Patient assessment and diagnosis
1. Introduction
After resuscitation and stabilization of the patient, acetabular specific factors which need to be clarified and identified are the sciatic nerve function and this should be recorded in all patients. Also, the condition of the skin and soft tissues must be assessed as abrasions, wounds and degloving injuries are common and may prevent the ideal surgical approach being performed initially or at all.
An associated hip dislocation should be considered an orthopedic emergency and requires prompt reduction.
For a complete overview of the secondary survey we direct you to the ATLS® courses and manual.
Emergency care for acetabular fractures should be available and preplanned at every trauma hospital. Most patients with acetabular fractures will need to be referred to a specialized center. Ideally surgery will be performed as soon as possible and ideally between day 3 and 7 after injury. So, if a secondary transfer is required this should be made promptly.
2. Physical examination
If the patient is conscious, ask about discomfort or pain in the pelvic area.
The patient is visually inspected to identify:
- Wounds
- Deformity
- Swelling
- Bruising
In case of open fractures, antibiotic administration should begin immediately.
Degloving injuries are common.
Contusions and abrasions in the area of the greater trochanter or iliac crest may herald the presence of a Morel-Lavallée lesion. This is an area of degloved skin with fluctuance due to a large underlying hematoma and fat necrosis. Although technically a closed injury, secondary bacterial contamination is common and surgical debridement and drainage is needed before definitive fracture care.
3. Neurological examination
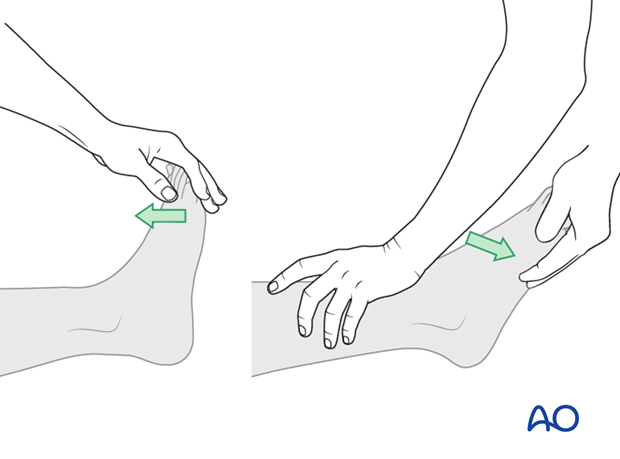
The incidence of sciatic nerve compromise detected preoperatively ranges from 12–38%. Because the peroneal division is most at risk, foot dorsiflexion and eversion should be tested and recorded in the medical records both before and after surgery.
Check long toe extensors (L5) and ankle plantar flexors (S1).
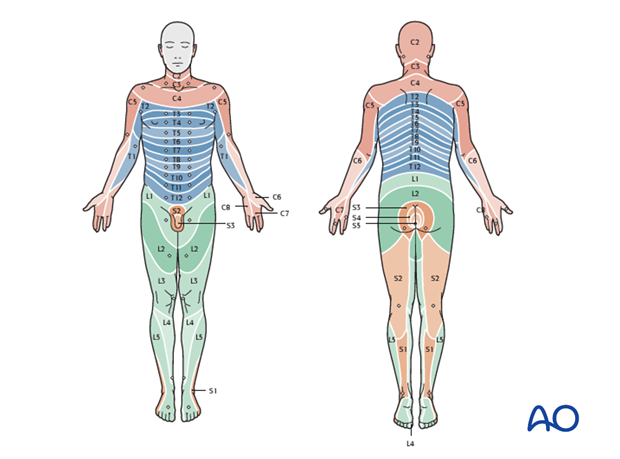
Key sensory points
The sciatic nerve sensation should be assessed and documented to be absent, abnormal, or normal.
4. Radiologic examination
Most patients sustaining an acetabular fracture will have the injury identified on a CT scan.
Plain films remain extremely useful as 2-D images will be used during the surgery.
A summary of the radiologic examination is given below. For more information about radiologic landmarks and interpretation of images and identification of fracture lines see Radiology of the intact acetabulum.
AP view of the involved hip
The six fundamental radiographic landmarks of Letournel:
- Posterior wall of the acetabulum
- Anterior wall of the acetabulum
- Roof (dome or tectum)
- Teardrop
- Ilioischial line (posterior column)
- Iliopectineal line (anterior column)
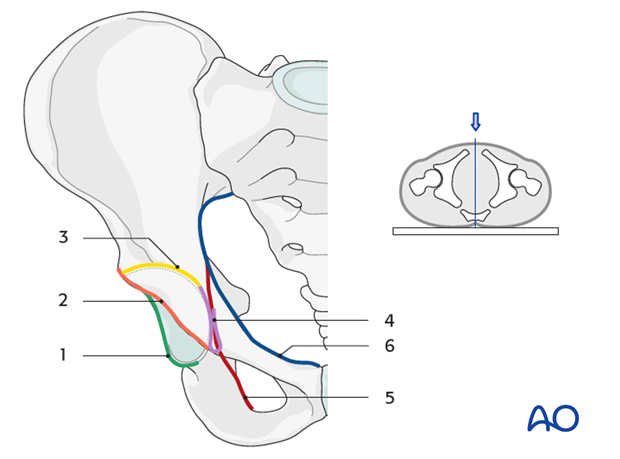
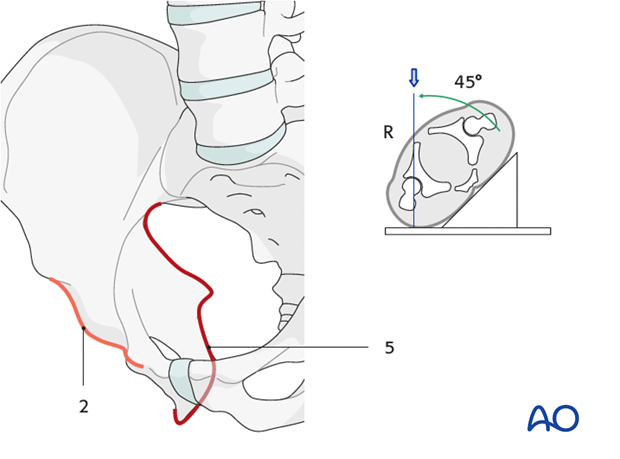
Iliac oblique view
It is useful to assess the posterior column and anterior wall. The patient is rolled 45° toward the injured side. This provides a view of the iliac wing and a profile of the obturator ring.
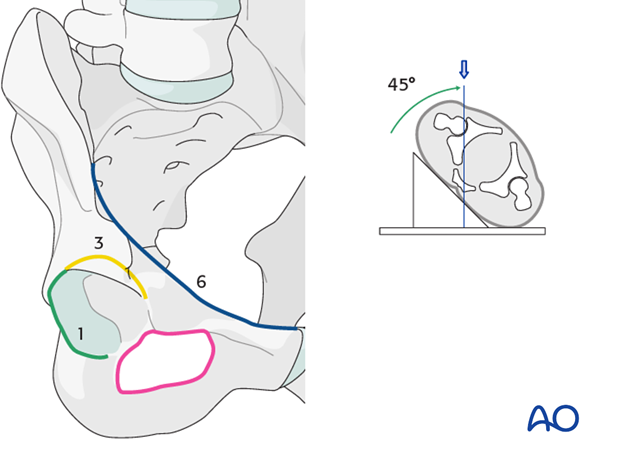
Obturator oblique view
It is useful to assess the obturator ring, anterior column, and posterior wall. The pelvis is rotated 45° toward the uninjured side, providing a view of the obturator ring (purple), and a profile of the iliac wing.
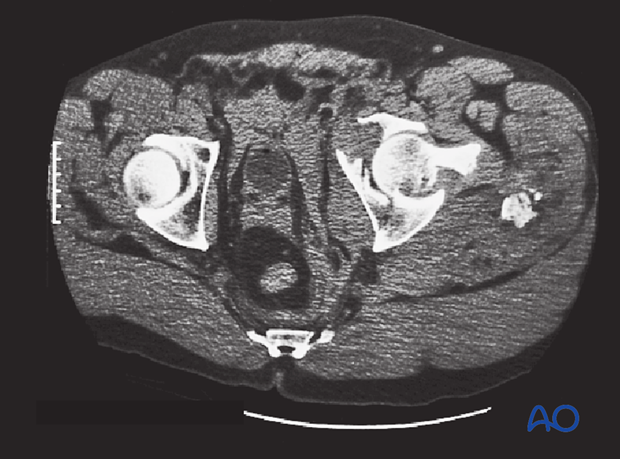
CT imaging
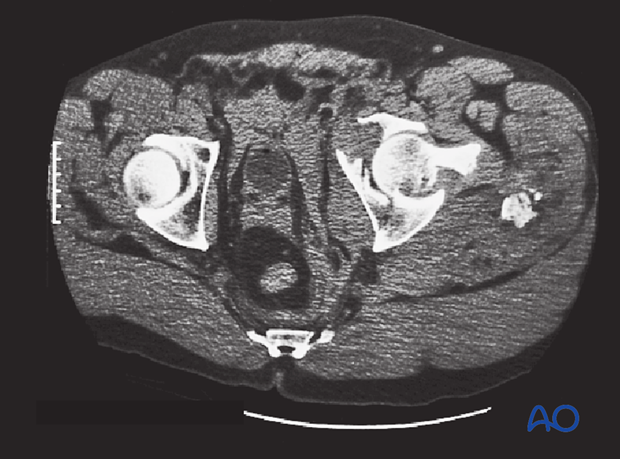
Axial and 3-D CT are now routinely obtained in all patients and improve understanding of the injury. They are especially useful in measuring articular comminution and step off, the size and number of posterior wall fragments, marginal impaction, rotation and displacement of the columns, and the presence of intraarticular fragments or femoral head fractures. A CT scan can also identify injuries to the posterior aspect of the pelvis, such as SI joint disruption or a sacral fracture.
This example shows a severe nonreduced acetabular fracture.
5. Diagnosing the fracture classification
A complete understanding of fracture line orientation is essential for preoperative planning, reduction maneuvers and proper placement of implants during surgery. Therefore, a proper radiologic examination is mandatory.
A summary of diagnosing the fracture classification is presented below. For more information refer to Radiology of the intact acetabulum and the diagnosis section of each fracture type.
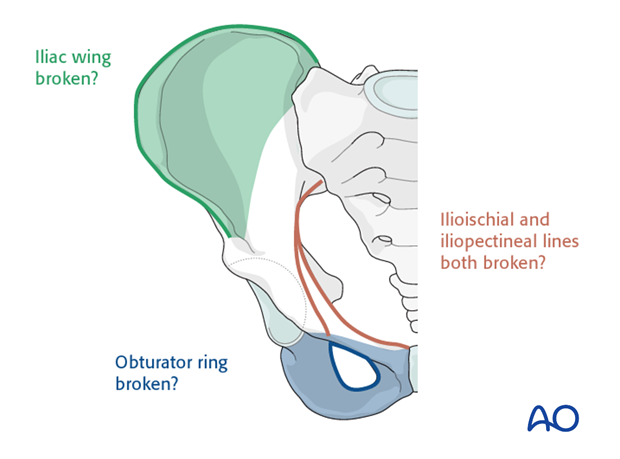
Diagnosis based on plain radiographs
By inspecting the three principal plain radiographic views, one can easily identify the fracture pattern in answering the following questions:
Is the iliac wing broken? (green area)
Inspect the obturator oblique view. If yes:
- Both column
- Anterior column
- Anterior column/posterior hemitransverse
Is the obturator ring broken? (blue area)
Inspect the obturator oblique view. If yes:
- Both column
- Posterior column ± posterior wall
- T-type
Note: Anterior column and associated fractures show fractures of the obturator ring at the superior pubic ramus only.
Are the ilioischial and iliopectineal lines both broken? (brown lines)
Inspect both oblique views. If yes:
- Both column
- T-type
- Anterior column/posterior hemitransverse
- Transverse ± posterior wall
Wall fractures
Posterior wall fractures may be associated with the transverse and posterior column fractures in the classification and additionally are often found in both column and T-type fractures.
Anterior wall fractures are rare.
Supplementary criteria
- An anterior fracture line in the obturator oblique view will distinguish the T-type from the posterior column fractures.
- A crossing posterior fracture line in the iliac oblique view will distinguish the anterior column/posterior hemitransverse from the anterior column fracture.
- Transverse fractures show neither iliac wing nor obturator ring fractures.
- Both column fractures will show a spur sign in the obturator oblique view.
Diagnosis based on CT images
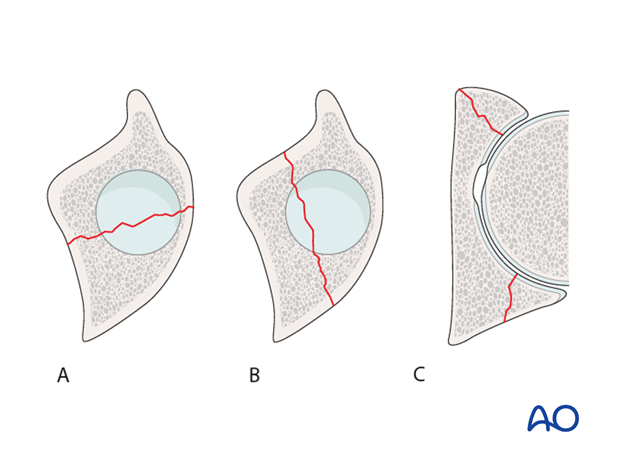
The axial CT plane image on the level of the fracture reveals whether …
… the fracture is:
- A column fracture (A)
- Transverse fracture (B)
- Wall fractures (C, both wall fractures shown)
The column fracture runs from medial to lateral, the transverse fracture runs from anterior to posterior, and the wall fracture is oblique.