Temporary long leg splint
1. Principles
General considerations
It can also be used as a temporary aid to fracture stabilization in the multiple injured patient.
Care should always be taken with any splint to protect pressure areas, such as the Achilles tendon, lateral and medial malleoli, and the heel, as ulceration in these areas can be extremely difficult to treat.
Fixed splints should not be applied to patients that have other pathological conditions in the lower limb, a neurological compromise that causes sensory defects (such as spinal injury, or diabetes with peripheral neuropathy), or in patients who are unconscious.
The splint is inexpensive, and both easy and quick to apply. It is not possible, however, to obtain good three-point immobilization of distal femoral fractures with any splint. The conical shape of the thigh will not allow for close apposition of a splint.
For the treatment of distal femur fractures alone, the ankle does not need to be immobilized and therefore a cylinder splint can be used. If there is an ipsilateral ankle, or foot, fracture, the long leg cylinder splint can be converted to one that incorporates the ankle and foot. A cylinder long leg splint is described here, as it is the most commonly used.
Common deformity
It is recognized that perfect realignment of a displaced distal femoral fracture will be impossible with a long leg cylinder splint. However, it helps to bring the fracture out to length and to correct some of the common hyperextension deformity.
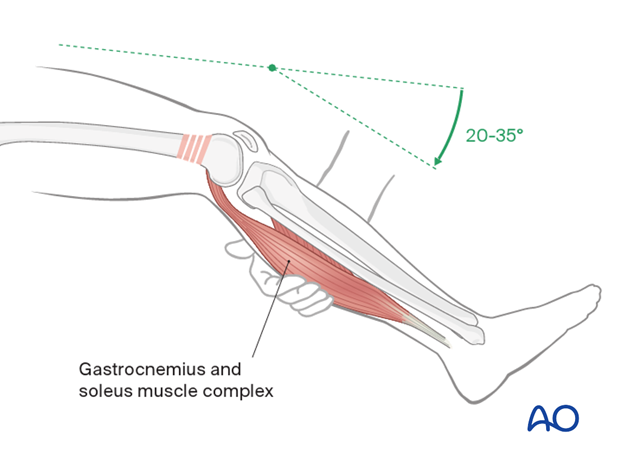
The surgeon applying the long leg splint must remember that the common deformity of a supracondylar femoral fracture is shortening and hyperextension of the distal fragment.
In order to counteract the hyperextension, either a bolster can be placed under the supracondylar region, or preferably the knee can be sufficiently flexed by bringing the leg off the end or side of the table.
In order to maintain the length of the fracture in the long-leg splint, care must be taken to provide a good supracondylar molding.
2. Splint application
Manual traction
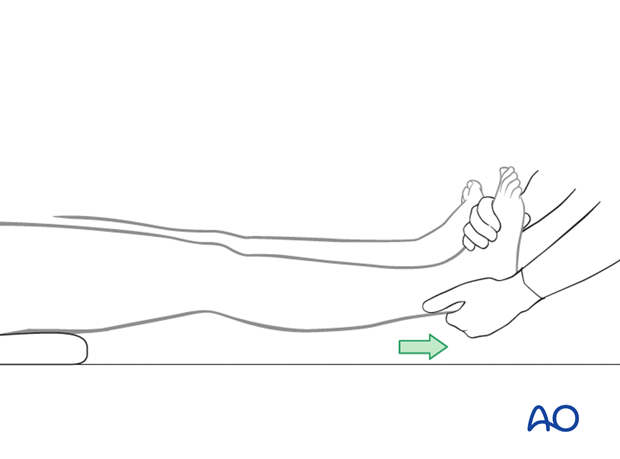
A preliminary reduction of the distal femoral fracture is performed. An assistant is needed to provide manual traction through the ankle while the splint is being applied.
Splint padding
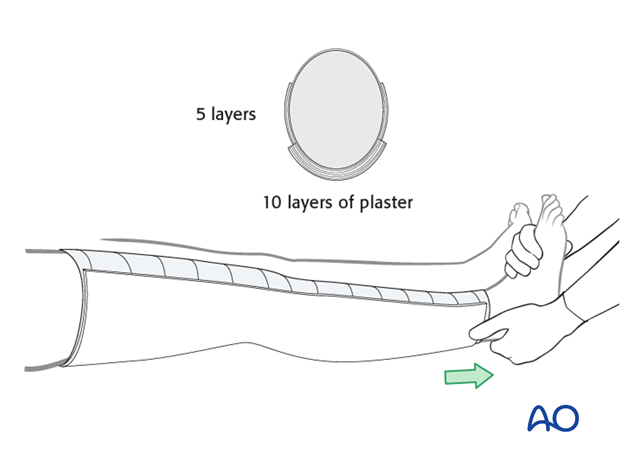
With the leg under manual traction and the knee flexed 20°, ample splint padding is placed around the leg. The padding starts at the supramalleolar region and extends up to the top of the thigh. It is important to make this several layers thick above the ankle and at the upper thigh to reduce the risk of pressure problems in these areas.
12.5 cm wide plaster slabs are used medially, laterally, and posteriorly. Medially and laterally, 5 layers of plaster are used. Posteriorly, 10 layers of plaster are used. The plaster is wetted, placed on the leg and then secured with additional cast padding and elastic bandages.
While the plaster is drying, supracondylar molding is performed and held until the splint material is hard.

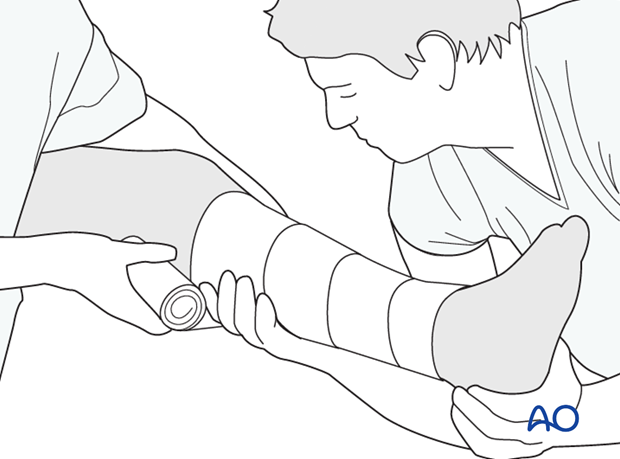
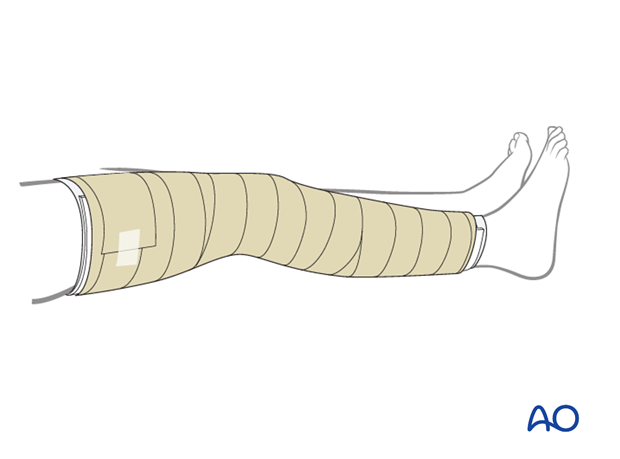
Elastic bandage
The elastic bandage should not be placed too tightly around the leg. The advantage of the non-circumferential splint is that it allows for swelling and it is therefore ideal during the early days following a fracture.
3. Aftercare
The splint is intended for provisional stabilization and can be used for up to 2-3 weeks. In general, it is taken off in the operating room before operative management. In the rare case of definitive nonoperative treatment, it can be converted to a long leg cast at 1-2 weeks, after the swelling has subsided.













