Sinus tarsi approach to the calcaneus
1. Indications
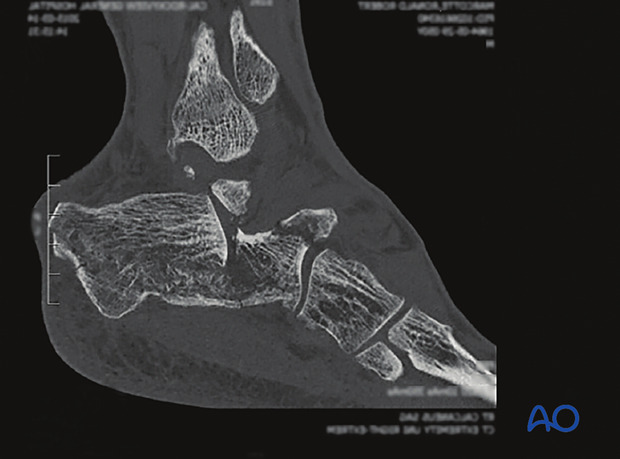
This approach is used for minimally invasive reductions and percutaneous fixation of displaced intraarticular calcaneal fractures. It is common for this approach to be undertaken when the calcaneal fracture is of a simpler classification.
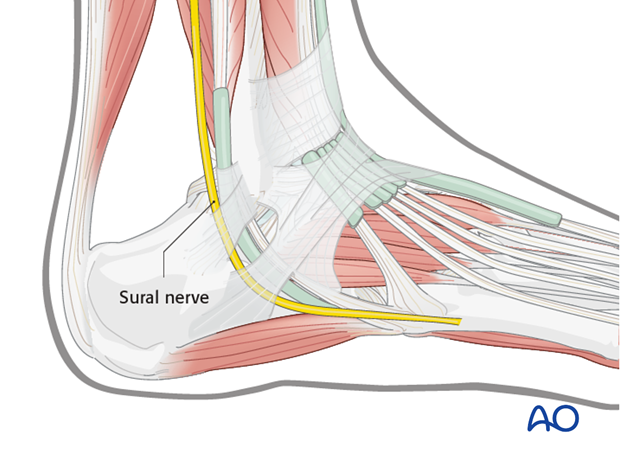
2. Anatomy
This approach is subfibular and slightly anterior and keeps the peroneal tendons inferiorly. This is a safe, simple incision, but the surgeon must look for the sural nerve.
The lateral calcaneal artery is responsible for the majority of the blood supply to this area.
This small incision is much safer than the extended L-incision. It is smaller and is not compromising any skin on the lateral side of the foot.
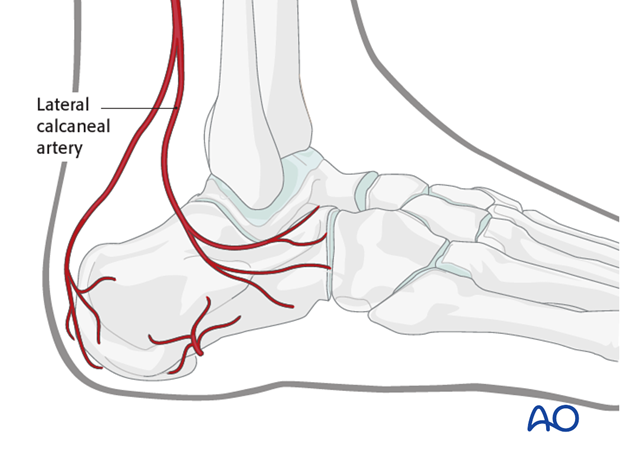
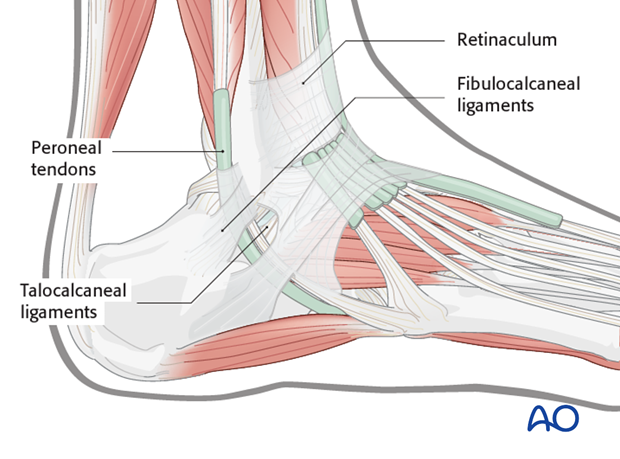
Ligaments and tendons
The peroneal tendons are on the lateral side of the calcaneus. Note the position of the retinaculum and of the fibulocalcaneal and talocalcaneal ligaments.
3. Timing of surgery
Correct timing of surgery is the most important factor in preventing local wound complication. Early surgery may be appropriate for percutaneous sinus tarsi reduction if foot swelling is not severe. But sometimes swelling precludes early surgery and great patience is required to optimize the local surgical environment.
Skin blisters should be observed and carefully protected.
The image shows a foot 3 days after serious trauma, which is inappropriate for surgery.

The return of skin wrinkles to the lateral side of the foot should be used as a guide for the timing of surgery. Generally, 2-5 days is the optimal time for percutaneous sinus tarsi surgery. Longer delays may be associated with increasing difficulty in obtaining a reduction and closing the surgical incision.
The image shows a foot 14 days after injury appropriate for surgery, with the “wrinkle sign” present.

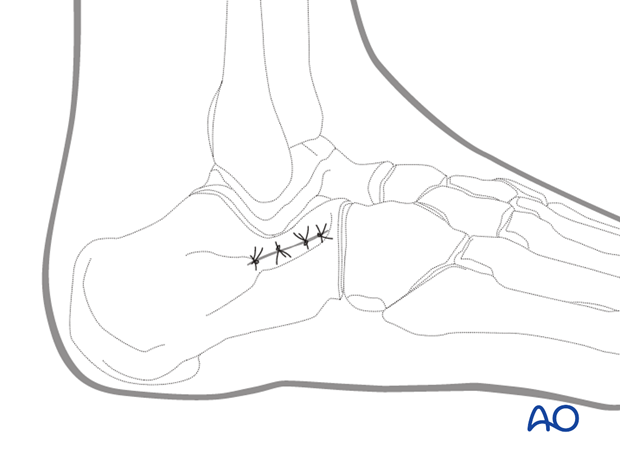
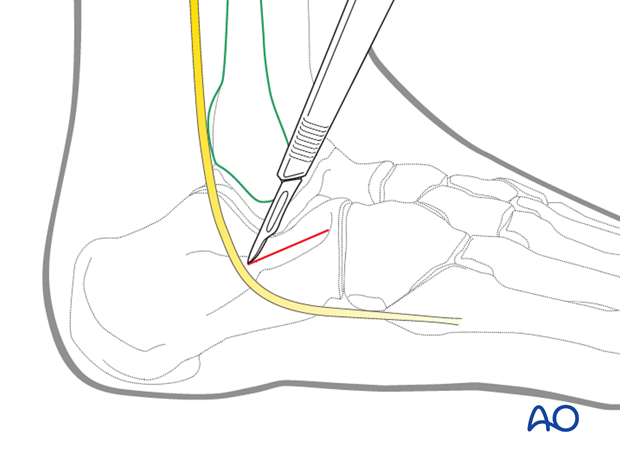
4. Incision
First the skin and then the peroneal retinaculum are incised. Tendons and sural nerve are protected inferiorly. Then the subtalar joint is found and entered.
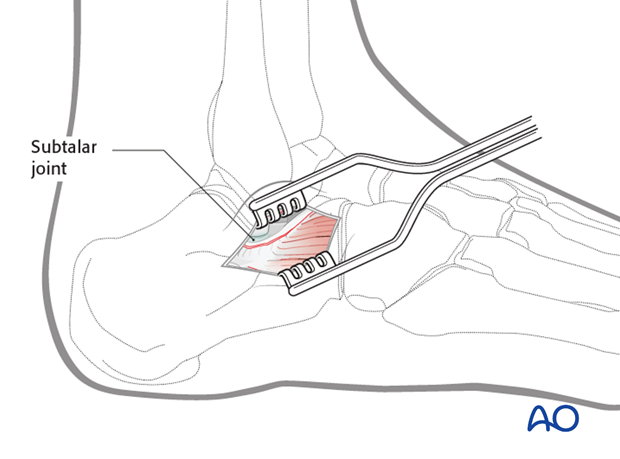
5. Approaching the joint
Once the subtalar joint is entered, this small incision allows the surgeon to have direct vision of the subtalar joint and the surgeon can reduce and internally fix any fracture lines.
Dry arthroscopy can also assist in accurate joint reduction.
6. Wound closure
This small wound is easily closed and has a very low infection rate.