Lacerations
1. General considerations
Craniofacial injuries are often associated with lacerations. These existing soft-tissue injuries can be used to directly access fracture sites for fracture management.
The surgeon may elect to extend the laceration to attain enough access to the fractured area, unless this would result in a worse esthetic outcome. Additional incisions are placed starting from the wound margins along the relaxed skin tension lines (RSTL).
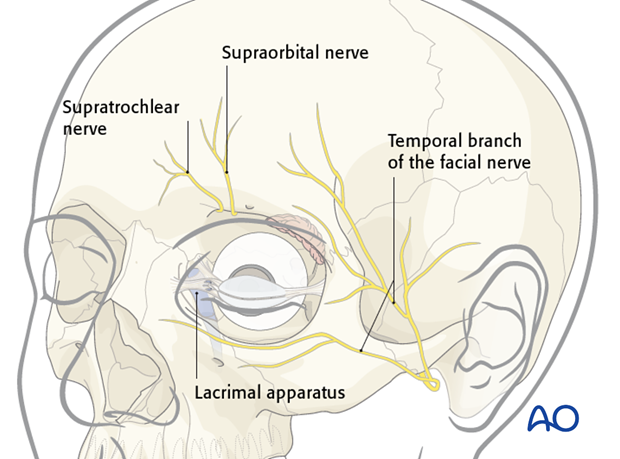
2. Injuries to nerves and the lacrimal apparatus
Depending on the location of the laceration, nerves, or the lacrimal apparatus can be injured.
Respecting their functional importance the facial nerve branches can either be repaired primarily or tagged for ease of location during a secondary repair.
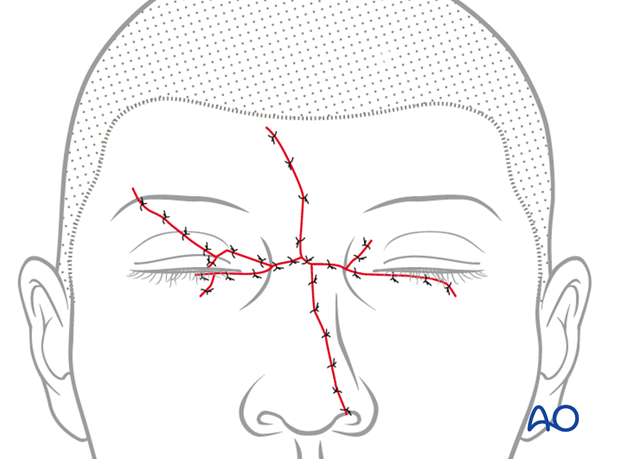
3. Wound closure
Proper cleansing, debridement, and hemostasis should be accomplished prior to the repair of the underlying bony injury, cranial peripheral nerve injuries, or injuries to the lacrimal apparatus.
Facial wounds can be closed primarily up to 24 hours after the injury due the high vascularity of this region.
The laceration is closed in layers with short-term resorbable interrupted sutures, realigning the anatomic structures and eliminating dead space:
- Periosteum
- Mimetic muscles
- Subcutaneous tissues
- Epidermis
Particular attention is given to completing the repair of free eyelid margins.
A variety of skin closure techniques are available based on surgical preference. A drain may be placed if necessary.
Usually the wound is not covered with dressings.
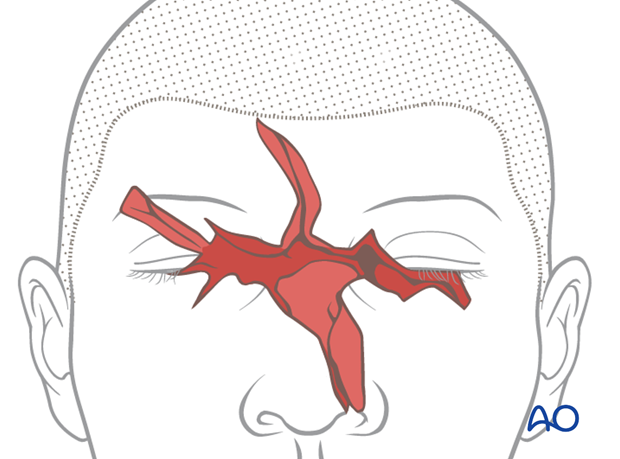
This clinical photograph shows a stellar injury of the central face.

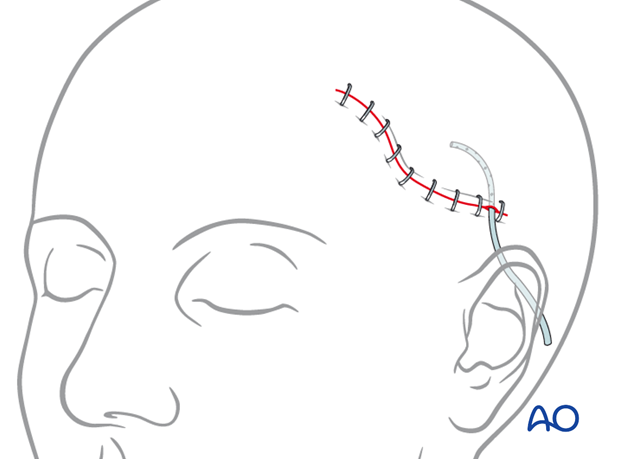
For scalp lacerations most surgeons would prefer use of a mechanical stapler for the skin after a layered closure of the deeper planes. Use of a suction drain to avoid hematoma formation is recommended.
4. Postoperative care and follow-up
Close monitoring of the early wound healing phase is necessary in order to detect infection early enough to prevent wound slough and abscess formation.
Remove sutures in an appropriate time frame.
Instruct the patient to avoid sun exposure and use protection such as hats, shields, and sunscreen.
Further interventions may help to minimize scar contractures and hypertrophy.
Remind the patient that facial scars need months to mature, lose their redness and become less conspicuous.
5. Examples
The use of an existing laceration to access the fracture in the supraorbital region.

Severe trauma with extensive laceration of the NOE area with left globe rupture.














