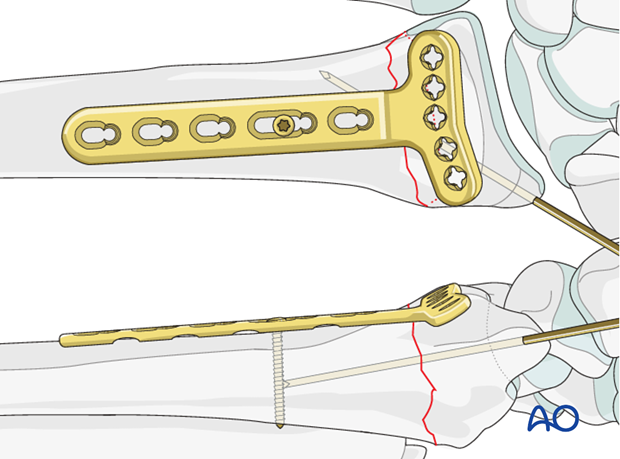
Alternative reduction
Some surgeons feel that using the plate for reduction in osteoporotic patients may cause the screws to loosen in the bone. In such cases, manual reduction and preliminary fixation with K-wires may be preferable.
Apply the plate to the bone. The distal end of the plate should end at the anatomic watershed zone of the distal radius.
Insert a screw through an oblong hole in the proximal radial fragment. Before fully tightening it, check the plate position using intraoperative imaging, adjusting the position of the plate as necessary.
5. Aftercare
Functional exercises
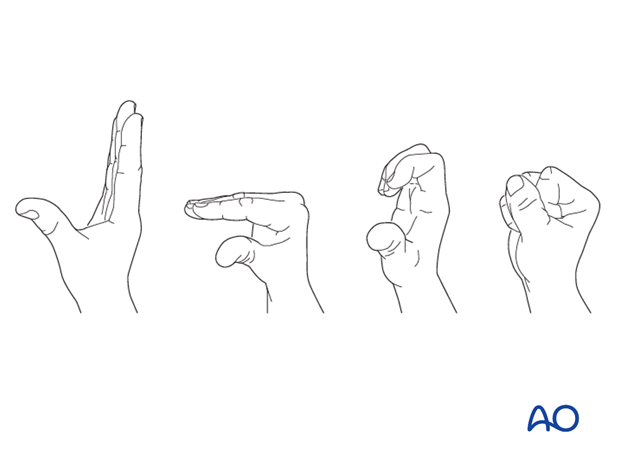
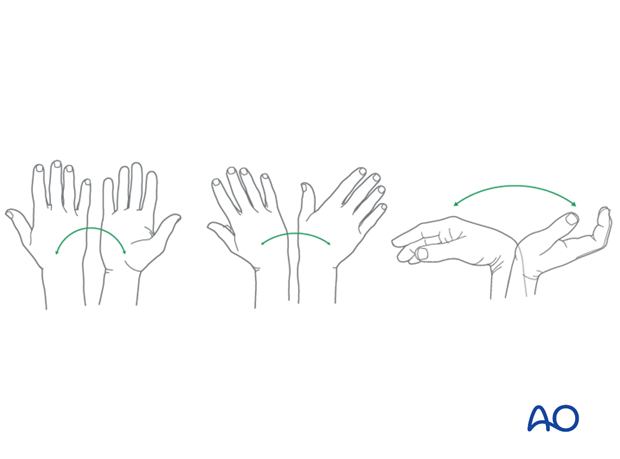
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.













