ORIF through modified Stoppa approach
1. General considerations
Sequence of the treatment
In anterior column/posterior hemitransverse fractures with modified Stoppa approach, the following surgical sequence is common:
- Joint distraction and removal of incarcerated fragments
- Reduction of femoral head dislocation if not achieved closed on admission
- Reduction
- Assessment of reduction (both the anterior column and posterior hemitransverse reduction is direct)
- Fixation of the anterior column
- Fixation of the hemitransverse fracture
Planning/templating
Preoperative templating is essential for understanding the complexity of an acetabular fracture.
When using implants on the innominate bone, it is important to know the best starting points for obtaining optimal screw anchorage (see General stabilization principles and screw directions).
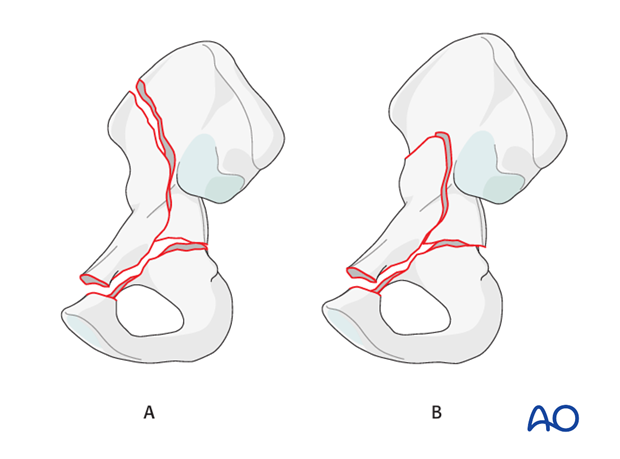
Approach windows
Many fractures can be treated with use of the Stoppa window only. The lateral window may supplement this.
Fractures with low and intermediate anterior column elements will only require a Stoppa window (B).
Only high anterior column fractures (A) may benefit from a lateral window to allow control of the iliac crest and supplemental fixation.
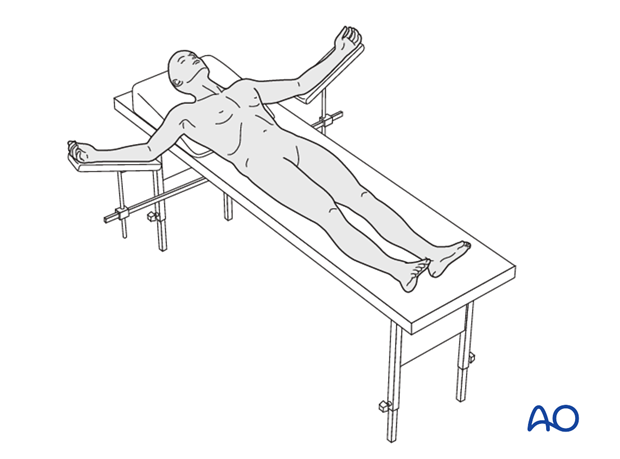
Patient positioning
This procedure is normally performed with the patient in a supine position.
2. Principles of reduction
Open fracture reduction
The Stoppa approach allows direct control of the anterior column around the acetabulum and it is often possible to control the reduction entirely at the level of the pelvic brim. This may enable the lateral window to become unnecessary and the approach limited to the Stoppa window only.
The Stoppa approach allows better visualization and control of the posterior column than the ilioinguinal approach, such that the hemitransverse fracture can be reduced and stabilized directly.
Indirect visualization
Unusually for a significant joint, articular reduction of acetabular fractures is indirect. The articular surface of the hip joint is not seen directly. Reduction must be assessed by the appearance of the extraarticular fracture lines and intraoperative fluoroscopic assessment. Some fracture lines are palpated manually but not seen directly such as transverse fracture lines on the quadrilateral plate.
Quality of reduction
Posttraumatic arthrosis is directly related to the quality of reduction - the better the reduction, the greater the chance of a good or excellent result.
3. Joint distraction
Application of traction
It is important to ensure hip flexion to allow enhanced exposure of the iliac fossa and true pelvis.
The anterior column/posterior hemitransverse fracture is a result of medial displacement of the femoral head at the time of injury. In order to allow manipulation of the anterior column element, the femoral head must be distracted. This is typically accomplished with the application of lateral and/or distal traction.
It may be successful to push the femoral head out of the pelvis using a ball spike pusher.
Otherwise this may be accomplished with the application of lateral or distal traction.
In some surgeon’s experience, the use of a traction table post or other traction frame is helpful during this operation.
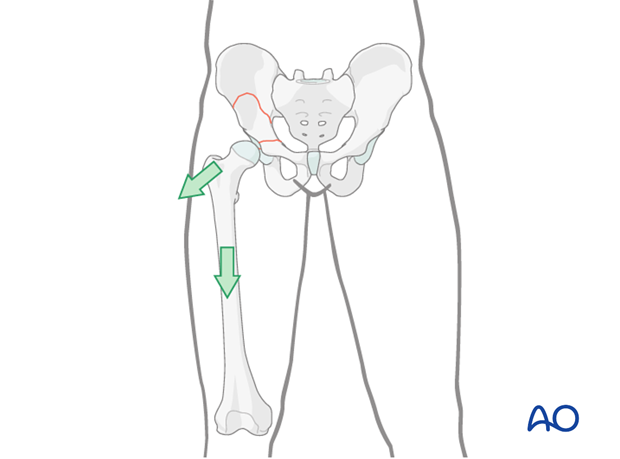
Center the femoral head under the radiological roof using a combination of lateral traction, distal/longitudinal traction, and limb positioning.
Verify the femoral head reduction with the image intensifier.
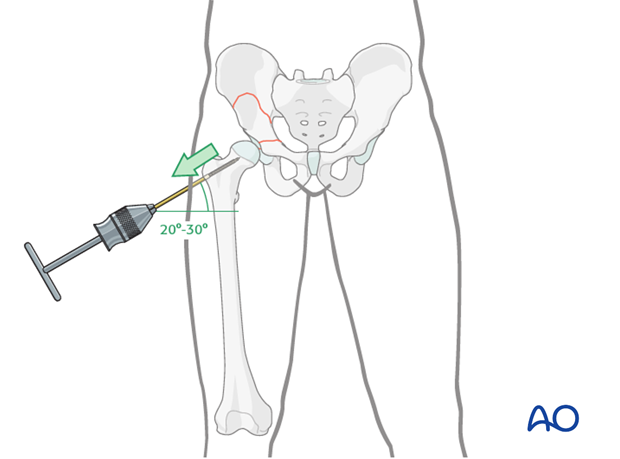
Lateral traction with a trochanter screw
Traction may be applied through a Schanz screw in the greater trochanter, manually or attached to a fracture table.
Insert the screw along the axis of the femoral neck, through a short, separate incision over the greater trochanter.
Distal/longitudinal traction
Distal or longitudinal traction may be applied in the axis of the femur. This can be accomplished manually via a distal femoral traction pin or via a fracture table.
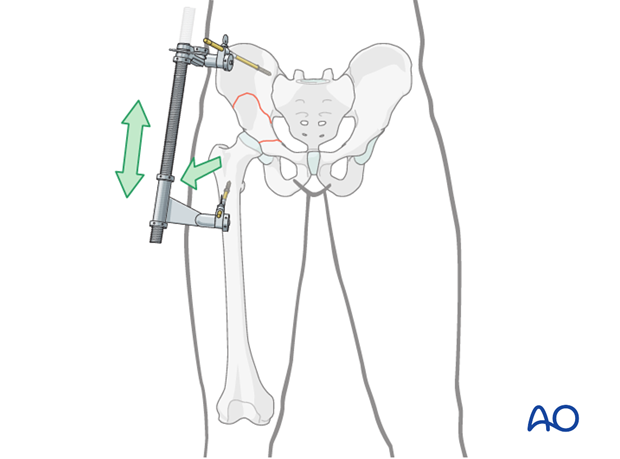
Alternatively, a large distractor may be applied using the following technique.
Insert the proximal 5 mm Schanz screw in the sciatic buttress placed from anterior to posterior. This screw must be cranial to the fracture and into an intact segment of the innominate bone. Based on the fracture through the ilium, this screw may not be possible in high anterior column fractures.
Place the distal Schanz screw into the femur at the level of the lesser trochanter from anterior to posterior. Attach the distractor as shown to these two screws.
Teaching video
AO teaching video: Use of the distractor on the pelvis
4. Cleaning of the fracture site
Fracture sites are prepared by preliminarily increasing the displacement and then removing early callus and granulation tissue.
Joint distraction is extremely useful to facilitate this debridement.
5. Anterior column: reduction and fixation
Fixation with a pelvic brim plate
A contoured pelvic brim plate is used through the Stoppa approach. This plate can be contoured as required by the specific fracture.
The plate must be long enough to provide adequate fixation above and below the acetabulum. This typically requires extension to the pubic body.
It is likely that the application of the plate will facilitate some or all of the reduction.
Contouring the plate
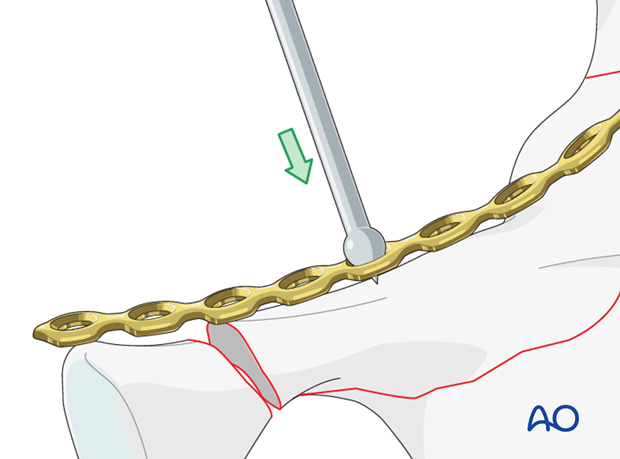
Contour the plate to fit the anterior column in advance of the reduction.
The use of a malleable template aids plate contouring.
Because the primary purpose of this plate is to buttress the anterior column, posterior contouring is most critical. For this reason, plate fixation normally starts posteriorly and proceeds anteriorly. Final adjustment of the plate profile can be achieved in situ, due to plate malleability.
Tools for in situ plate contouring include the ball spike for pushing, ...
... and large and small fragment screwdrivers for torsional adjustment.
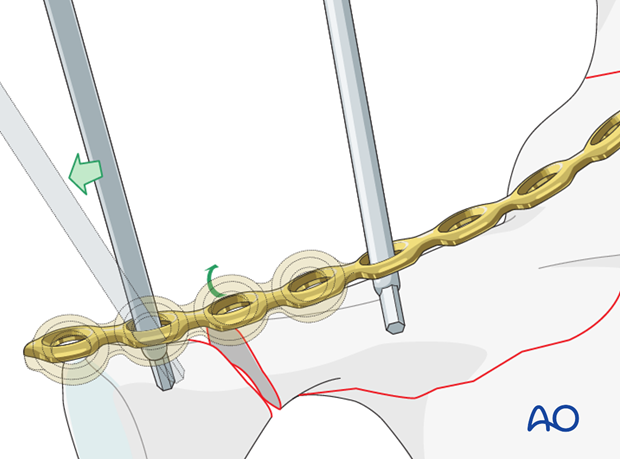
Plate fixation of the anterior column
The plate is positioned in the medial iliac fossa adjacent to the SI joint. The cranial screw is placed proximal to the fracture in an anterior to posterior direction parallel to the SI joint, and typically measures 40 mm in length. The screw drives the plate down and buttresses the elevated anterior column fragment, completing the reduction.
The next two screws may have the proximal cortex overdrilled with a 4.5 mm drill if further compression of the fracture is required.
Care should be taken to avoid inadvertent violation of the SI joint.
The proximal fixation is typically shorter than with an ilioinguinal approach and the fixation includes screws through the proximal part of the fracture.
The interfragmentary screws applied through the plate ensure compression of the fracture and provide additional stability above the acetabulum. Care should be taken to ensure that each screw is placed extraarticularly, as this region is juxtaarticular.
Fixation of high anterior column fractures
High fractures will be adequately controlled by the fixation at the pelvic brim. It may be necessary to supplement this with the addition of a lateral window.
With an approach through a small lateral window, direct reduction and screw or plate fixation can be completed.
6. Posterior column: reduction
Fracture reduction
This element is often undisplaced and little reduction is required.
If required, preliminary reduction is normally achieved by ligamentotaxis with distal and lateral traction through the femur. This can be augmented by placement of a small bone hook in the lesser sciatic notch. The hook can be used to laterally and anteriorly reduce the posterior column.
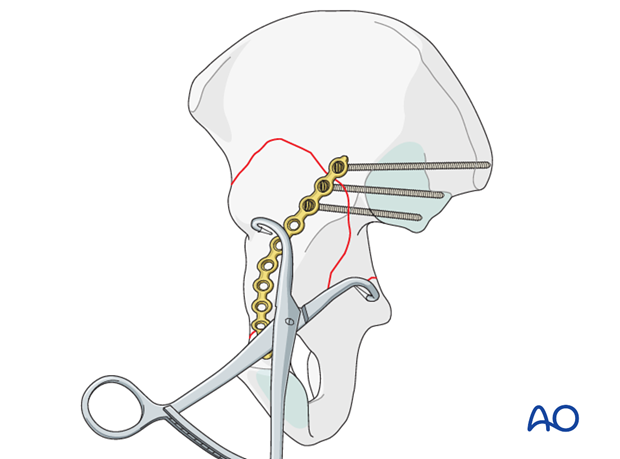
Offset quadrangular clamp
The most common reduction maneuver of the posterior column element is the use of the quadrangular clamp.
This clamp is applied with the short arm over the pelvic brim, and the second deep arm applied to the displaced posterior column along the quadrilateral surface.
Care must be taken to avoid excessive pressure on the vessels by the clamp or force of retraction.
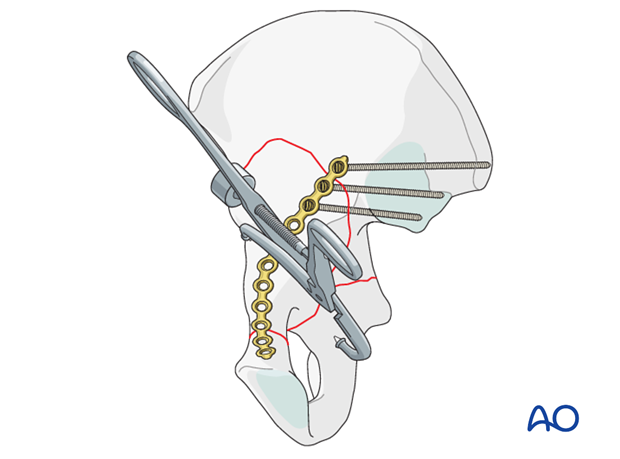
Use of pointed reduction forceps
The most direct technique uses pointed reduction forceps (or Weber clamp) which spans from the pelvic brim to the quadrilateral surface portion of the posterior column.
Completion of the anterior column plate
After reduction, the plate can be secured inferiorly to the pubic ramus and the body of the pubis. Distal fixation becomes increasingly important in lower fractures.
7. Posterior column: fixation
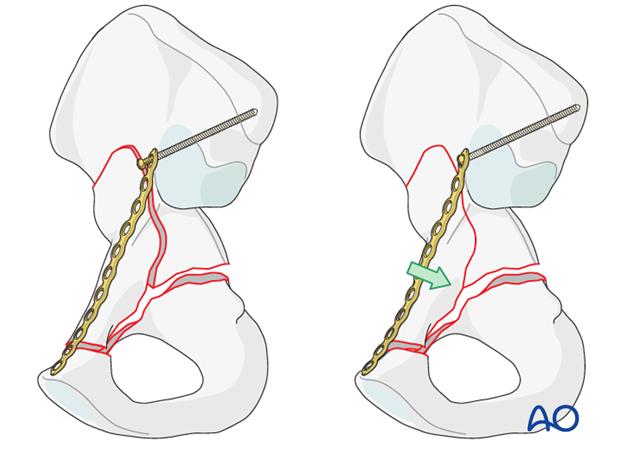
Anterior to posterior screw fixation
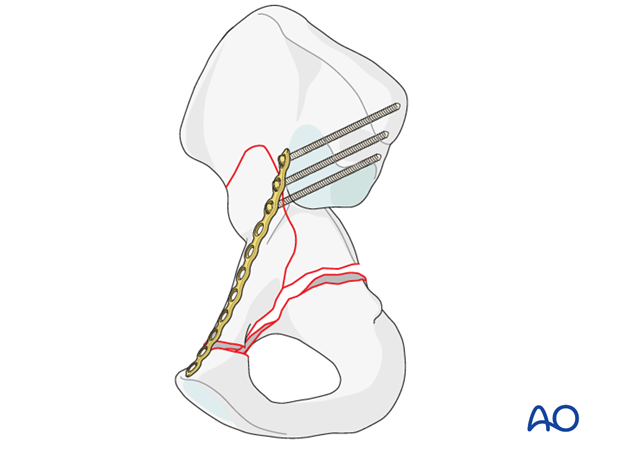
Posterior column element fixation relies primarily on screws placed from the anterior column directed posteriorly.
The posterior column fixation is placed through the pelvic brim plate. The most posterior screw (ca 80 mm) is directed toward the ischial spine. It is usually possible to place a second screw (ca 100 mm) in the next anterior plate hole, directed toward the ischial tuberosity.
Regardless of configuration, it is important that at least two screws be used for the posterior column fixation. A single screw does not provide sufficient torsional stability.
The construct is completed with the most anterior screws in the body.
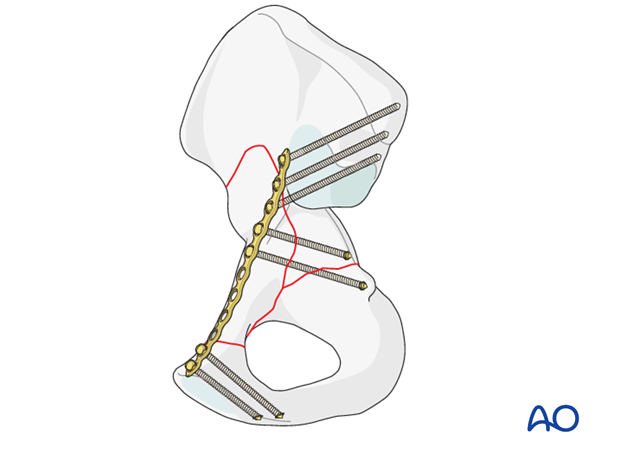
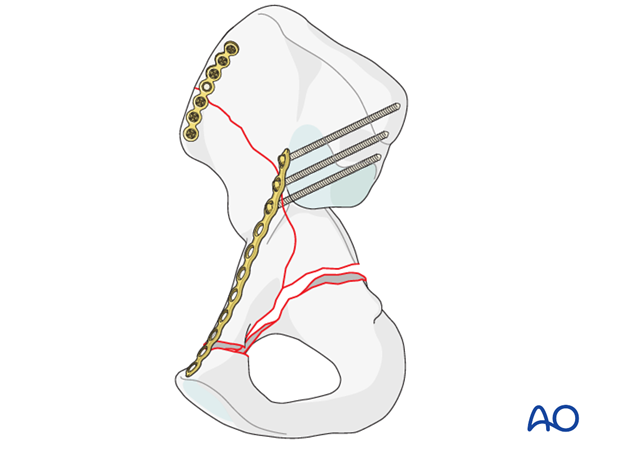
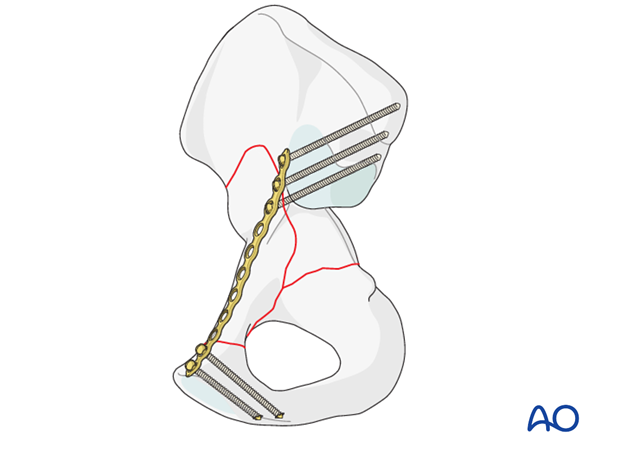
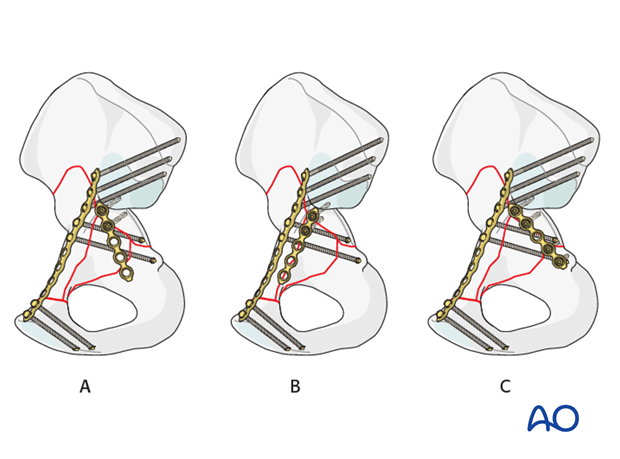
Option: stabilization of quadrilateral surface and/or posterior column with an infrapectineal plate
A plate can be placed on the quadrilateral surface to buttress comminution or to stabilize the posterior column.
This plate is placed under direct visualization.
There are multiple plating options available. Utilizing 3.5 mm reconstructive plates undercontoured to provide a buttressing effect; these plates can be oriented either down the posterior column (A), or down the anterior column towards the pubic ramus (B).
Such a plate is typically fixed into the dense bone in the sciatic buttress just anterior to the SI joint. The obturator oblique radiograph can be helpful to ensure that these screws are extraarticular.
Inferiorly the posterior column can be stabilized with two screws under direct vision of the Stoppa window (C).
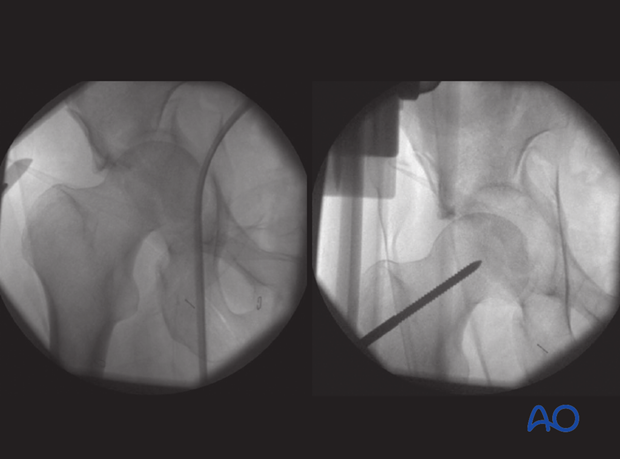
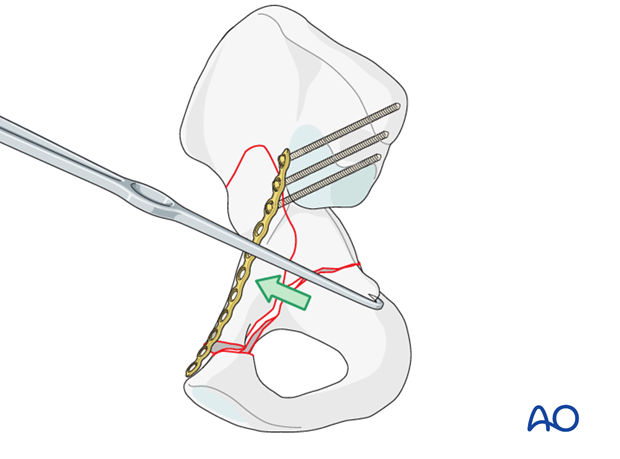
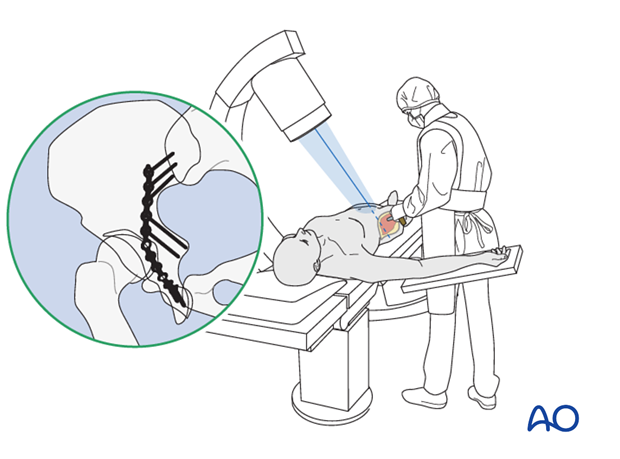
Fluoroscopic navigation of the posterior column screw placement
The iliac oblique view can be used to position the anterior to posterior screws. With the C-arm rolled away from the surgeon 45°, the posterior column is well visualized and the access unobstructed.
The drill can be advanced down the posterior column under fluoroscopic guidance, ensuring an extraarticular position as shown in the image. The screw can then be placed in the same tract.
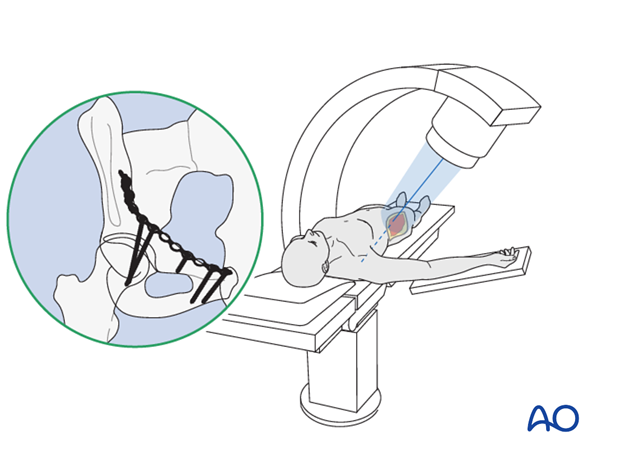
The obturator oblique view can be used to confirm appropriate placement. The projection of the screw should aim at the ischium. The most common mistake is to drive the screw in the direction of the posterior wall.
Screws that penetrate the posterior column cortex may injure the sciatic nerve.
Because this view is obtained with the C-arm rolled in the direction of the surgeon, access to the acetabulum is obstructed. This view is therefore used as confirmation and difficult to use for real time navigation.
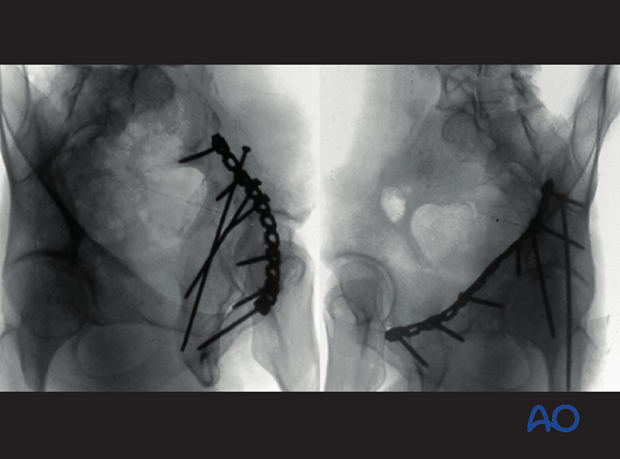
8. Final radiographic assessment
Once all fixation is in place, confirm the appropriate appearance of AP, obturator oblique and iliac oblique views and check the location of any screw that is placed near the hip joint.
Postoperatively, obtain formal high-quality radiographs of AP and both oblique views.
9. Postoperative care
During the first 24-48 hours, antibiotics are administered intravenously, according to hospital prophylaxis protocol. In order to avoid heterotopic ossification in high-risk patients, the use of indomethacin or single low dose radiation should be considered. Every patient needs DVT treatment. There is no universal protocol, but 6 weeks of anticoagulation is a common strategy.
Wound drains are rarely used. Local protocols should be followed if used, aiming to remove the drain as soon as possible and balancing output with infection risk.
Specialized therapy input is essential.
Follow up
X-rays are taken for immediate postoperative control, and at 8 weeks prior to full weight bearing.
Postoperative CT scans are used routinely in some units, and only obtained if there are concerns regarding the quality of reduction or intraarticular hardware in others.
With satisfactory healing, sutures are removed around 10-14 days after surgery.
Mobilization
Early mobilization should be stressed and patients encouraged to sit up within the first 24-48 hours following surgery.
Mobilization touch weight bearing for 8 weeks is advised.
Weight bearing
The patient should remain on crutches touch weight bearing (up to 20 kg) for 8 weeks. This is preferable to complete non-weight bearing because forces across the hip joint are higher when the leg is held off the floor. Weight bearing can be progressively increased to full weight after 8 weeks.
With osteoporotic bone or comminuted fractures, delay until 12 weeks may be considered.
Implant removal
Generally, implants are left in situ indefinitely. For acute infections with stable fixation, implants should usually be retained until the fracture is healed. Typically, by then a treated acute infection has become quiescent. Should it recur, hardware removal may help prevent further recurrences. Remember that a recurrent infection may involve the hip joint, which must be assessed in such patients with arthrocentesis. For patients with a history of wound infection who become candidates for total hip replacement, a two-stage reconstruction may be appropriate.
Sciatic nerve palsy
Posterior hip dislocation associated with posterior wall, posterior column, transverse, and T-shaped fractures can be associated with sciatic nerve palsy. At the time of surgical exploration, it is very rare to find a completely disrupted nerve and there are no treatment options beyond fracture reduction, hip stabilization and hemostasis. Neurologic recovery may take up to 2 years. Peroneal division involvement is more common than tibial. Sensory recovery precedes motor recovery and it is not unusual to see clinical improvement in the setting of grossly abnormal electrodiagnostic findings.













