MIO - K-wire and screw fixation (joint-depression type)
1. Diagnosis
General indications for surgery
Some patients with fractures are obvious surgical candidates. Others present with medical contraindications to open surgery, or local soft-tissue contraindications to open surgery. Examples would be older diabetics, or medically unwell patients who have a significant calcaneal deformity but have a contraindication to a more invasive procedure.

Choice of treatment method
Younger patients in good health, good soft tissues with uncompromised healing potential and significantly displaced fractures have an undisputed indication to open reduction and internal fixation. At the other end of the spectrum are patients who have significant co-morbidities, or who are elderly, or who have risk factors, like smoking. These are considered to be too high a risk for a formal open reduction and internal fixation.
It is in this latter patient group that minimally invasive techniques are most useful.
Fracture indications for minimally invasive surgical techniques
When a fracture changes foot morphology, normal gait would be compromised, therefore surgery is indicated in order to restore normal anatomy and normal biomechanical relationships. Such restoration leads to normal gait.
If the fracture is extraarticular, absolutely anatomical reduction is not necessary because we are not dealing with an articular surface. In these situations, indirect reduction techniques and minimally invasive surgical stabilization methods can be used. One can employ these techniques also in patients in whom, under normal circumstances, an open reduction could be performed, but who are unwell, or have other risk factors which mitigate against full open surgery.
A basic principle is always to obtain accurate joint reductions. However, medical contraindications are of greater importance, as indicated by an infection rate in calcaneal fracture surgery upwards of 15% in diabetics, older unwell patients, or heavy smokers.
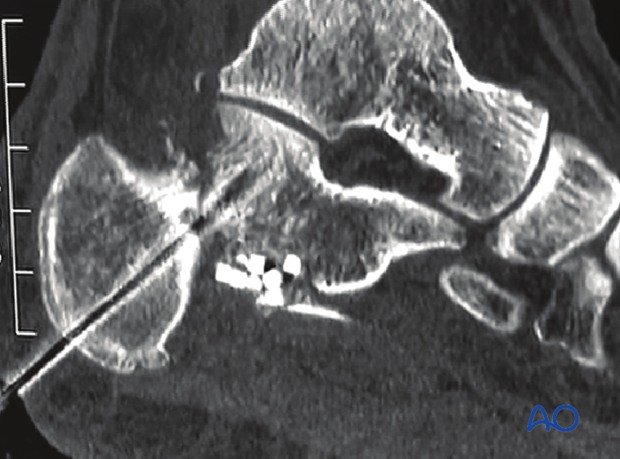
This image shows a CT with a joint-depression type fracture in which the posterior facet is one large fragment. This lends itself to an elevation of this single joint fragment (posterior facet) and then fixation is carried out by placing lag screws in the subchondral bone.

2. Approaches
For this procedure either the sinus tarsi approach or the minimally invasive lateral approach may be used.
3. Reduction
Preparation
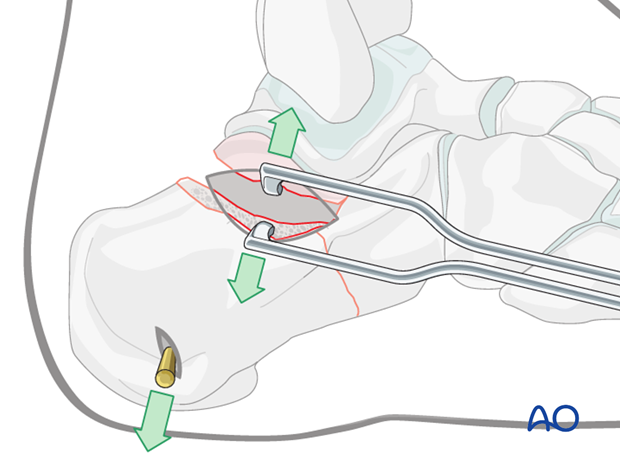
Under image intensification, with the patient in the lateral position, a large Steinmann pin is placed in the posterior calcaneal tuberosity. This will be used as a joystick for re-establishing calcaneal length.
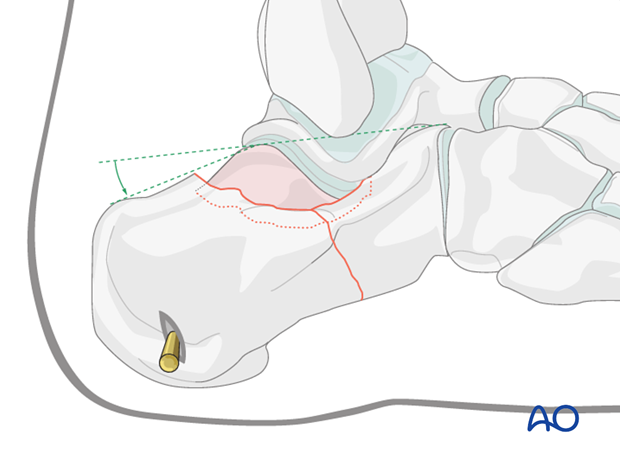
Elevate depression
A small incision is made under fluoroscopy centered on the fracture.
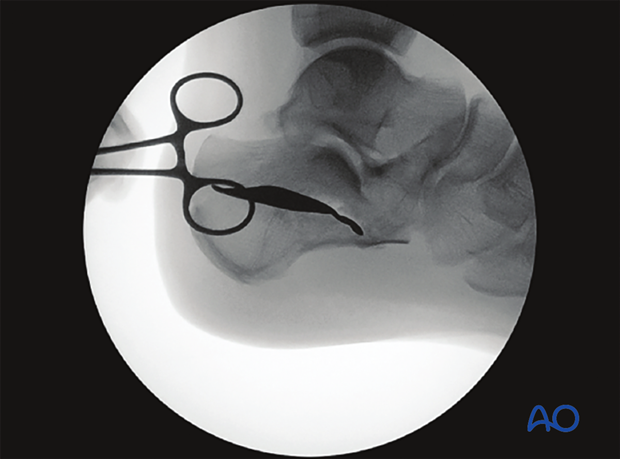
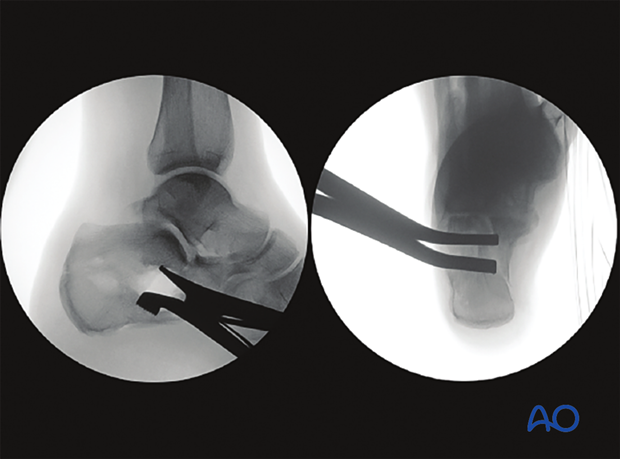
The x-ray shows the incision on patient’s foot for the sinus tarsi approach.
This will allow the surgeon to insert an elevator beneath the depressed fragment, lift it up and in this way restore joint congruity.
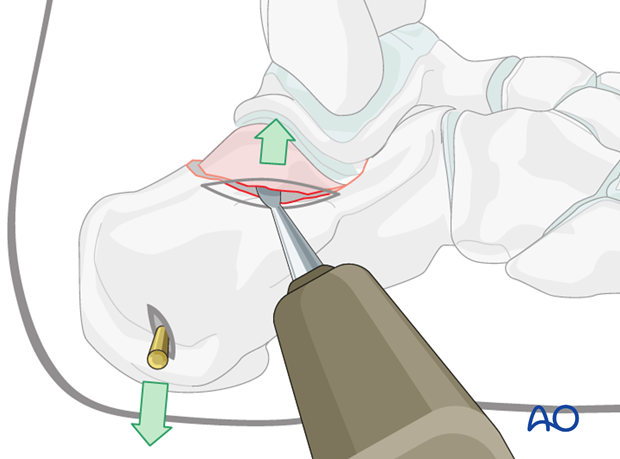
Maintenance of reduction
A lamina spreader can be very helpful. Careful examination under fluoroscopy establishes when the reduction is complete.
This x-ray shows a percutaneus reduction with small 3 cm incision to lift the posterior facet using a laminar spreader.
Wires or percutaneous screws can be used to maintain the calcaneal reduction.
The large bone defect may be filled with bone substitute which assists in maintaining the elevated fragment in position. It also helps to accelerate healing.
4. Fixation
K-wire fixation
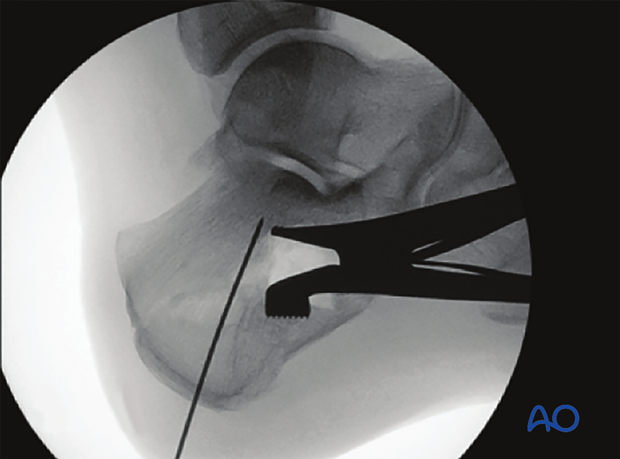
This postoperative image shows restoration of the Böhler’s angle. Note that the pin was placed from the posterior tuberosity into the posterior facet and bone substitute was used to fill the defect. One required only a 2 cm long incision through which the posterior facet was elevated and the bone substitute was inserted.
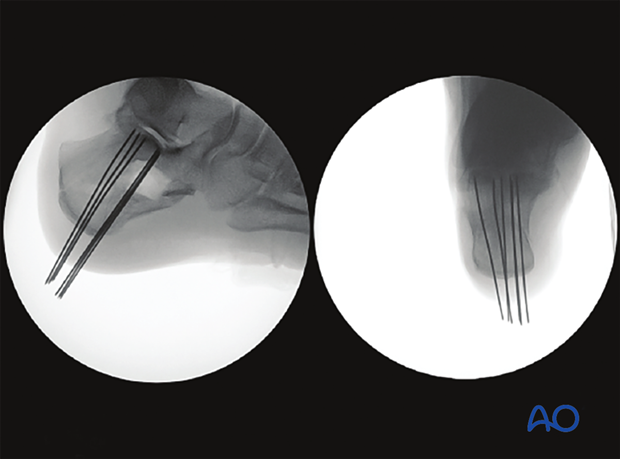
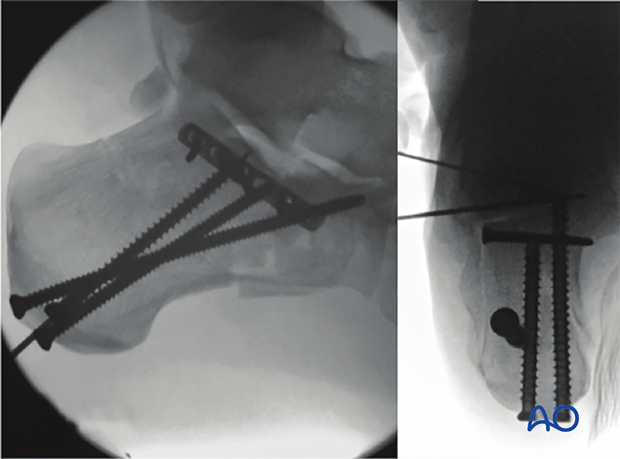
These images show in two views the reduced posterior facet with K-wire fixation.
Screw or plate fixation
As an alternative to K-wires percutaneous screws or plates can be used.
5. Aftertreatment
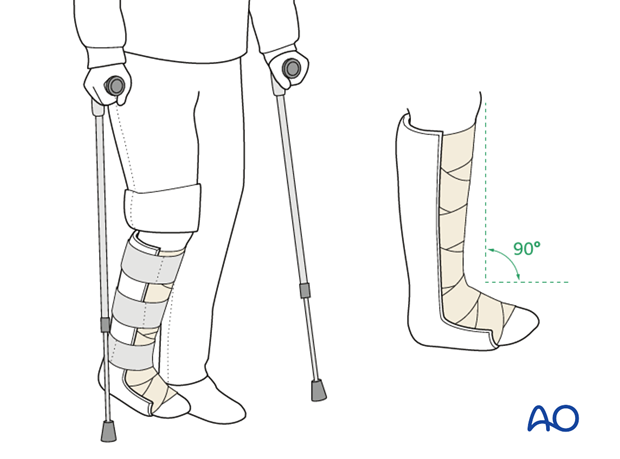
Initially, the patient’s foot and ankle are kept in a well-padded posterior splint that maintains the foot in a neutral position.
The leg should be elevated intermittently through the first number of weeks. The ankle joint is put through range-of-motion exercises as soon as possible, usually by 2-5 days. Normal bathing and washing prevents pin-track infections.
Pin removal is not before 6 weeks. Image at left shows pins at 6 weeks before removal.
Weight bearing is delayed until pin removal after 6 weeks.
Radiography including lateral and axial views is obtained at 6,12 and 26 weeks.














