Examination of patients with NOE fractures
1. Clinical examination
A thorough visual inspection from frontal, worm’s eye, and bird’s eye views should be performed, followed by manual palpation of the supraorbital rims, frontonasal junctions, lateral nasal complex, inferior orbital rims, and the nasal complex as a unit. Deep palpation over the medial orbital rim (posterior to the nose) can reveal a 'click' of bone displacement or mobility.
The patient often has swelling in the medial canthal area and pain and crepitation with palpation. One may detect posterior dislocation of the bone cartilages of the nose.
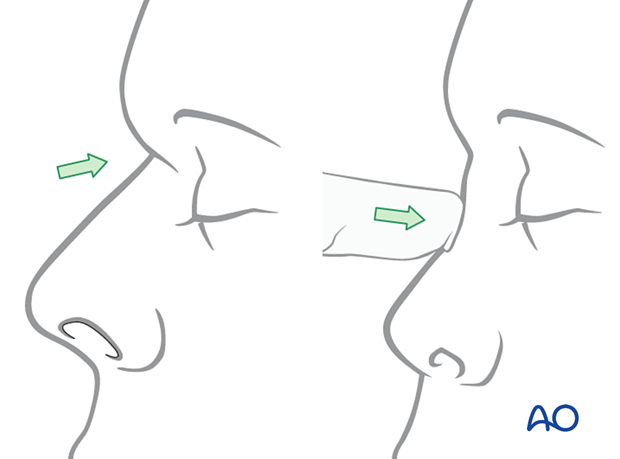
Palpation of the distal septum at the columella may reveal lack of distal nasal support due to superior dislocation of the septum.

The nose can be retruded and impacted at the nasofrontal suture area with a lack of support for the nasal septum and cartilages.
Intercanthal distance
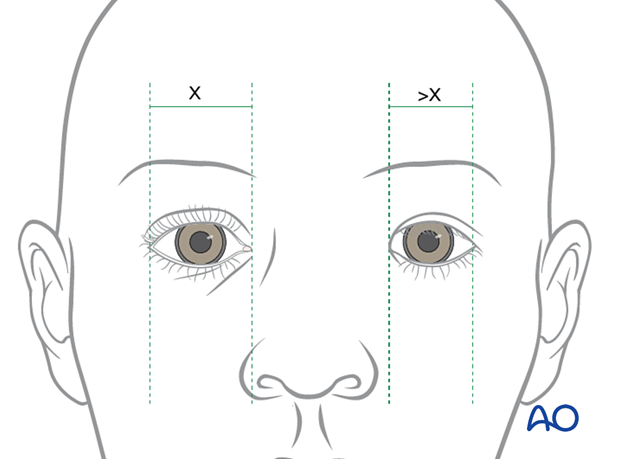
There will be a lack of definition of the bony anatomy in the medial canthal area and possible lateral splaying of the medial canthus with increased intercanthal distance (the normal distance varies between 28 and 35 mm depending on the ethnic group, eg, in Caucasians, more than 35 mm intercanthal distance is considered abnormal).
A thorough ophthalmological examination should also be performed.
This illustration demonstrates widening on the left, with the medial canthus positioned lateral to the lateral nasal alar margin.
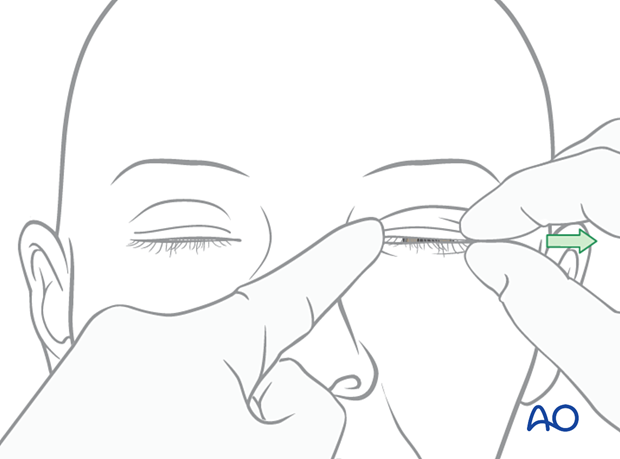
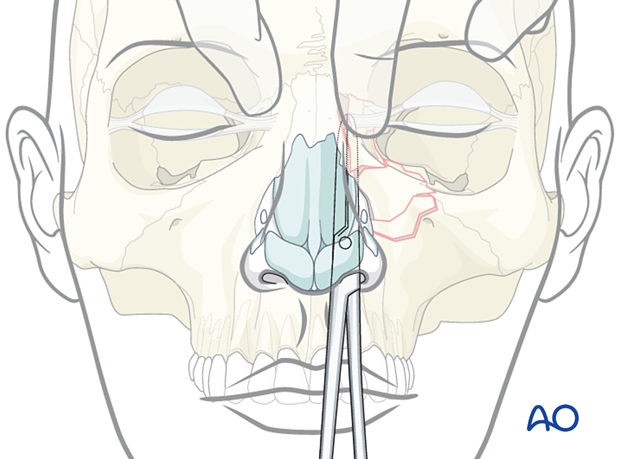
Bow-string test
The surgeon may be able to grab the eyelid or use forceps to hold the skin in the medial canthal area and pull it laterally (“bow-string” test).
In the bow-string test, the lid is pulled laterally while the tendon area is palpated to detect mobility of the fracture segments. A lack of resistance or movement of the underlying bone is indicative of a fracture. This test is only positive in the most severe injuries.
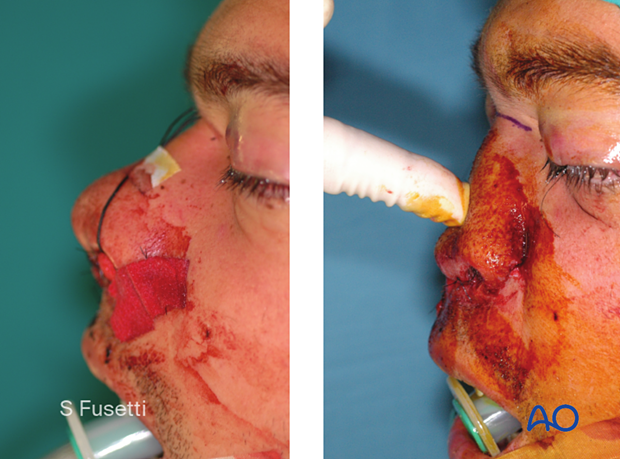
Bimanual palpation
Another test is to place an instrument (Kelly clamp) in the nose with the tip under the canthal ligament (not the nasal bone). Pushing the tip of the clamp laterally allows detection of movement of the bone bearing the attachment of the medial canthal ligament. Placement of the clamp underneath a nasal bone will detect movement of a nasal fracture. It is important that the clamp be directly under the bone bearing the attachment of the medial canthal ligament with a palpating finger directly over the medial canthal ligament attachment to bone.
2. Radiographic findings
A surgeon can often distinguish between a type I NOE fracture versus a type II/III fracture by the degree of comminution noted on the CT. In type I fractures only the inferior aspect of the piriform aperture and the orbital floor are dislocated. Type II and III fractures dislocate the entire medial maxilla and medial orbital rim allowing lateral displacement of the medial canthal ligament. In type I fractures the medial canthal ligament is often displaced slightly medially.
It is generally very difficult to distinguish between a type II and a type III NOE fracture based on radiographic examination. The finding of a medial canthal tendon avulsed from its insertion on the bone is often determined intraoperatively.
This CT shows a sagittal view of a bilateral NOE type II fracture. Note the depression of the nasal root.
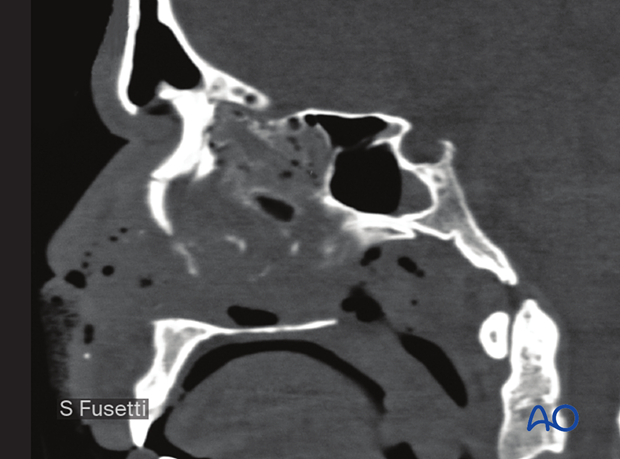
This CT shows a coronal view of the same patient.
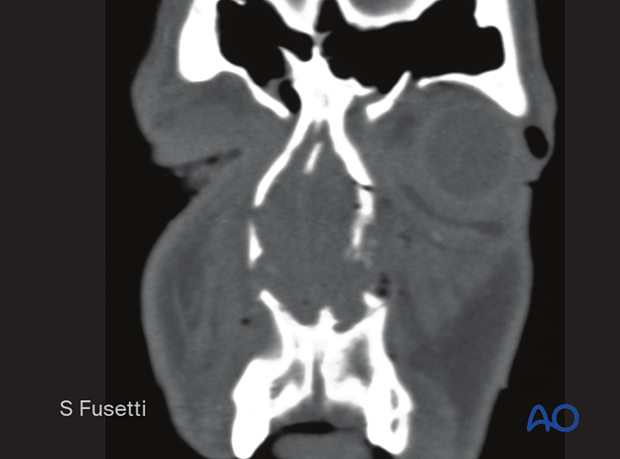
This CT shows axial views of the same patient. The axial view shows the involvement and potential compromise of the lacrimal system.
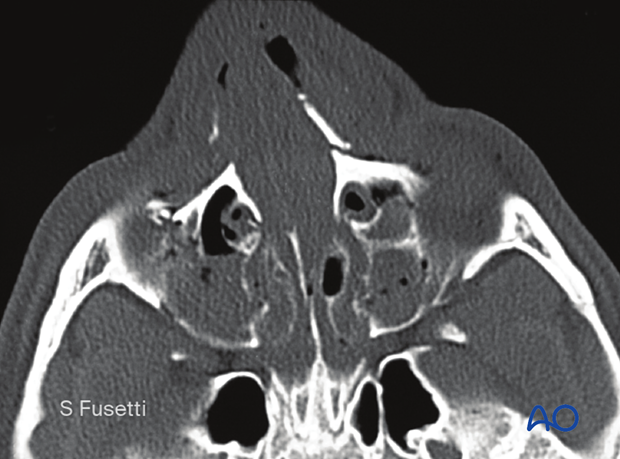
Note the depression of the nasal bone complex.

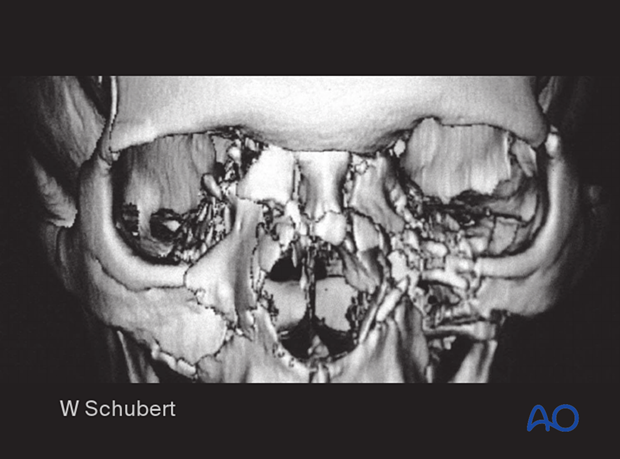
A 3D CT, as shown, can help assess the severity of the injury, but the final diagnosis requires axial and coronal CT scans, bimanual examination, and clinical findings of the nose and orbit. The exact findings are usually confirmed by additional intraoperative information.
This 3D CT shows a bilateral NOE type II with the involvement of the nasal bones.
3. Suspected CSF leak
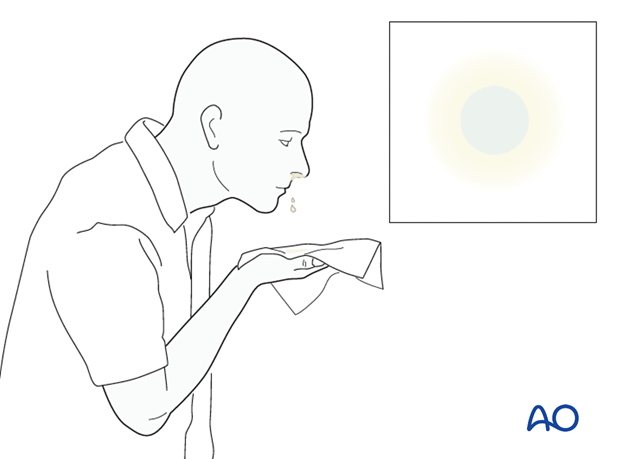
The following diagnostic procedures can be performed if there is a suspected CSF leak (clinical sign: straw-colored or clear nasal drainage):
- Tilt test with positive halo sign (as illustrated)
- CT scan with thin coronal cuts (0.5 mm) of the cribriform plate
- Comparison of the concentration of glucose between fluid and patient’s serum
- Laboratory analysis for beta-2-transferrin
- Application of fluorescent dyes and direct visualization of the leak via transnasal endoscopy. Note: in many countries, the use of intrathecal dyes is not approved and, therefore, special permission from the patient may be necessary.
4. Evaluation of lacrimal apparatus
The lacrimal drainage system is intimately related to the NOE region and can be damaged during the trauma. It is difficult to confirm the patency/continuity of the nasolacrimal system at the time of surgical treatment. Probing often produces false passages. The literature indicates that proper positioning of the bone surrounding the nasolacrimal system will often produce good function. Lacerations of the canaliculi area should be repaired over stent support. Other discontinuities of the nasolacrimal system, if detected, can be repaired.
Click here for a detailed description of the repair of the lacrimal system.













