Cranialization
1. Introduction
Severe injuries which result in disruption of greater than 25% of the posterior table should be considered for cranialization. This involves exposure of the entire sinus, meticulous removal of all sinus mucosa, and removal of the posterior table bone. The anterior table bone is replaced to reconstitute the forehead contour.
Important: Complete removal of the posterior wall and obstruction of the sinus outflow tract is essential to create a "safe sinus".
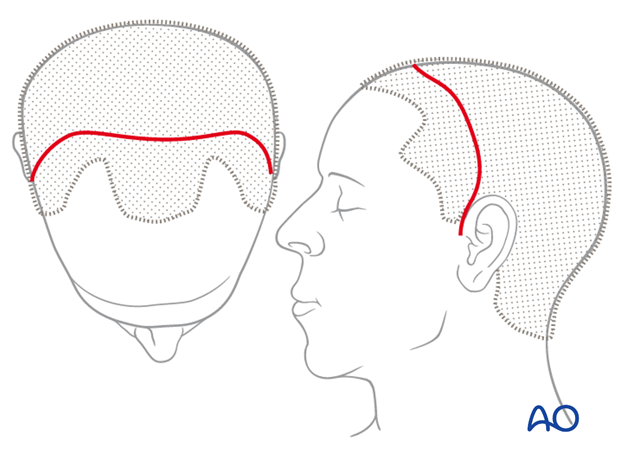
2. Approach
For this procedure the coronal approach is normally used. However, if present, lacerations can be used to directly access fracture sites for fracture managment.
3. Exposure
While elevating the coronal flap, it is critical to maintain the integrity of the pericranial flap. It may be necessary for repair of dural lacerations.

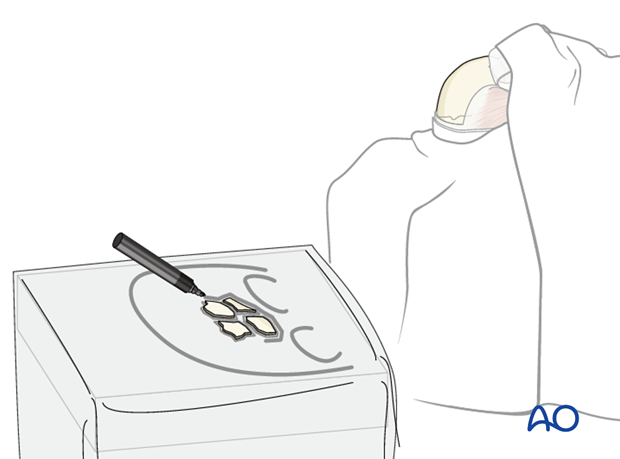
Pearl: identification of explanted bone fragments
Final orientation of any removed bone fragments can be challenging. Placing the explanted segments on a rough sketch of the skull made with a sterile pen will maintain orientation until re-implantation. Outline each segment and the overall shape of the defect.
The bone fragments should be kept moist until they are re-placed.
4. Defining the sinus margin
The margins of the frontal sinus are irregular and may not be visible through the fracture.
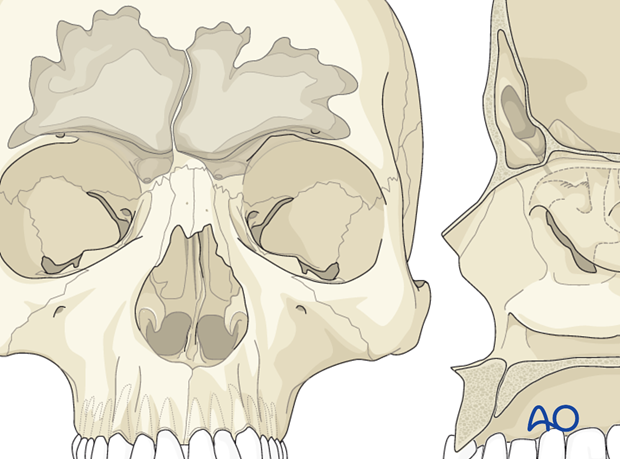
It is however critical to determine the precise margins of the sinus to allow for an accurate osteotomy and complete exposure of the sinus. There are several ways to accomplish this:
- Bayonet forceps
- Transillumination
- 6-foot (1.83 m) Caldwell x-ray with coin reference
- Intraoperative navigation
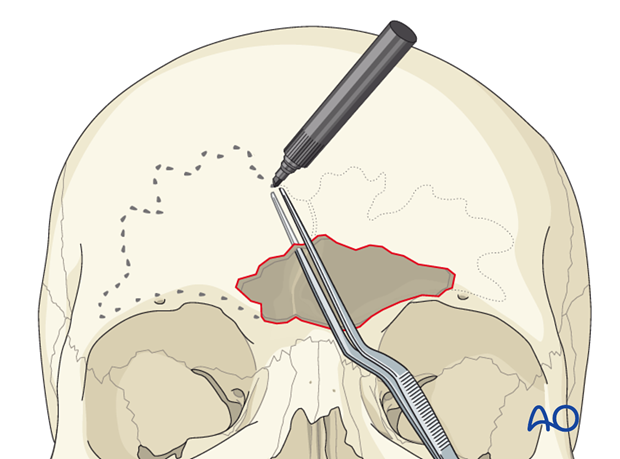
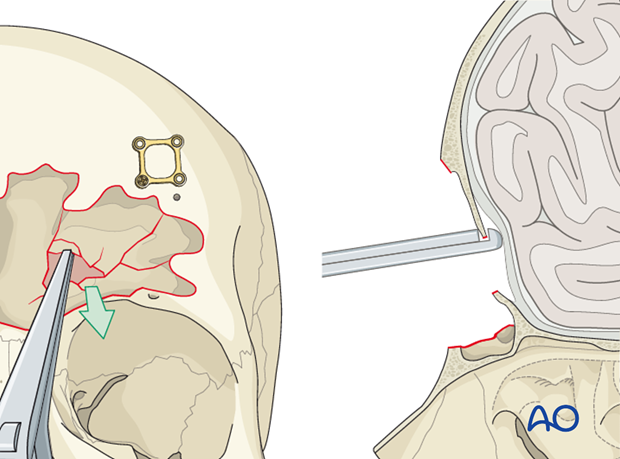
Bayonet forceps
One tine of the bayonet forceps (or bipolar cautery) can be inserted into the defect. The other tine spans the anterior table. The internal tine is then “walked” around the periphery of the sinus. The external tine is then used to guide markings which will outline the periphery of the sinus on the outer table bone. The outline can be marked with ink or electrocautery (the electrocautery should be placed at a low setting to coagulate overlying blood and avoid excessive bone injury).
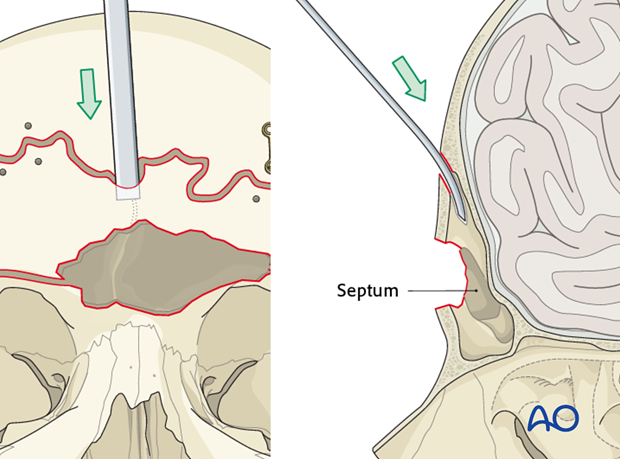
Transillumination
Alternatively, a light source (such as an endoscope) can be inserted through the anterior table bone defect. The light will transilluminate the sinus and delineate its margins.
Beware of pitfalls such as soft-tissue and blood present in the sinus.

6-foot (1.83 m) Caldwell x-ray with coin reference
A 6-foot (1.83 m) Caldwell x-ray with (anterior-posterior Caldwell x-ray with the patient placed 6 feet from the x-ray tube) can be used to delineate the margins of the sinus. The 6-foot penny Caldwell generates a “life-size” representation of the sinus cavity. It is imperative that the orientation (ie, right and left) is clearly documented on the x-ray.
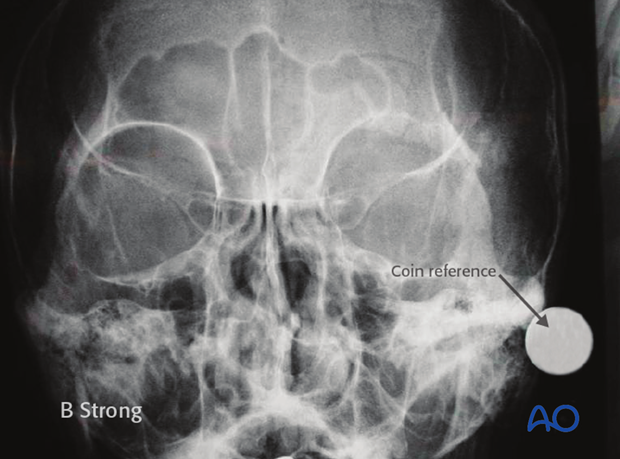
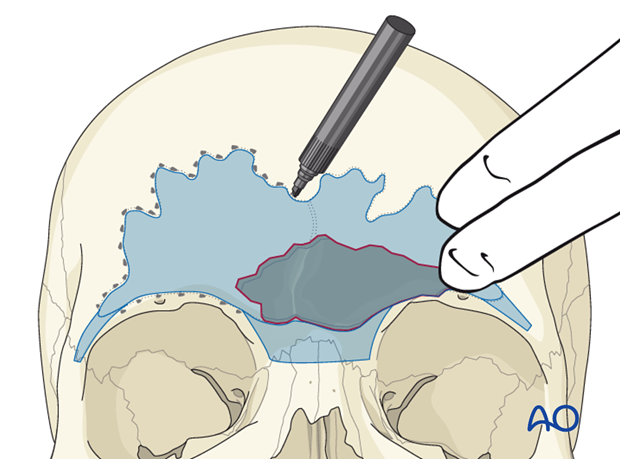
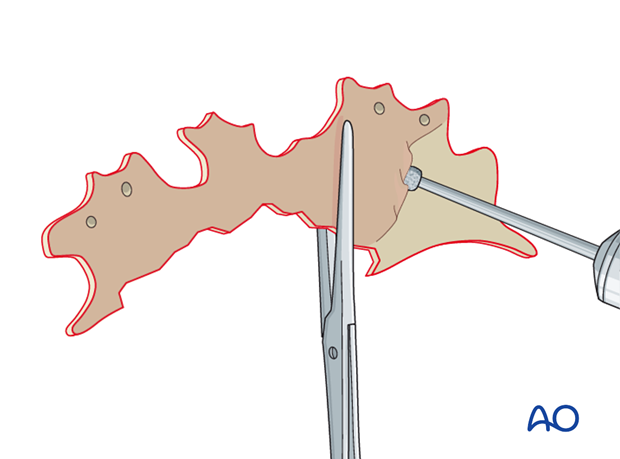
Scissors are then used to cut along the margins of the sinus. Lateral “wings” that project along the orbital rims are also cut out to help with orientation. A second copy of the sinus template is generated from the first in case one is contaminated during the procedure. An “R” is scratched into the right side of both templates to record orientation. Both copies are sterilized and brought onto the surgical field.
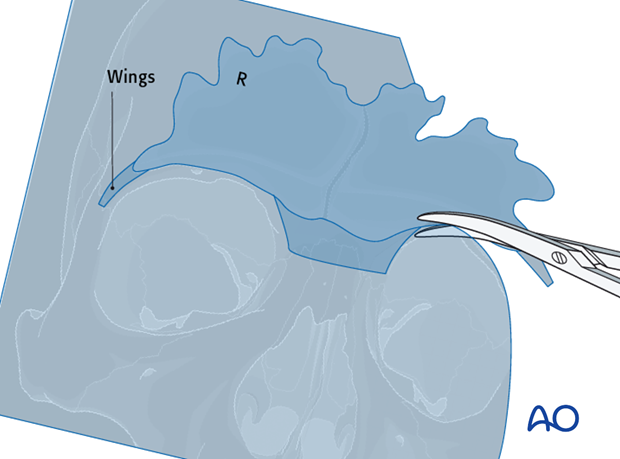
The template is then placed over the sinus using the orbital rim “wings” to help with orientation. The template is held in place. The sinus periphery can then be outlined using ink or electrocautery as previously described.
Intraoperative navigation
Intraoperative navigation can be used to outline the periphery of the sinuses using the preoperative CT scan. A reference array must be fixed to the skull (or Mayfield head holder) to allow for accurate navigation.
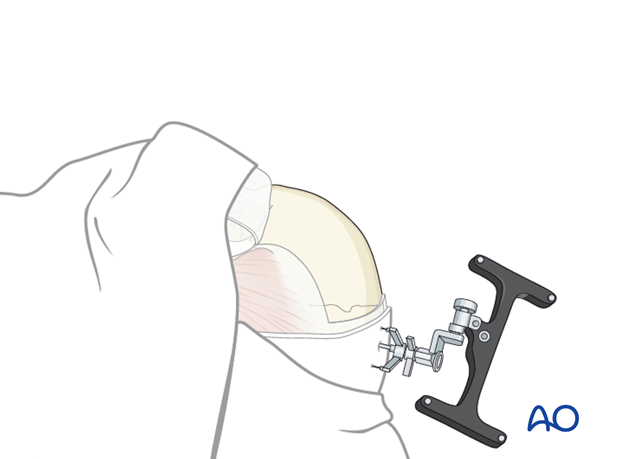
The navigation system is used to guide the probe along the periphery of the sinus.
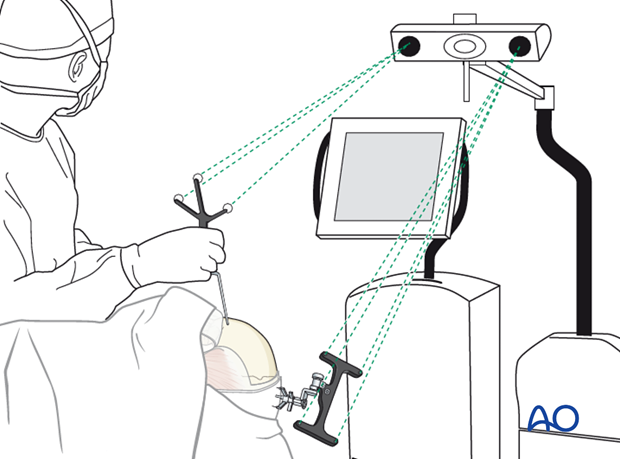
Ink or electrocautery can be used to mark the outline.
5. Osteotomy
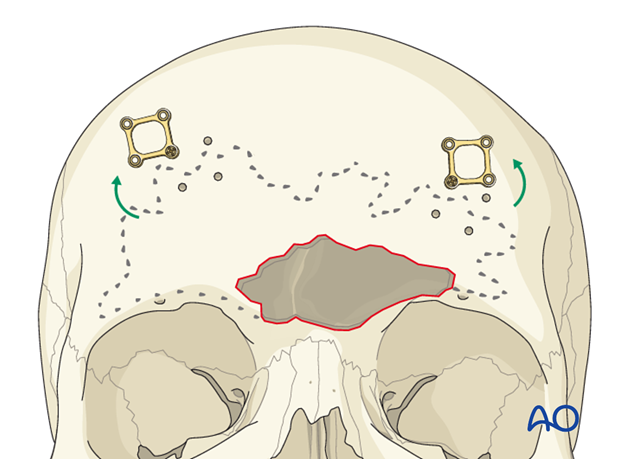
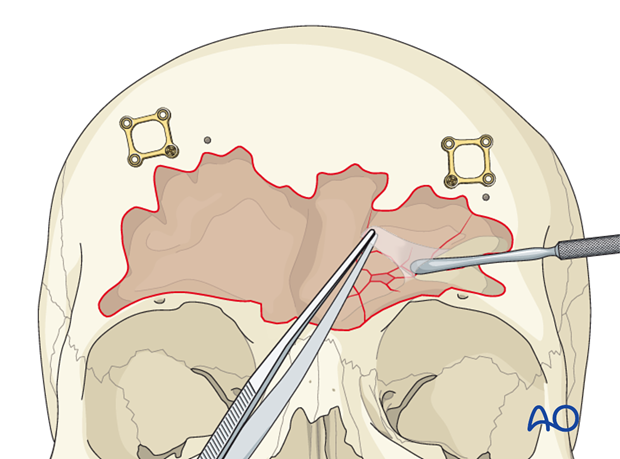
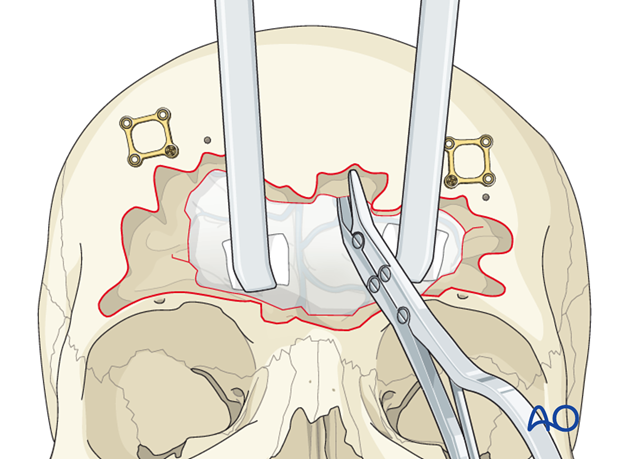
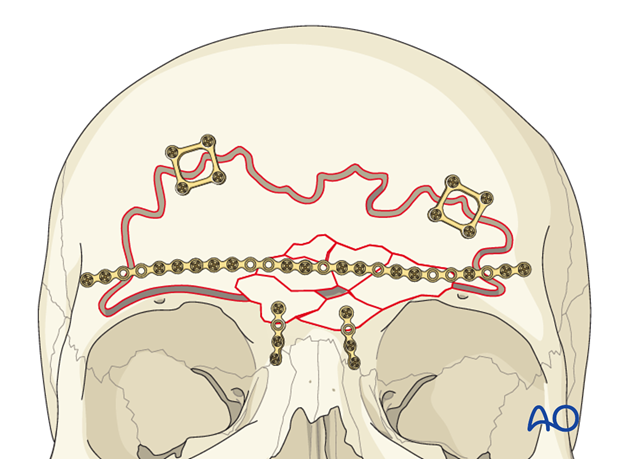
Plate application
After the proposed osteotomy has been marked at the periphery of the sinus, thin plates are applied spanning the sinus margin. An adequate number of plates should be applied to provide stability when the anterior table segment is osteotomized. The plates should be pre-applied prior to the osteotomy. This allows for accurate repositioning of the anterior table bone.
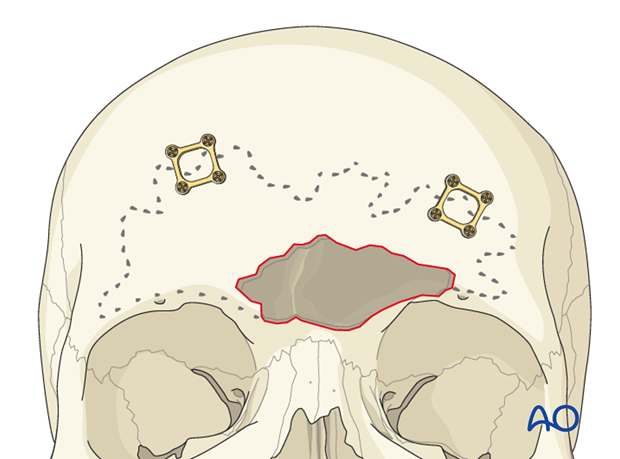
Each plate should be rotated away from the proposed osteotomy line. This can be accomplished by removal all but one screw located on stable bone outside the sinus. The plate can then be rotated away from the sinus.
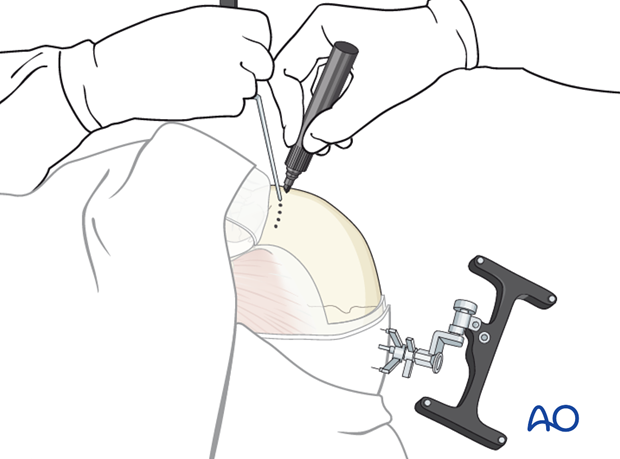
Perforating the anterior table
A sagittal saw can be used to perform the osteotomy. However, a side-cutting burr (as illustrated) is more controlled and accurate. The bit is used to drill sequential holes along the superior border of the sinus. Individual holes are separated by several millimeters.
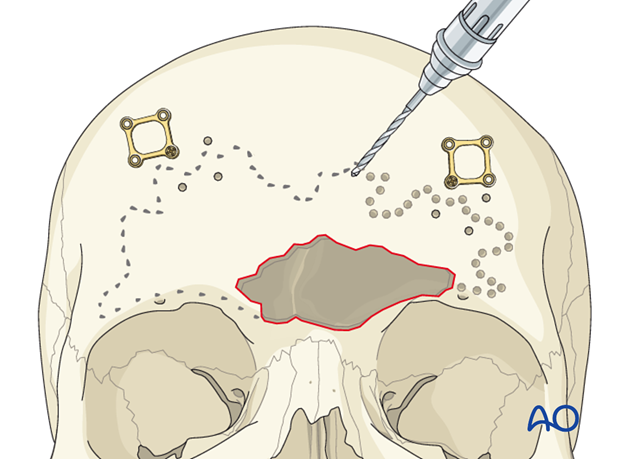
The handpiece should be angled approximately 45° towards the sinus and away from the cranial vault to avoid violation of the posterior table.

Completion of superior osteotomy
The holes are then connected to create a single osteotomy on the superior margin of the sinus.
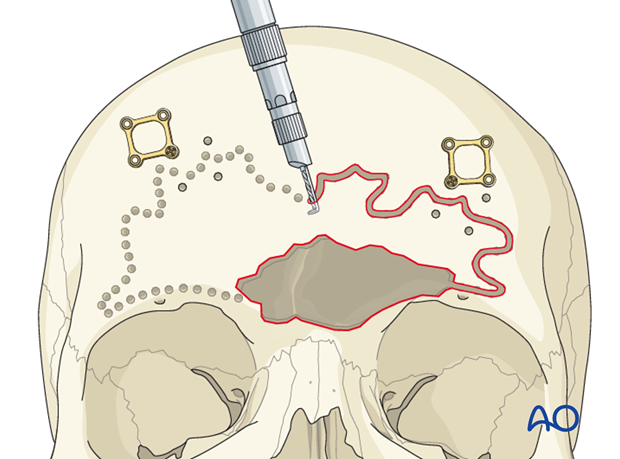
Osteotomizing the orbital rims/glabella
Next, the drill is used to osteotomize the orbital rims and glabella in a similar fashion. Care should be taken to protect the orbital contents and supratrochlear/supraorbital neurovascular pedicles.
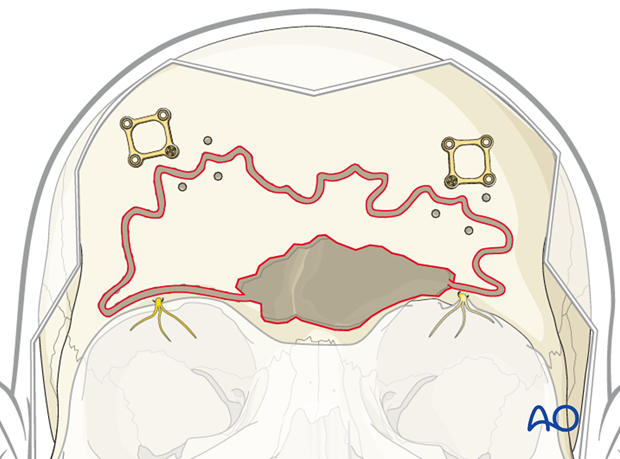
Intersinus septum osteotomy
If the intersinus septum is intact, it may be necessary to insert a curved osteotome through the superior osteotomy site and fracture the intersinus septum just deep to the anterior table bone. Care must be used to avoid injuring the posterior table.
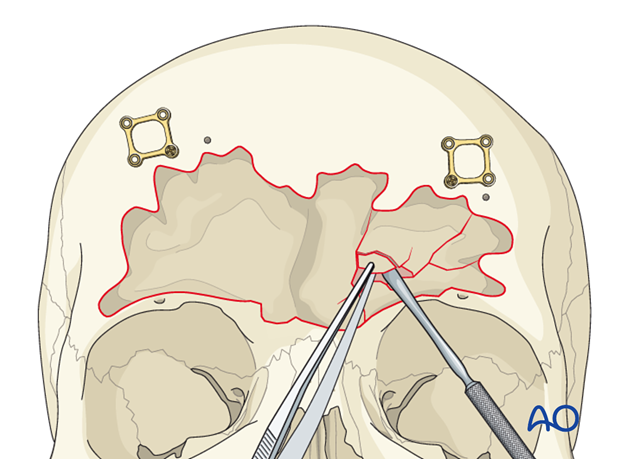
Bone removal
A curved osteotome is then inserted through the superior osteotomy to cantilever the anterior table and generate a controlled fracture of any remaining attached bone. A clamp should be used to control the anterior bone fragment as the osteotomy fracture is completed.

Mucosa removal
The sinus cavity is then suctioned free of any blood or mucous. An elevator and/or forceps are used to remove any bone or mucosa that has been displaced into the sinus cavity. Meticulous dissection technique should be used to avoid iatrogenic injury of the dura.
These injuries can result in severe disruption or even loss of anterior table bone. Therefore, larger bone fragments from the posterior table should be maintained for possible use with reconstruction of the anterior table or obliteration of the frontal recess.
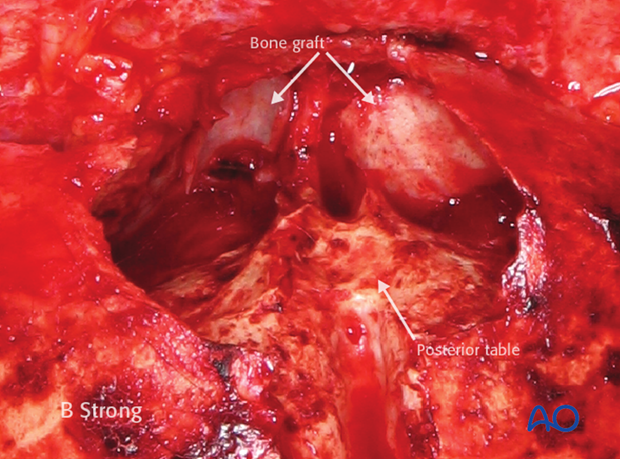
6. Posterior table removal
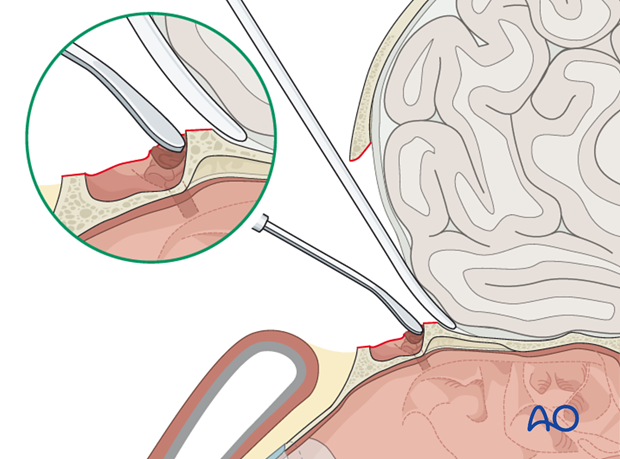
An elevator is used to separate the dura from the posterior table along the entire margin of the defect.
The dura should be elevated from the posterior sinus wall prior to bone removal.
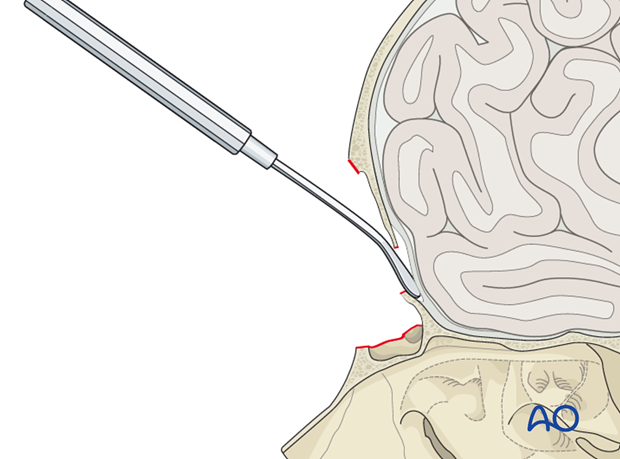
A Kerrison rongeur is then used to initiate the removal of the posterior wall.
The process of dural elevation and bone removal should then be repeated. As the defect gets larger, it is possible to use a double action rongeur to remove the remainder of the posterior wall.
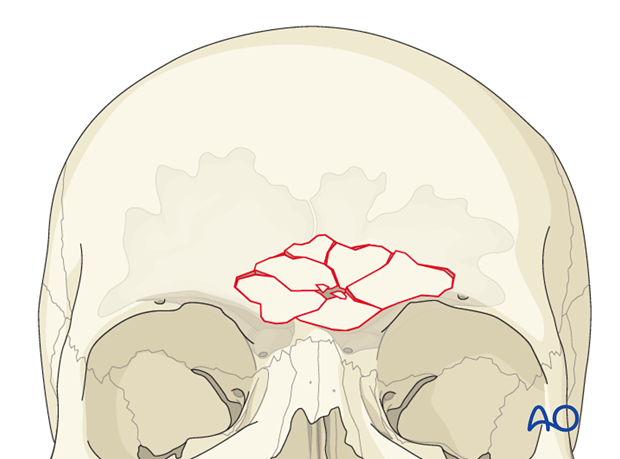
A diamond drill should be used to make a smooth contour between the sinus and intracranial cavities. A malleable retractor is used to retract and protect the brain while drilling. When drilling is complete, there should be a smooth contour between the cranial vault and the sinus.
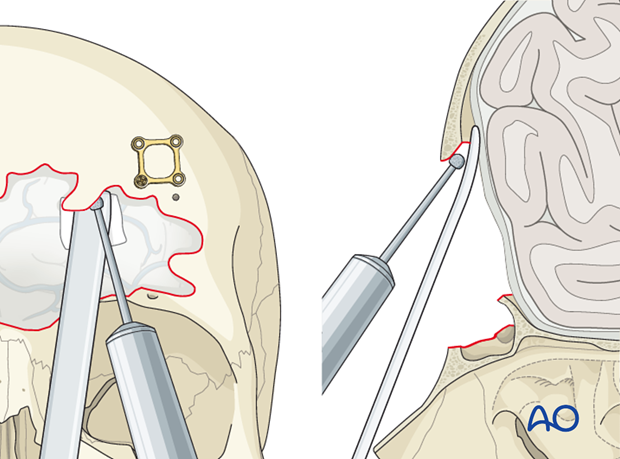
Particular attention must be paid to the scalloped areas at the periphery of the sinus.
7. Mucosa removal
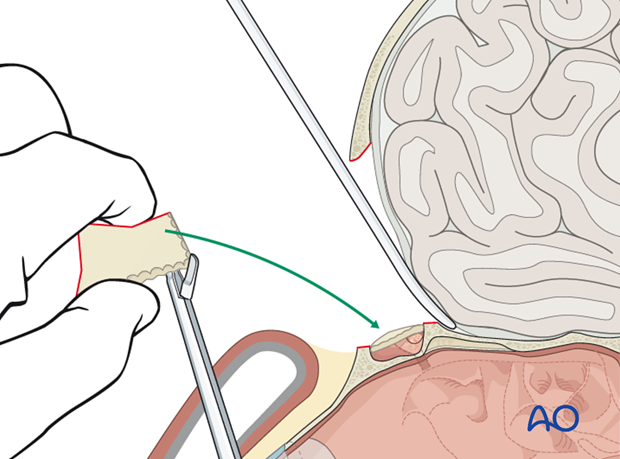
A clamp is used to stabilize the free anterior bone segment(s) that were previously removed. A large diamond burr is then used to remove the mucosa from the inner surface. The mucosa should also be stripped of any posterior table bone fragments to be used for reconstruction of the anterior wall.
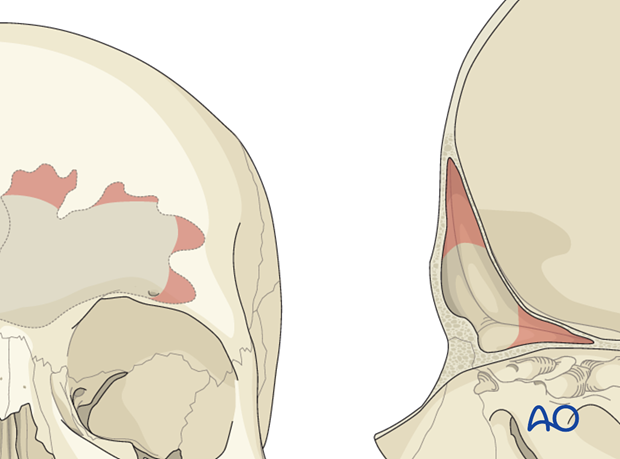
8. Closure of the recess
An elevator is then used to circumferentially elevate the mucosa in the frontal recess bilaterally. The mucosa is then inverted and pushed inferiorly to obstruct the outflow tract. Free fascia is used for obliteration of the outflow tract.
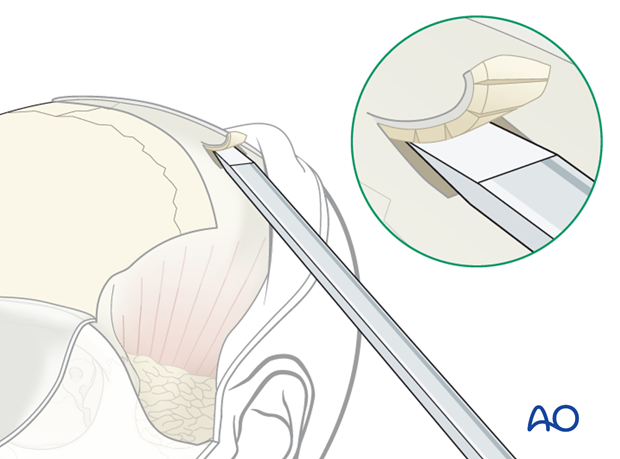
Alternatively, a sharp 1-2 cm straight osteotome can be used to harvest a thin layer of outer layer calvarial bone. If the graft can be harvested from a region with Intact periosteum, this will help maintain the integrity of the graft. If posterior table bone fragments are available, these can also be used to plug the outflow tract.
9. Closure of sinus ostia
Each bone graft is trimmed to fit into the frontal sinus infundibulum using a fine bone rongeur.
The graft is then wedged into place to obstruct the sinus outflow tract.
10. Anterior table repair
The anterior table bone fragments are then repositioned and the pre-applied plates are rotated back into position to fixate the fragments. Replace any remaining fragments and fix them with small plates.
With time, the brain will expand into the cranialized sinus.
11. Aftercare following management of frontal sinus fractures
Evaluation of the patient’s vision
Evaluation of the patient’s vision is performed as soon as they are awakened from anesthesia and then at regular intervals until they are discharged from the hospital.
A swinging flashlight test may serve in the unconscious and/or noncooperative patient; alternatively electrophysiological examination has to be performed but is dependent on the appropriate equipment visual evoked potential (VEP).
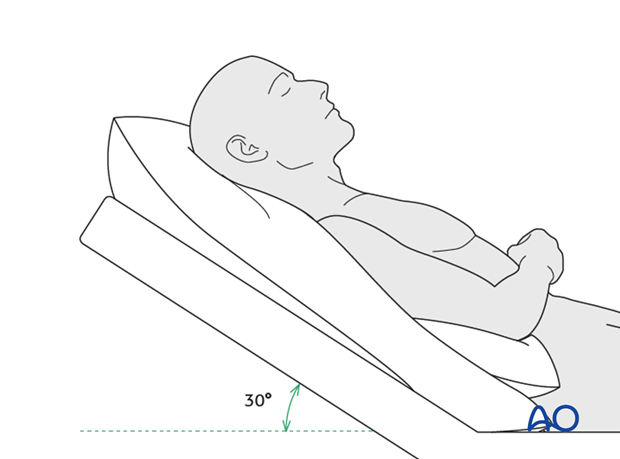
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly improve edema and pain.
Nose-blowing
Nose-blowing should be avoided for at least 3 weeks following frontal sinus and skull base repair.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin for 7 days (nonsteroidal antiinflammatory drugs (NSAIDs) use is controversial)
- Analgesia as necessary
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any one antibiotic, and the recommended duration of treatment is debatable.)
- Nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Visual field test
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked
- If the patient complains of eye pain, evaluate for corneal abrasion
Note: In case of postoperative diplopia, ophthalmological assessment is needed to identify the cause. Hess-chart testing should be performed if diplopia persists.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3-D imaging (CT, cone beam) is recommended to assess complex fracture reductions. In centers where intraoperative imaging is available postoperative imaging can be performed at a delayed time.
For skull base and frontal sinus fractures postoperative imaging should be performed when indicated. If the frontal sinus is preserved, perform a follow up scan in 3-6 months to ensure that it is aerated.
Wound care
The scalp can generally be washed at 5 days postoperatively.
Suture removal from scalp is performed at 7-10 days postoperatively.
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern and patients condition but there are usually no limitations.
Clinical follow-up
Patients should be counseled that frontal sinusitis, mucocele formation, or any other signs of intracranial infection can occur years after the injury. The symptoms should be discussed with the patient including
- Headache
- Erythema
- Mucopurulent nasal drainage
- Frontal bone deformity
- Orbital edema/displacement
Clinical follow-up depends on the complexity of the surgery, and the patient’s postoperative course.
- Other issues to consider are:
- Cranial vault contour deformity
- Sensory nerve compromise
- Problems of scar formation
- Alopecia
- Postoperative headache
- Anosmia
- Dizziness
- Vomiting
- Meningitis (can occur years after injury)
- Mucocele formation (can occur years after injury)
Implant removal
Implant removal is rarely required. It is possible that this may be requested by patients if the implant becomes palpable or visible. In some countries it will be more commonly requested. There have been cases where patients have complained of cold sensitivity in areas of plate placement. It is controversial whether this cold sensitivity is a result of the plate, a result of nerve injury from the original trauma, or from nerve injury due to trauma of the surgery. Issues of cold sensitivity generally improve or resolve with time without removal of the hardware.
Special considerations
Travel in pressurized aircraft is permitted 4 – 6 weeks postoperatively. Mild pain on descent may be noticed. However, flying in non-pressurized aircraft should be avoided for a minimum of 12 weeks.
No scuba diving should be permitted for at least 12 weeks. Additionally, the patient should be warned of long term potential risks.













