Examination of patients with nasal bone fractures
Diagnosis should be made from the history of the injury, physical examination, and imaging. The direction and strength of the impact should be considered. Preexisting nasal or septal deformities, and remote injuries or operations should also be noted.
A history of nasal bleeding may indicate a mucosal laceration. Skin lacerations may suggest fractures of a particular anatomical area.
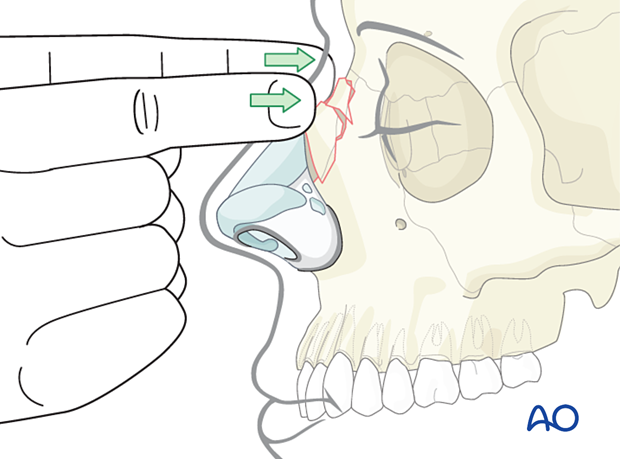
Physical examination
The external nose should be examined via palpation. Bimanual palpation may detect crepitus or bone movement.
Swelling may preclude proper assessment.
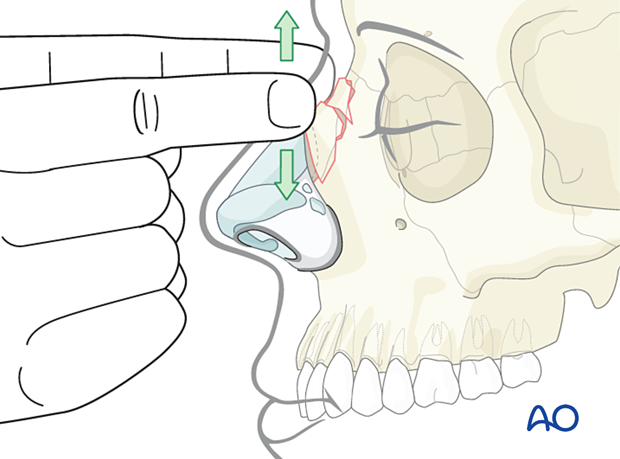
Step-offs, humps, bone discontinuity, and crepitus are all signs of nasal bone fractures.
Ecchymosis, or the presence of a hematoma, should also be noted.
The nasal dorsum should be observed from frontal, worm's eye, and bird's eye views to appreciate the complete extent of external nasal deformities from multiple perspectives.
The origin and extent of epistaxis and/or cerebrospinal fluid (CSF) rhinorrhea should be determined.
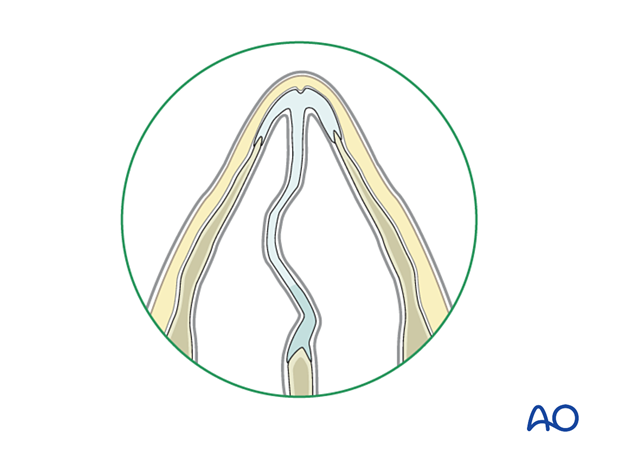
Intranasal anatomy should be assessed using a nasal speculum, looking for septal deviation, mucosal laceration, and septal hematoma.
The presence of a significant septal hematoma requires immediate drainage.
Hematoma is diagnosed as follows:
- The main symptom is severe nasal obstruction.
- On examination, the septum appears swollen and boggy.
- The swollen area should be palpated with a cotton-tipped applicator. If a hematoma is present, it should be compressible.
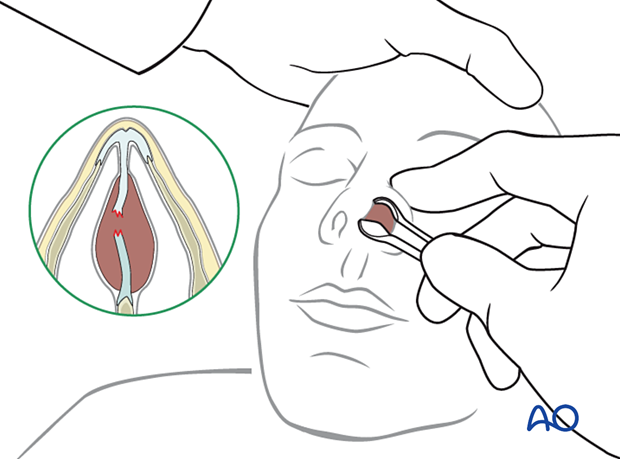
Preexisting septal deviation should be differentiated from traumatic fracture to the septum, if possible.
A detailed facial examination in patients with nasal bone fractures is important and should include visual acuity, extraocular muscle movements, pupil size and reactivity, intercanthal distance, medial canthal tendon position, mandibular range of motion, and occlusion. Forces great enough to fracture the nasal and septal bones are substantial enough to injure adjacent structures such as the globe and the orbital floor. For further details, please refer to Examination of patients with midfacial injuries.
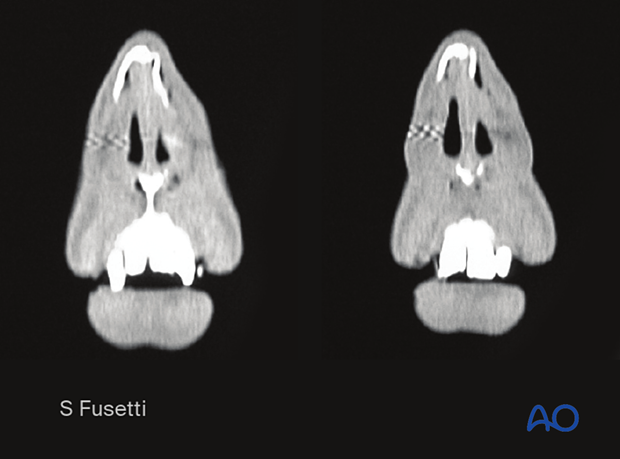
Imaging
Most surgeons find plain films of the nose to be inadequate.
The greatest weakness of plain films is their inability to assess the injury for correct management. The management of nasal bone fractures is based upon correlating clinical assessment of appearance and function with a detailed multiplane CT evaluation.
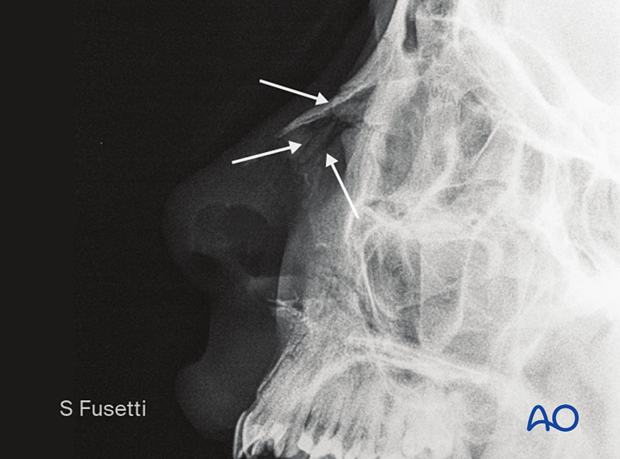
CT scans should be performed to accurately diagnose nasal bone fractures and they also detect associated fractures of other facial bones.