Delayed endoscopic repair
1. Principles
Indication
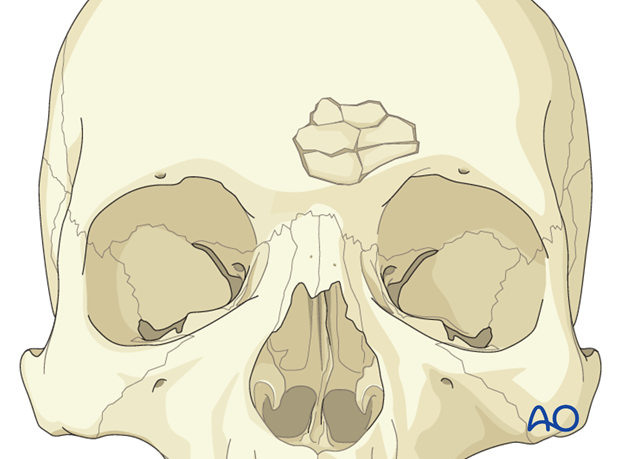
Delayed endoscopic repair should be considered in patients with isolated fractures, limited to the anterior table who continue to have a cosmetic contour deformity after 3-4 months of observation and do not demonstrate any obstructive signs of sinus pathology.
Endoscopic repair of anterior table frontal sinus fractures is a recently developed technique aimed at delayed repair of limited fractures through a minimally invasive approach.
The benefits include limited incisions. The fractures are observed for 3-4 months and allowed to heal. Only those patients with an esthetic deformity and who desires surgical repair are treated with an onlay graft to camouflage the defect.
2. Approach
For this procedure the endoscopic approach to the anterior table is normally used.
3. Implant preparation
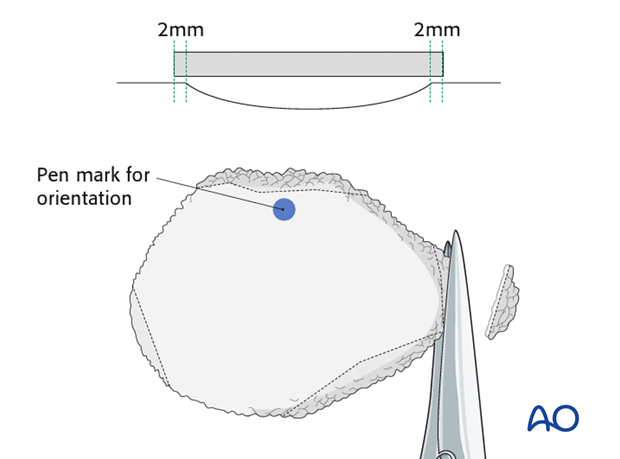
A sheet of 0.85 thick porous polyethylene is placed on the skin over the fracture. The sheeting is trimmed slightly larger then the defect.
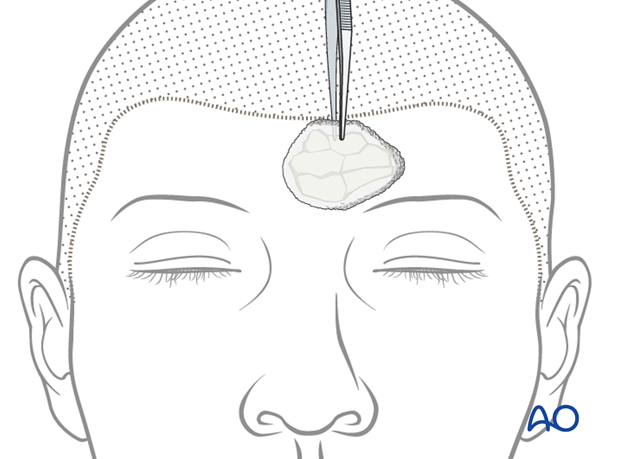
The superior edge of the implant is marked with pen to maintain orientation endoscopically.
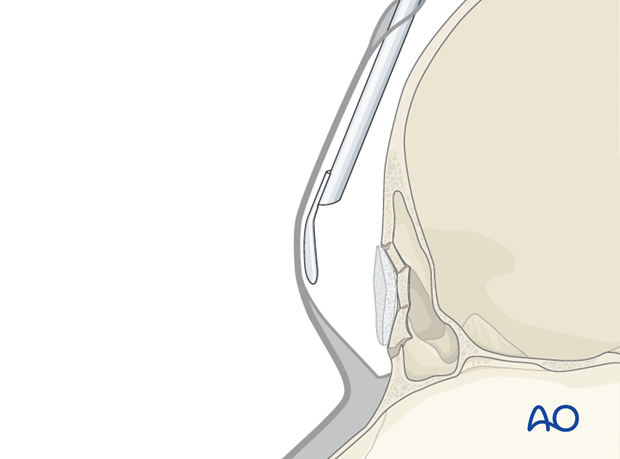
The implant is then inserted through the working incision and positioned above the fracture.
The implant is then removed and trimmed to the appropriate size. It should cover the fracture and overlap stable bone by approximately 2 mm. This step may need to be repeated several times to assure the appropriate size.
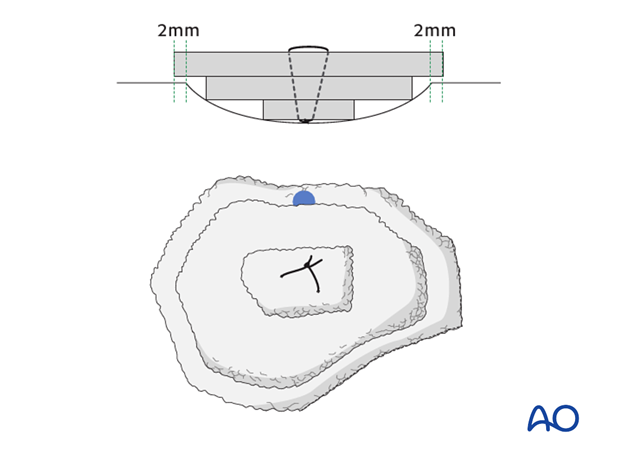
Pearl: layered implant
The implant may be sutured together in layers to fill deeper defects.
4. Implant fixation
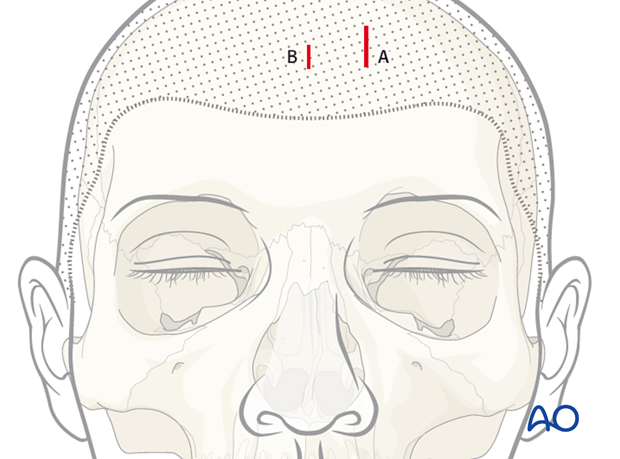
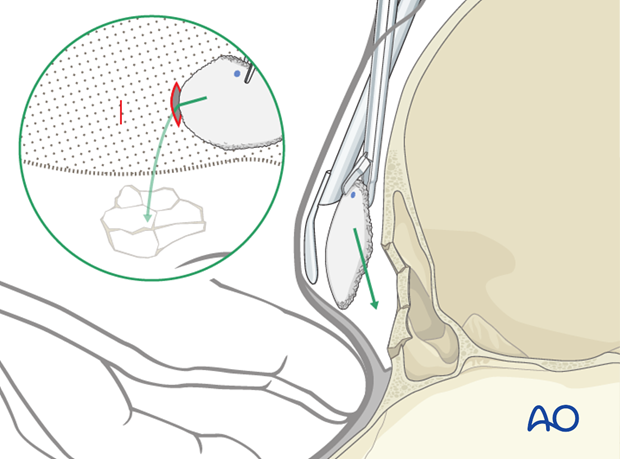
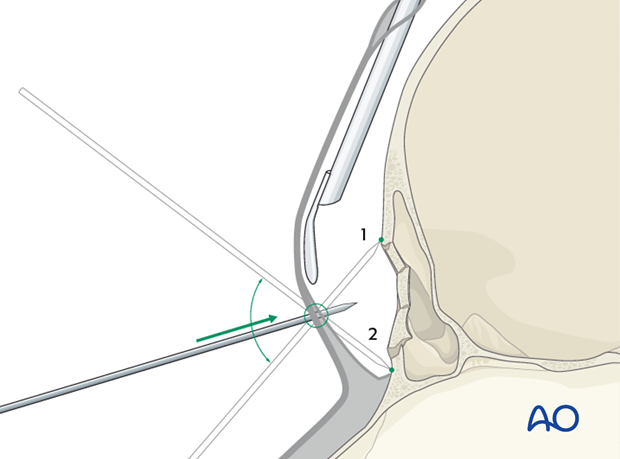
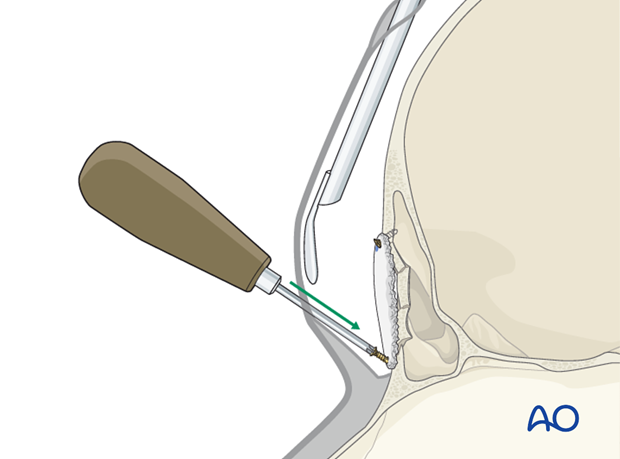
A 21 gauge needle is then passed through the forehead skin above the fracture to determine the optimal location for a forehead incision to be used for screw fixation of the implant. The needle is repositioned under endoscopic visualization until it is optimally positioned to allow for two screws to be placed on opposite sides of the implant through one stab incision. While one screw is generally sufficient (1) to stabilize the implant, the stab incision should be appropriately positioned to allow for placement of a second screw (2) should that be required.
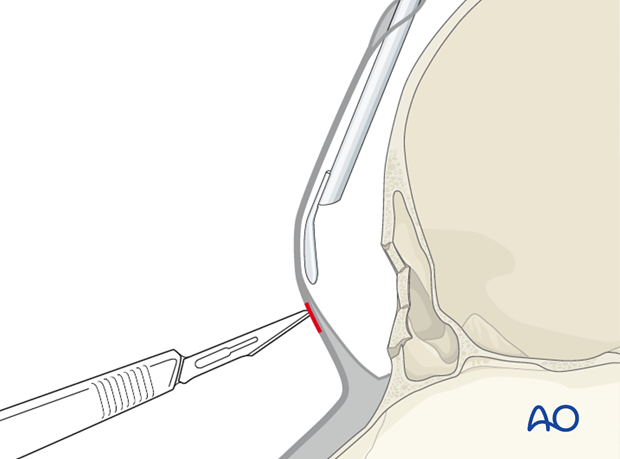
A stab incision is then performed using a no. 11 blade at the predetermined site. The trimmed implant is then positioned over the fracture.
The implant is fixed with a small self-drilling screw, of the appropriate length. The screw must be securely attached to the screw driver in order to avoid dislodgement in the soft tissues. The screw should be placed approximately 1 mm away from the implant edge or the implant may tear. A screw may be placed on the contralateral side of the implant if greater stability is required.
Larger implants may require a second stab incision.
Alternatively, hydroxyapatite bone cements can be used instead of the polyethylene sheets to fill the contour deformity.
5. Aftercare following delayed endoscopic repair of anterior table fractures
The aftercare for delayed endoscopic repair of anterior table fractures is the same as routine postoperative care after the placement of an alloplast and would include appropriate antibiotic coverage and postoperative clinical monitoring for any signs of infection.













