Occlusal splints
1. Introduction
Because of concerns of possible injury to the tooth buds with mixed dentition, various mandibular splints may be needed to treat pediatric mandibular fractures.
Options for splints include:
- Labial splints
- Lingual splints
- Occlusal splints
- Combinations of the above
These splints can be used as stabilization of the mandible without the use of internal fixation hardware.
We will demonstrate the implementation of a lingual splint.
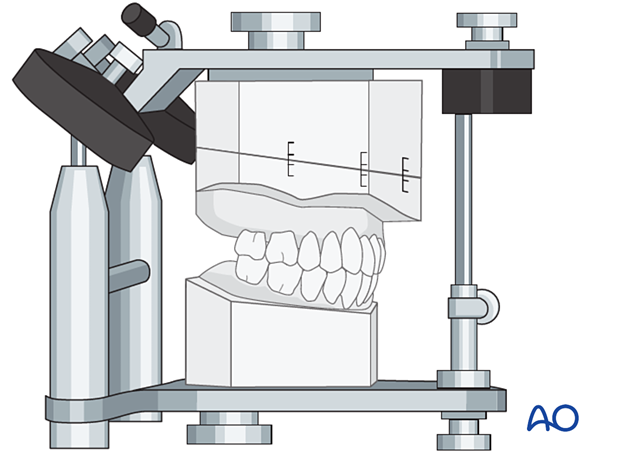
2. Splint preparation
Dental impressions of the mandibular and maxillary dentition are made.
The segmented mandibular cast is realigned using the maxillary models to achieve the premorbid occlusion.
The model is then mounted in an articulator and used to prepare labial, lingual, or occlusal splints.
3. Patient preparation
This procedure is typically performed with the patient placed in a supine position.
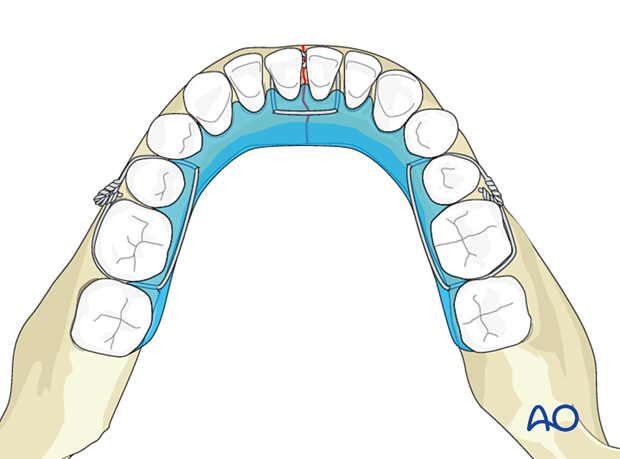
4. Fixation using circumdental wires
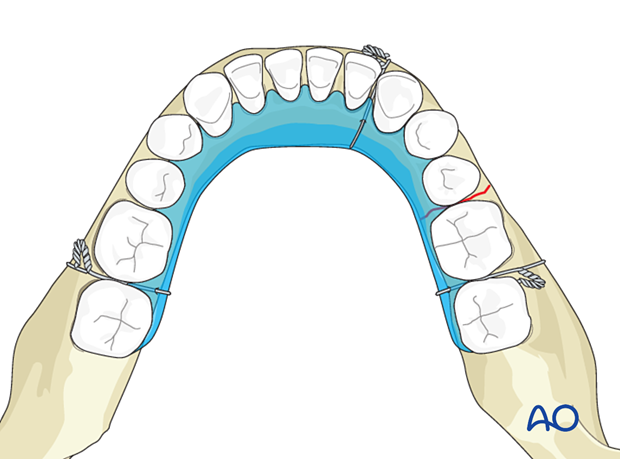
Holes are made in the splints to secure them to the teeth.
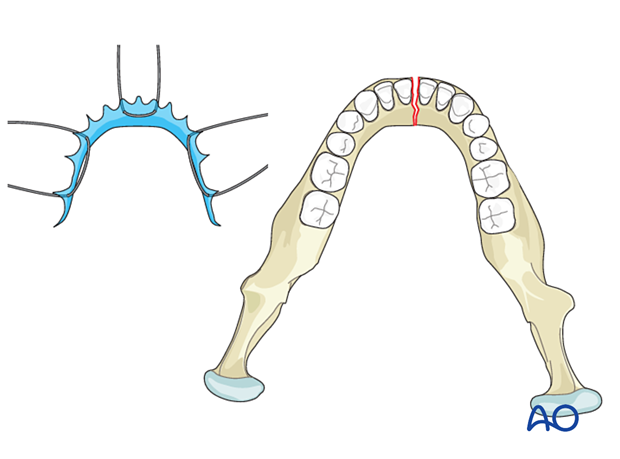
The displaced mandibular fragments are reduced and stabilized with the use of splints.
In some cases, a lingual splint can be used in combination with an arch bar.
5. Fixation using circummandiblular wires
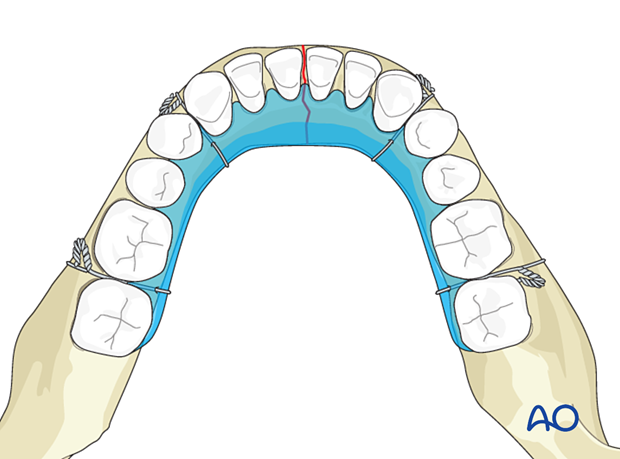
Consider circummandibular wires in primary and mixed dentition cases, as there is a tendency for the fixation to slip off the primary dentition.
The displaced mandibular fragments are reduced.
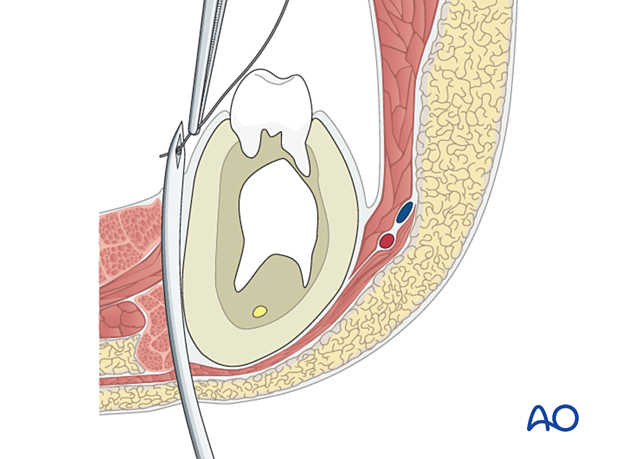
An awl (or needle) is inserted in the submandibular area and passed close to the periosteum on the labial or lingual side of the mandible into the mouth, being careful not to injure the mental nerve.
A wire is passed through the awl.
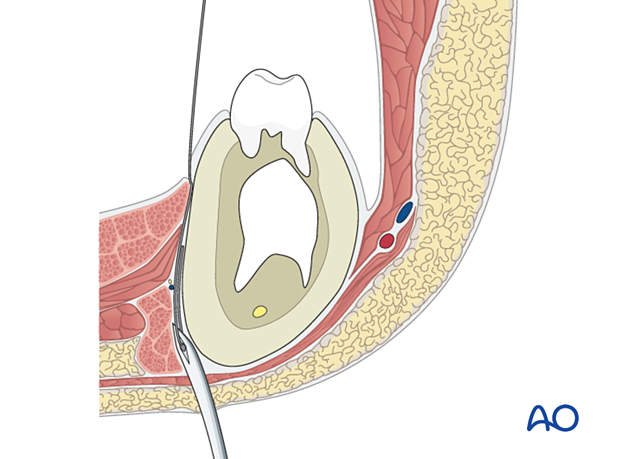
The awl is retracted to the inferior margin of the mandible…
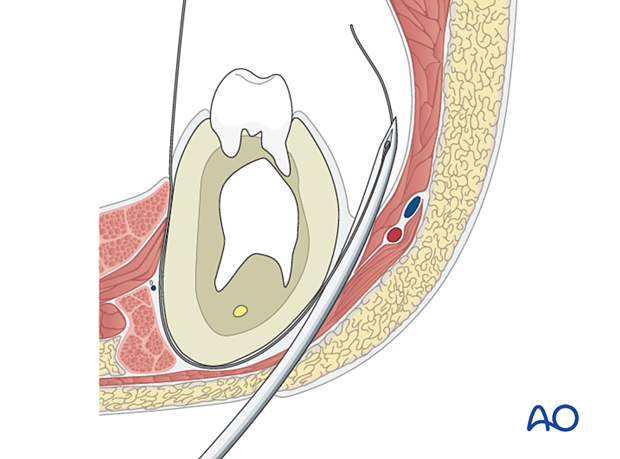
…and passed up to the other side of the mandible.
The two ends are tightened to secure the splint or arch bar.
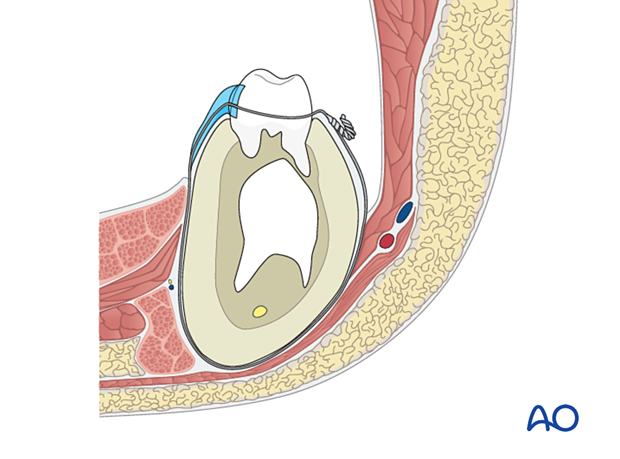
A minimum of two circummandibular wires are needed. More could be considered depending on the nature of the fracture
A minimum of two circummandibular wires are needed. More could be considered depending on the nature of the fracture
6. Aftercare following occlusal splints
Release of MMF and elastics (if MMF is used)
The patient should be instructed how to release the MMF in case of an emergency. Some surgeons prefer to provide wire cutters to the patient for the period of MMF. During this period, wire fatigue and loosening can occur. The patient should report any loosening of the MMF to the surgeon immediately.
As an alternative, the MMF may be achieved by using elastics instead of wires. With an adequate number of elastics, the same level of reliability can be reached minimizing the risk of inability to release the MMF during an emergency situation.
X-Rays
Postoperative x-rays are taken within the first days after surgery. In an uneventful course, follow-up x-rays are taken prior to releasing the MMF and removal of the splint.
Follow up
It will be necessary to see the patient approximately 1 week postoperatively to assess the stability of the occlusion and to check for infection of the surgical wound. The intermaxillary fixation wires or elastics must be assessed and proven to hold the patient tightly in occlusion. Patients also have to be periodically re-examined to rule out signs of infection. At each visit, the surgeon must evaluate the patient's ability to perform adequate oral cleaning. It may be necessary to provide additional instruction to assure appropriate hygiene and wound care.
Malocclusion
There should be no malocclusion detected as occlusion is determined and secured in the operating room.
Release of MMF and occlusal splint
On releasing the MMF and occlusal splint, physiotherapy can be prescribed. The mandible will be hypomobile after the period of MMF, and the muscles will be atrophic and “tight.” Opening and excursive exercises should be demonstrated and implemented. Goals should be set, and typically, 40 mm of maximum interincisal mouth opening should be attained by 4 weeks postoperatively. If the patient cannot fully open his or her mouth, additional passive physical therapy may be required.
Basic postoperative instructions
DietThe diet has to be in a liquid or semi-liquid form. For patients with a full complement of teeth, the diet must be more liquefied than when there are gaps with teeth missing. Because the diet will be no-chew, more fluids are required to assist in swallowing the food. A blender, or preferably, a juicer is useful. Anything can be made into a liquid or semi-liquid form with these tools. Liquid dietary supplements from the grocery store help maintain caloric intake. The patient should monitor their body weight on a weekly basis during the period of MMF to evaluate any dramatic changes.
Patients must be instructed in oral hygiene procedures. The presence of the arch-bars and MMF wires makes this a much more difficult procedure, and the inside of the teeth cannot be reached with a toothbrush. A soft toothbrush (dipping in warm water makes softer) should be used to clean the buccal/labial surfaces of the teeth, arch-bars and wires. Chlorhexidine oral rinses should be prescribed and used at least 3 times each day to help sanitize the mouth.
The patient should be warned to continue routine follow up with their dentist. Fractures near the dental roots can often result in delayed loss of tooth viability, requiring periapical films and additional dental procedures.













