Open reduction internal fixation
1. Principles
The goal of frontal sinus fracture management is to create a safe sinus, restore facial contour, and avoid short and long term complications.
The goal of open reduction is to reapproximate the bone fragments into their premorbid position and use internal fixation hardware to maintain them in their position.
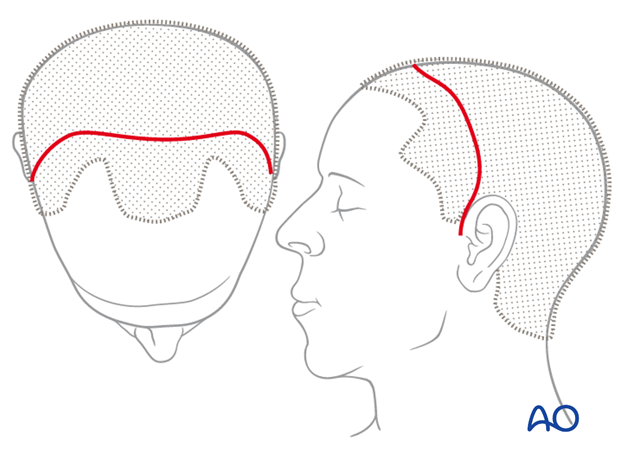
2. Approach
For this procedure the coronal approach is normally used. However, if present, lacerations can be used to directly access fracture sites for fracture managment.
3. Reduction
General considerations
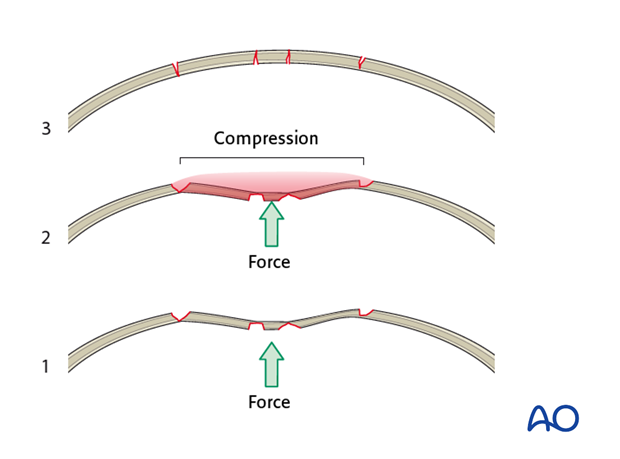
The anterior table of the frontal sinus is normally convex. Compressive forces on the frontal bone deform the convexity into a concavity. This may or may not result in fracture comminution.

Mobilization of the depressed bone fragment(s) may require significant effort to overcome compressive forces between bone fragments.
Reduction techniques
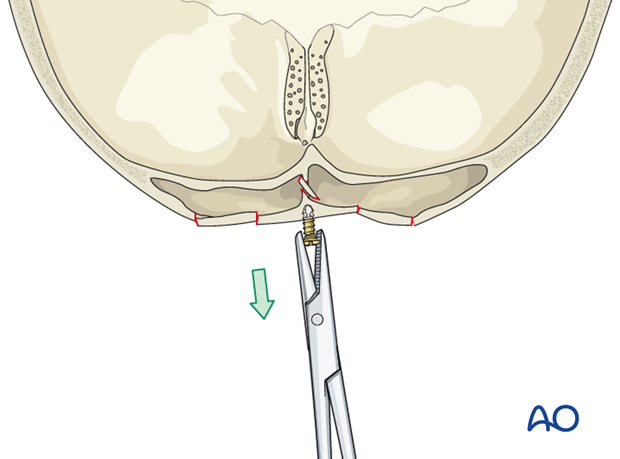
There are several techniques to reduce the fragments:
- Mobilizing the bone fragments using an elevator

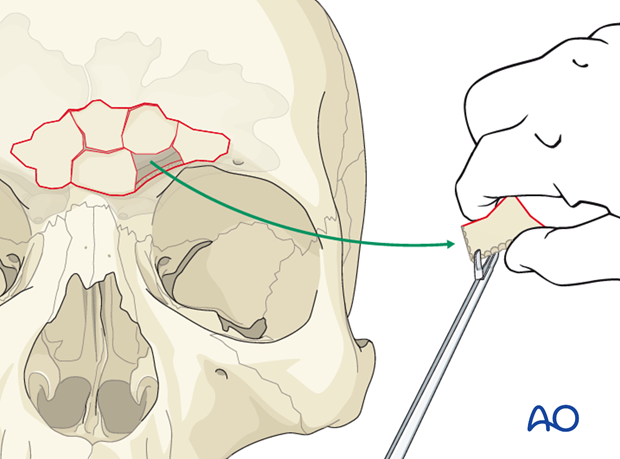
- Inserting a screw into a bony fragment and reducing it by pulling it outwards
Simple reduction
Minimally comminuted fractures may be stable after a simple reduction. Interfragmentary resistance may alleviate the need for internal fixation.
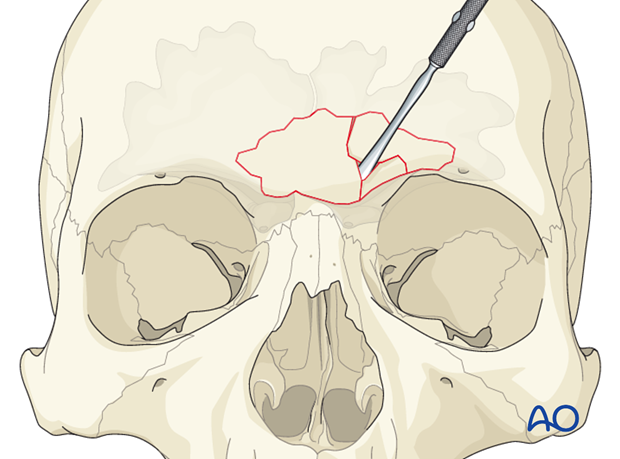
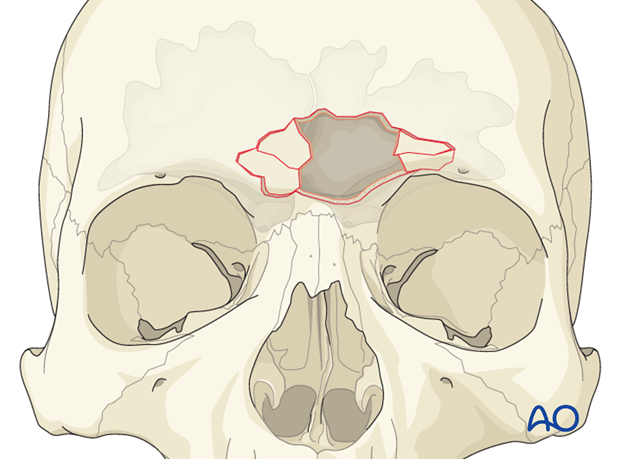
Comminuted fractures
More comminuted fractures often require removal of bone fragments to achieve fracture reduction.
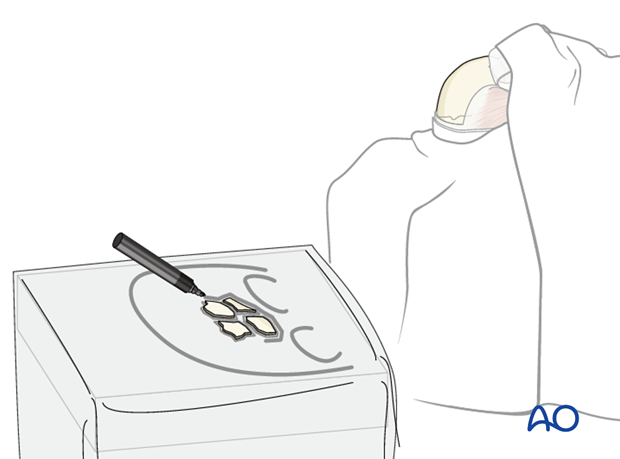
Pearl: identification of explanted bone fragments
Final orientation of any removed bone fragments can be challenging. Placing the explanted segments on a rough sketch of the skull made with a sterile pen will maintain orientation until re-implantation. Outline each segment and the overall shape of the defect.
The bone fragments should be kept moist until they are re-placed.
Pitfall: trapped mucosa
Comminuted fractures can result in trapped mucosa within fracture lines. This can result in sinusitis, or late mucocele formation.
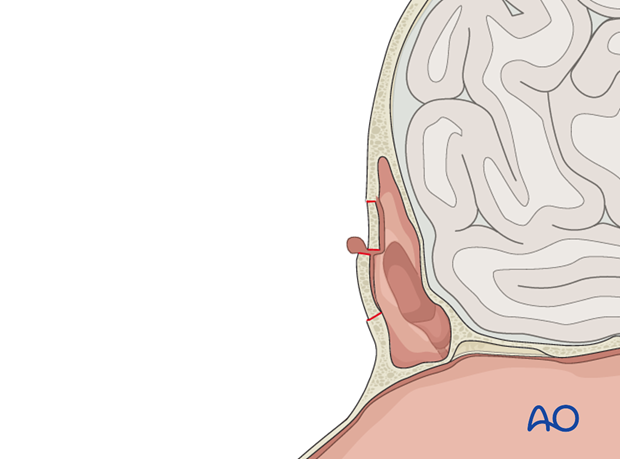
Any redundant or injured mucosa at the periphery of the fracture or on isolated bone fragments should be removed.
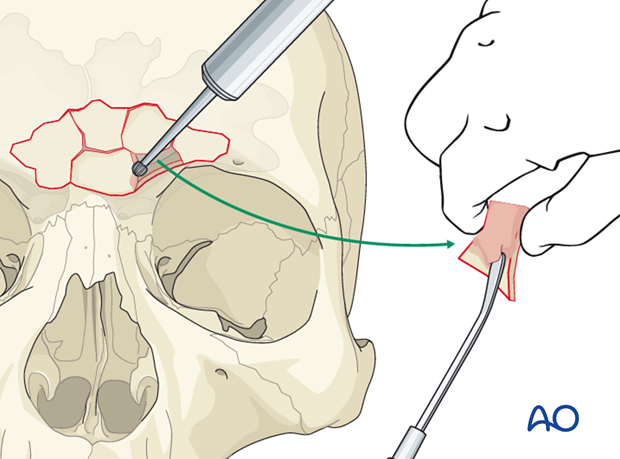
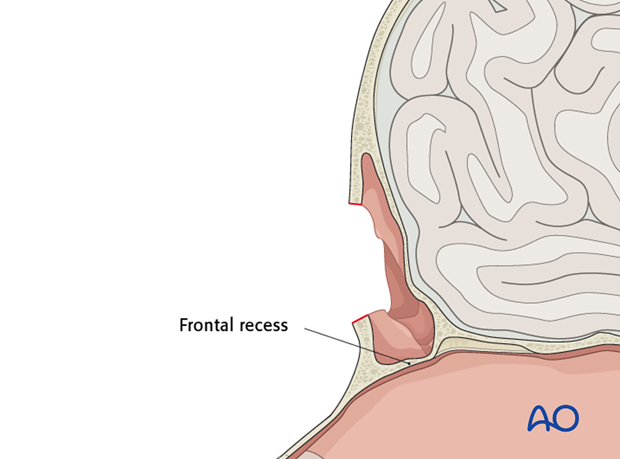
If removal of anterior table bone fragments is required, the defect should be used to inspect the frontal recess and assure that it is not injured.
Pearl: trimming fragments
Traumatic distortion of fracture segments may make it difficult to realign them. While every effort should be made to maintain the integrity of each bone fragment, it may be necessary to trim the edge of a fragment to allow for fracture reduction.
4. Fixation
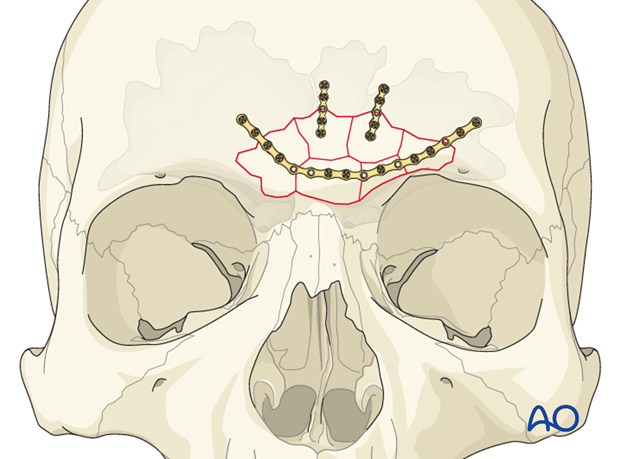
Bone fragments should then be repositioned and fixed with internal fixation hardware.
Stability can generally be achieved with thin titanium plates. This will minimize the risk of visibility/palpability of the implants. The number of plates will be dictated by the stability of the reduction.
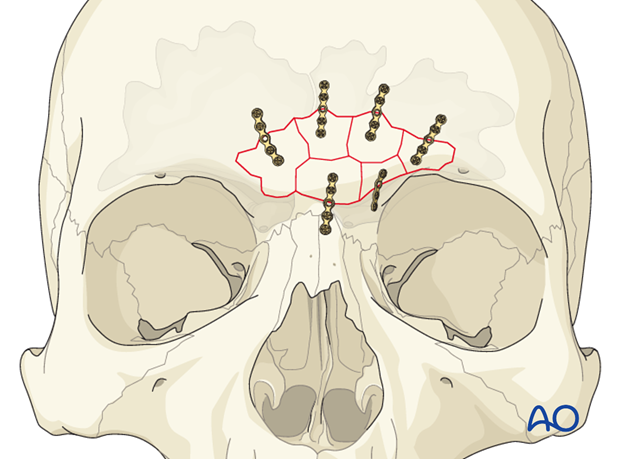
Alternatively, one long curved plate might be used to secure several fracture segments.
5. Aftercare following management of frontal sinus fractures
Evaluation of the patient’s vision
Evaluation of the patient’s vision is performed as soon as they are awakened from anesthesia and then at regular intervals until they are discharged from the hospital.
A swinging flashlight test may serve in the unconscious and/or noncooperative patient; alternatively electrophysiological examination has to be performed but is dependent on the appropriate equipment visual evoked potential (VEP).
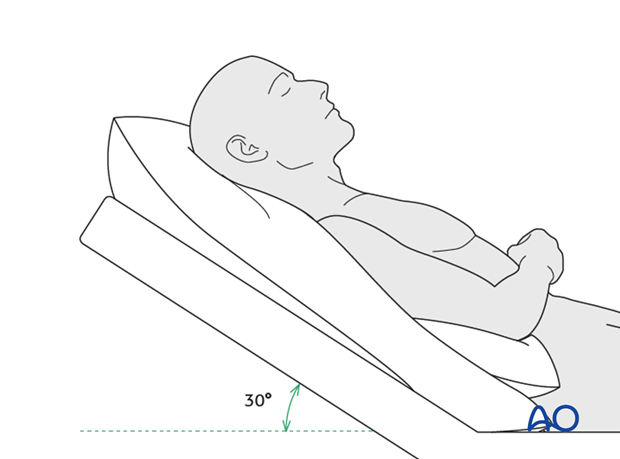
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly improve edema and pain.
Nose-blowing
Nose-blowing should be avoided for at least 3 weeks following frontal sinus and skull base repair.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin for 7 days (nonsteroidal antiinflammatory drugs (NSAIDs) use is controversial)
- Analgesia as necessary
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any one antibiotic, and the recommended duration of treatment is debatable.)
- Nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Visual field test
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked
- If the patient complains of eye pain, evaluate for corneal abrasion
Note: In case of postoperative diplopia, ophthalmological assessment is needed to identify the cause. Hess-chart testing should be performed if diplopia persists.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3-D imaging (CT, cone beam) is recommended to assess complex fracture reductions. In centers where intraoperative imaging is available postoperative imaging can be performed at a delayed time.
For skull base and frontal sinus fractures postoperative imaging should be performed when indicated. If the frontal sinus is preserved, perform a follow up scan in 3-6 months to ensure that it is aerated.
Wound care
The scalp can generally be washed at 5 days postoperatively.
Suture removal from scalp is performed at 7-10 days postoperatively.
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern and patients condition but there are usually no limitations.
Clinical follow-up
Patients should be counseled that frontal sinusitis, mucocele formation, or any other signs of intracranial infection can occur years after the injury. The symptoms should be discussed with the patient including
- Headache
- Erythema
- Mucopurulent nasal drainage
- Frontal bone deformity
- Orbital edema/displacement
Clinical follow-up depends on the complexity of the surgery, and the patient’s postoperative course.
- Other issues to consider are:
- Cranial vault contour deformity
- Sensory nerve compromise
- Problems of scar formation
- Alopecia
- Postoperative headache
- Anosmia
- Dizziness
- Vomiting
- Meningitis (can occur years after injury)
- Mucocele formation (can occur years after injury)
Implant removal
Implant removal is rarely required. It is possible that this may be requested by patients if the implant becomes palpable or visible. In some countries it will be more commonly requested. There have been cases where patients have complained of cold sensitivity in areas of plate placement. It is controversial whether this cold sensitivity is a result of the plate, a result of nerve injury from the original trauma, or from nerve injury due to trauma of the surgery. Issues of cold sensitivity generally improve or resolve with time without removal of the hardware.
Special considerations
Travel in pressurized aircraft is permitted 4 – 6 weeks postoperatively. Mild pain on descent may be noticed. However, flying in non-pressurized aircraft should be avoided for a minimum of 12 weeks.
No scuba diving should be permitted for at least 12 weeks. Additionally, the patient should be warned of long term potential risks.













