Four stage forehead flap with radial forearm flap for lining
1. Introduction
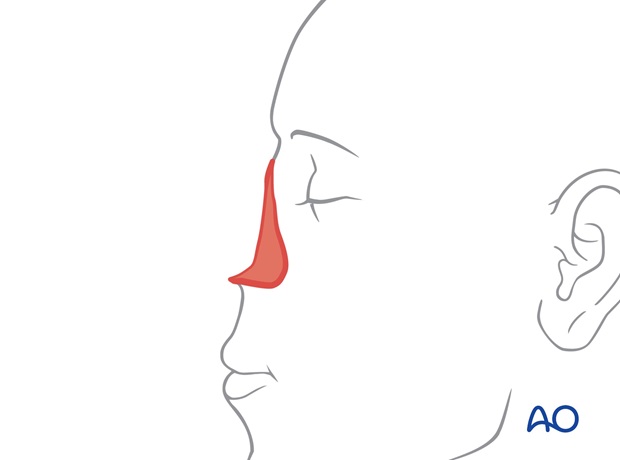
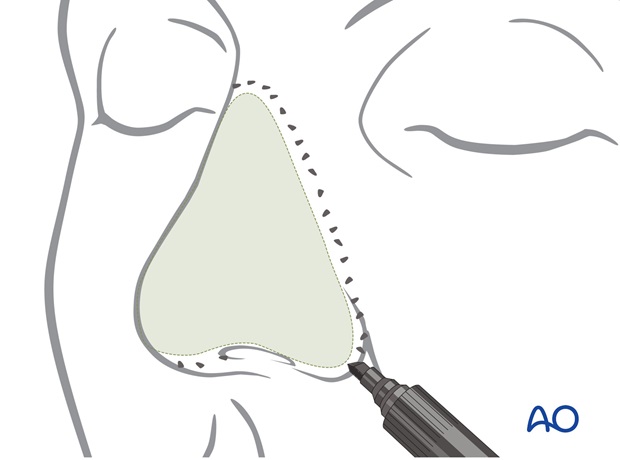
Nose surface
Single subunit defects (tip or ala) that require only modest skin resurfacing and limited cartilage replacement can be resurfaced with forehead skin transferred in two stages.
However, when a forehead flap in transferred in only two stages, it is not possible to alter the inferior nose, columella, or ala at the time of pedicle transfer without devascularization.
Large deep defects which encompass multiple nasal units and will require extensive replacement of cartilage support or nasal lining should be reconstructed with a full thickness forehead flap in three stages.
More details on nasal lining can be found here.
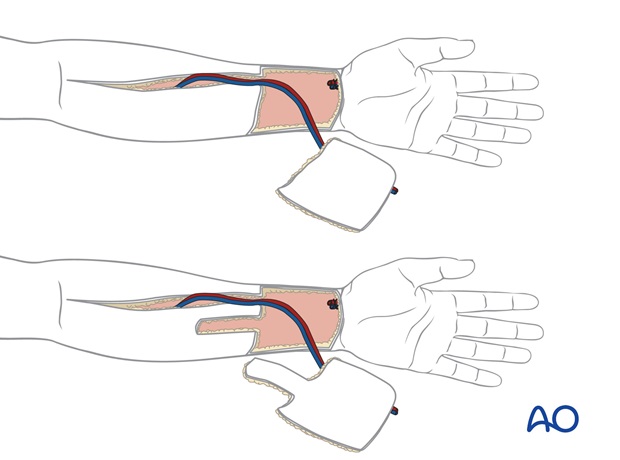
In subtotal and total nasal reconstructions lining will often be required for the vault, nasal floor, and columella. A radial forearm flap can provide a large area of relatively thin skin based on a long vascular pedicle.
The forehead is thicker than nasal skin and excessive subcutaneous fat and frontalis muscle must be excised to create a skin flap of a thickness similar to that of the missing skin of the nose. Although the excessive soft tissue can be excised at the time of harvest, in larger more complicated defects it is safer to thin the excess during an intermediate operation prior to pedicle division.
This improves vascular safety and aesthetic results. The intermediate operation allows the surgeon to re-elevate the flap completely and aesthetically contour the inferior nose by soft tissue excision and cartilage modification.
The advantages of a full thickness four stage flap are:
- Maximum vascularity at the time of transfer and at the intermediate second stage operation.
- The ability to create a uniformly thin supple skin flap.
- Staged soft tissue sculpture, primary and secondary cartilage grafting.
- The ability to correct previous intraoperative errors of judgments or imperfections of healing prior to pedicle division.
- Modified techniques to provide vascular lining as a folded distal flap extension or as a skin graft.
Nose lining
In subtotal and total nasal reconstructions lining will often be required for the vault, nasal floor, and columella. Frequently, the septum is absent.

Approximately 8 cm of lining is needed from one alar base across the tip to the other alar base to reline the vault.
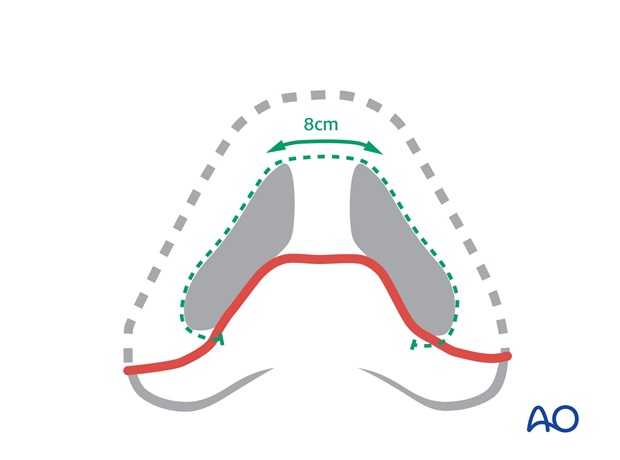
If missing, loss of the nasal floor pulls the upper lip inward by scar contraction. This must be replaced to reposition the lip. The nasal floor is part of the platform on which the nose sits.

The septum is not reconstructed but lining for the columella must be provided to create a soft tissue pocket in which a columella strut can be positioned.
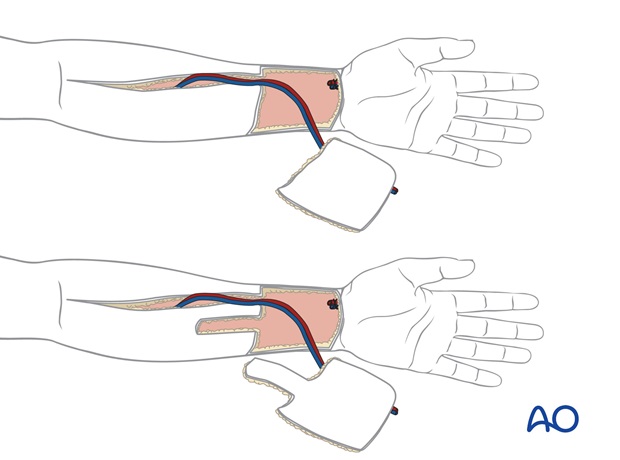
A radial forearm flap can provide a large area of relatively thin skin based on a long vascular pedicle. An approximately 8 x 7 cm skin paddle is marked on the distal volar forearm over the radial vessels.
An additional proximal skin extension is included if nasal floor lining is needed.
Principles of reconstruction
Each defect is different but each reconstruction is simplified because the "Normal" never changes so the principles of repair remain the same. The contralateral normal remains as a visible comparison. If the contralateral normal is unavailable, the ideal is used as a guide.
The face can be described in regional units characterized by:
- Skin quality
- Border outline
- 3 dimensional contour
The principles of nasal reconstruction which apply to large deep defect which will be resurfaced with a flap are:
- Recreate nasal subunits, not just fill the defect.
- Alter the wound in site, size and depth to improve the final result
- If appropriate, excise residual normal skin within the subunit to replace missing skin as a unit, rather than as a patch (subunit principle)
- Use the contralateral Normal or the Ideal as a guide
- Replace missing tissues exactly
- Employ surgical templates
- Build on a stable platform
Subunit principle: If a defect encompasses more than 50 % of a convex subunit – tip or ala - remaining normal skin is excised within the subunit and the entire subunit is resurfaced with a subunit flap. This positions final border scars in the junctions between adjacent subunits and harnesses flap trapdoor contraction and postoperative pin cushioning, and in combination with shaped underlying cartilage support, augments the shape of underlying cartilage support over the entire subunit.
Anaesthesia
This procedure is performed under general anaesthesia.
2. Preparation of template for nose resurfacing
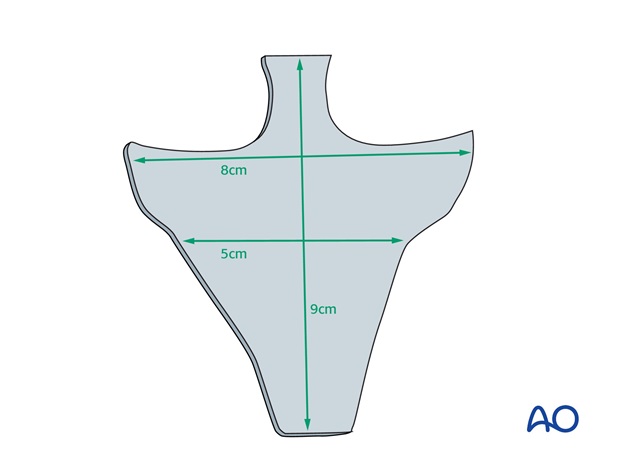
A universal pattern can be used to create a template with a basic nasal dimension and outline for the future forehead flap. Prior to use, it is crimped, bent, and trimmed to conform to the defect exactly.
3. Resection
If an initial excision is required to treat skin cancer, the tumor is excised utilizing standard excisional margins, verified by frozen section by the operating surgeon or the operating Mohs surgeon.
4. Stage 1: Microvascular lining transfer
Flap harvest
The forearm flap is designed as a single paddle and with a proximal extension if lining for the nasal floor is needed to release contraction of the lip.
It is harvested in a standard fashion, transferred to the face and anastomosed to the facial or cervical vessels.
Dorsal support
As the septum is largely absent, a rib graft is positioned as a cantilever graft to project from the remaining radix and nasal bone. This is fixed with one or more screws to the residual nasal bones.
Primary cartilage grafts for the columella, tip, or ala support are not placed at this time.

The dorsal graft may also be supported by a fixation plate.
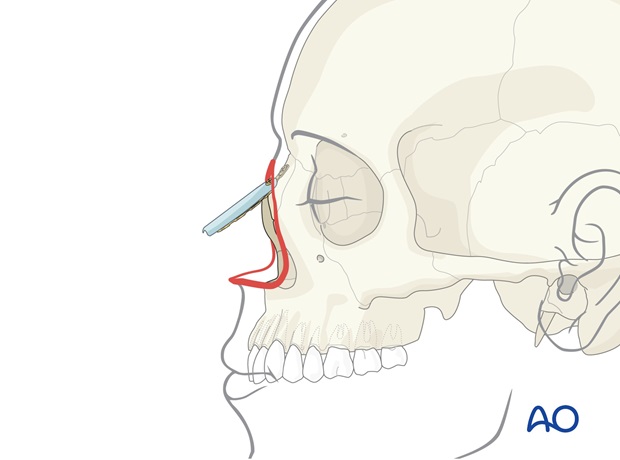
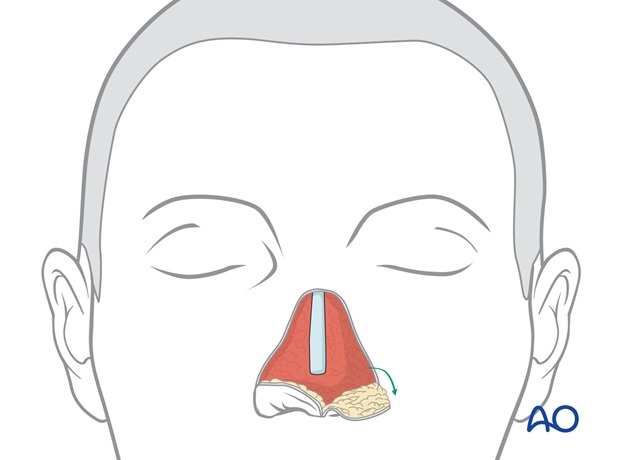
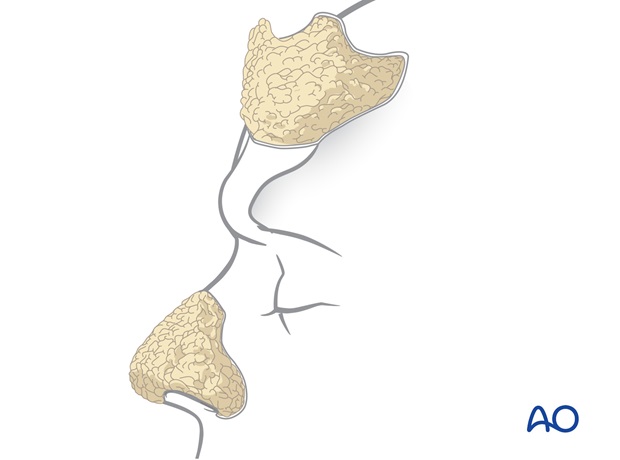
The thin distal ulnar border of the flap is folded inwards to create lining for the vault and columella.
If necessary, the contracted scar within the injured nasal floor is released and the additional skin extension transferred to fill the deficiency.
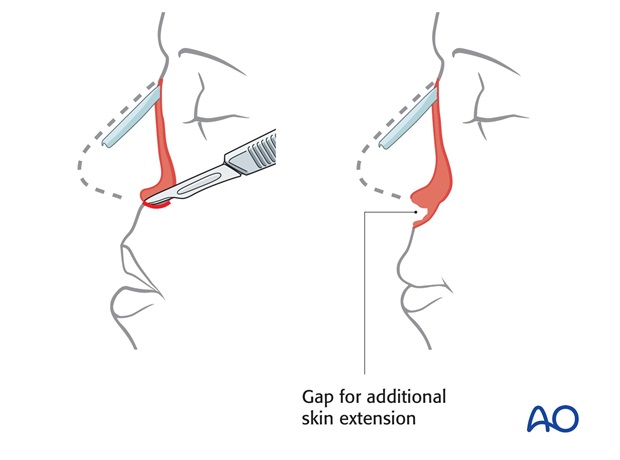
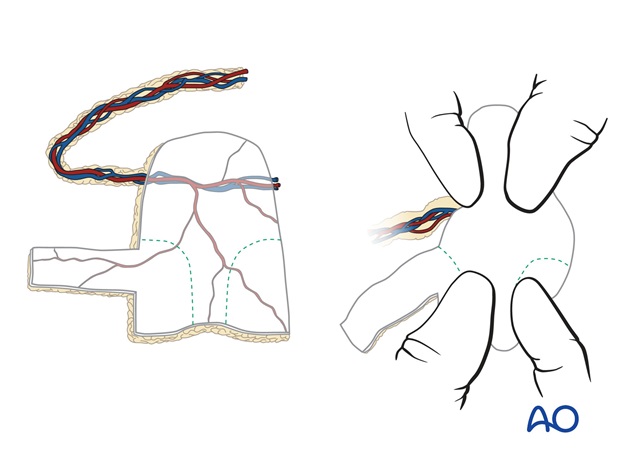
The proximal external skin with the vascular pedicle is turned back over the lining to envelope the dorsal rib graft. The radial vessels are located at the proximal external skin component of the paddle.

5. Stage 2a: Excision of external skin
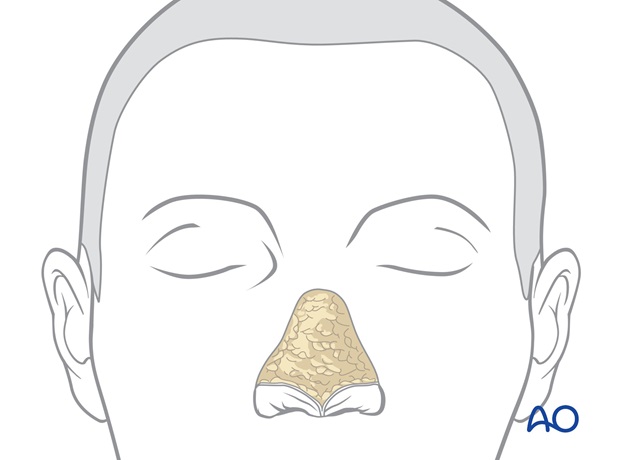
Two months later after resolution of edema and flap healing, the preliminary folded "neo nose" is additionally vascularized by its inset on the face, but remains incompletely supported and shaped by cartilage grafts, and its external skin surface does not match the facial skin in colour and texture. Minor imperfections in nostril margin position and alar base inset will be apparent.
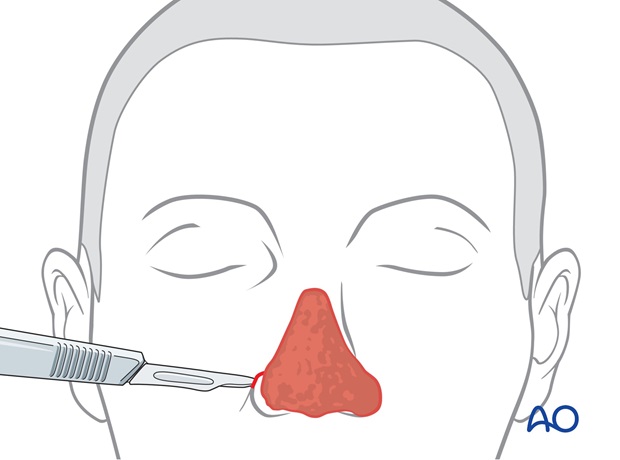
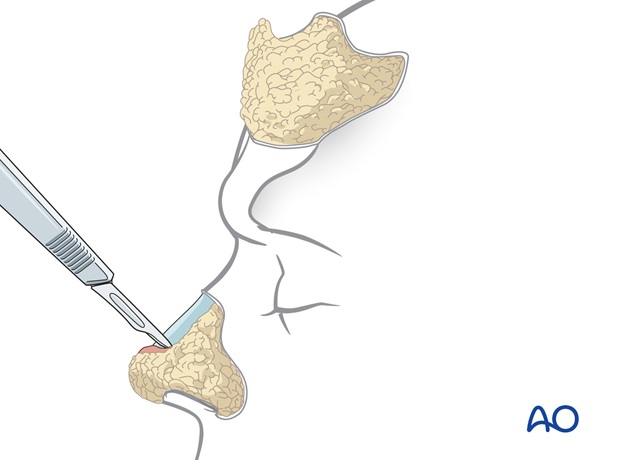
The external flap skin is incised and the flap is elevated with 2-3 mm of subcutaneous fat towards the proposed nostril margin.
Underlying bulky forearm subcutaneous fat and fascia are discarded.
The radial vessels originally supplying the external skin component of the forearm flap are now adherent to the underlying forearm lining and will continue to vascularize the lining after elevation of the external skin.
Before discarding the excess of external skin, it can be hinged over to reposition the nostril margins and adjust the alar base inset.
6. Stage 2b: Delayed cartilage support
Excision of residual skin
If a subunit excision is planned, residual normal skin within remaining subunits is excised.
The cartilaginous and bony framework of the nose is enveloped by the external covering skin and internal lining. This framework supports and shapes soft tissues and braces a reconstructed nose against gravity, tension, and scar contraction. If missing, nasal support must be replaced. The dimension, border outline, and shape of these bone and cartilage support grafts will re-establish the normal nasal contour.
The choice of donor material will depend on the needs of the defect:
- Graft size
- Graft shape
- Graft rigidity
Septal cartilage is straight but of limited length and thickness.
Ear cartilage is relatively soft, curved, but limited in availability.
Rib cartilage is available in large quantity, thickness, and rigidity, but can be shaved into thinner more bendable strips with suture material. In cases requiring a forearm flap for lining, all support grafts will be constructed with rib cartilage.
Grafts are fixed with sutures to remaining nasal support structures and fixed to one another to recreate a rigid nasal framework to support and shape the nose.
Tip reconstruction
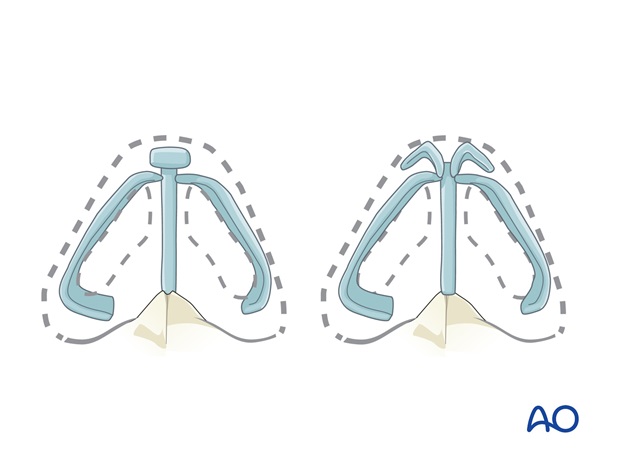
The volume, dimension, and contour of the tip subunit depend on the underlying cartilage framework.
Each component must be reconstructed to support, shape and brace the reconstructed tip postoperatively
Rib cartilage is used to reconstruct the medial and lateral crura.
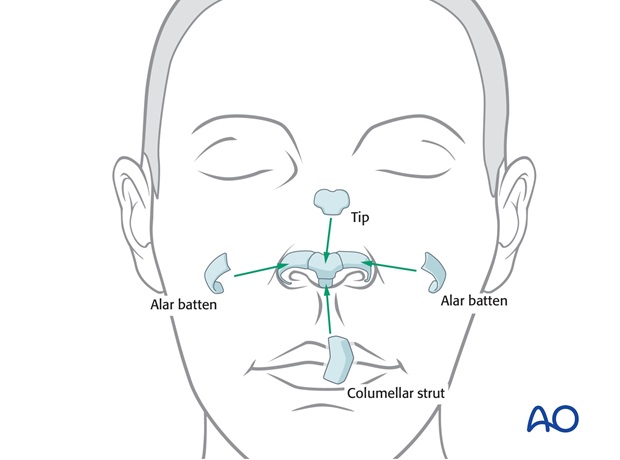
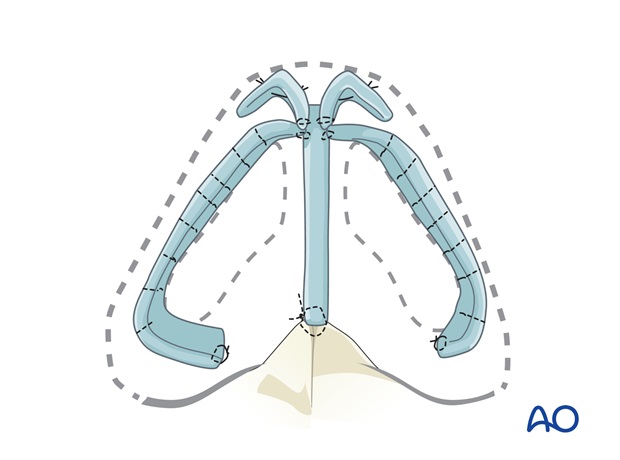
A columellar strut is fixed to the nasal spine and sutured to the tip off the dorsal graft. Tip volume, projection, and definition are rebuilt with a Peck graft. Alar margin Batten grafts support the shape of nostril margins, their preparation and insertion is shown below.
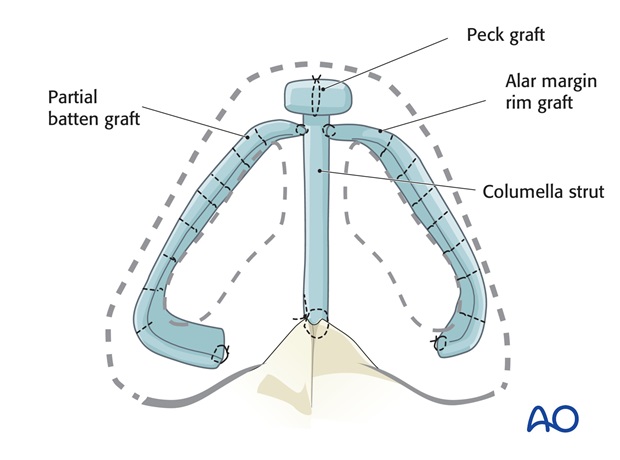
Alternatively, the tip can be rebuilt with anatomically shaped tip grafts – middle and lateral crura replacements of rib cartilage that are bent with sutures to mimic the normal anatomy.
Alar reconstruction
Normally the ala contains no cartilage, but an alar rim is now supported with a delayed primary alar batten support graft to support, shape and brace the reconstructed ala postoperatively.
Rigid rib graft is shaved in thin strips which are bent with horizontal mattress sutures.
The rib cartilage graft is guided into a pocket at the alar base with percutaneous quilting sutures laterally and the medial edge of the graft is sutured to the columella strut and the underlying forearm lining surface.
Sidewall support
A side wall bracing graft is placed to support and shape the lateral nasal wall, maintain the airway, and prevent retraction of the ala superiorly.
The graft extends from the pyriform aperture anteriorly to the central dorsal support and inferiorly to the alar crease. It is fixed with sutures to these support structures.
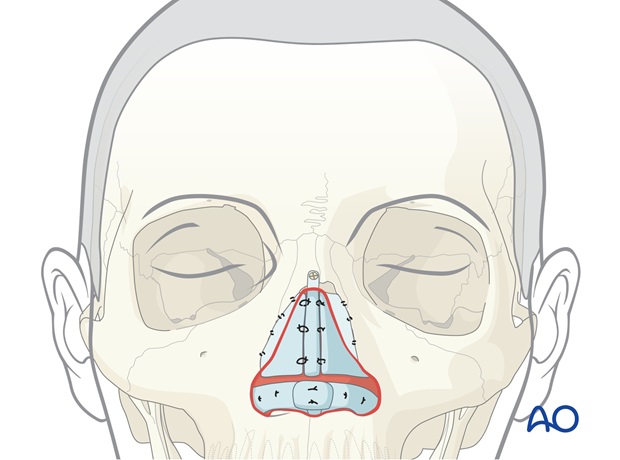
7. Stage 2c: Transfer of a paramedian forehead flap
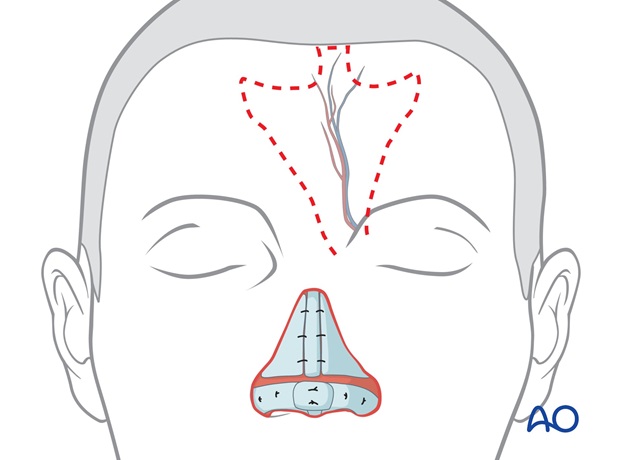
Outline of paramedian forehead flap
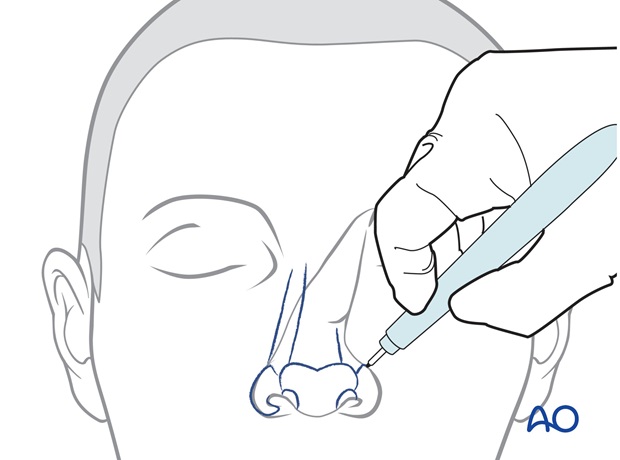
The template is positioned under the hairline directly superiorly to its supratrochlear pedicle, which is located a few mm lateral to the frown crease (verified by doppler).
The outline and the dimension of the flap will be designed to resurface parts or all of the dorsum, tip, and ala depending on the defect.
The paramedian flap is perfused by the supratrochlear vessels and can be based on either side of the forehead. Unilateral defects are more easily resurfaced with the ipsilateral flap because its pedicle is closer to the defect.
Either the right or left pedicle can be chosen for midline defects.
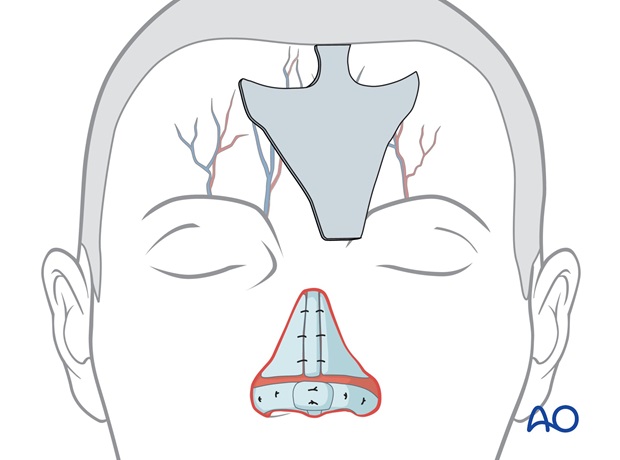
Centered over the left (or right) supratrochlear vessels, the flaps pedicle is drawn inferiorly through the medial eyebrow, narrowing to 1.2 to 1.5 cm in width at the pedicle base.
The border of the flap is incised, elevating the flap from distal to proximal over the periosteum to its pedicle base, with the underlying tissues and frontalis muscle, as a full thickness flap without thinning.
This maintains the skin vascularity through the deep dermis, frontalis muscle and axial supratrochlear vessels.
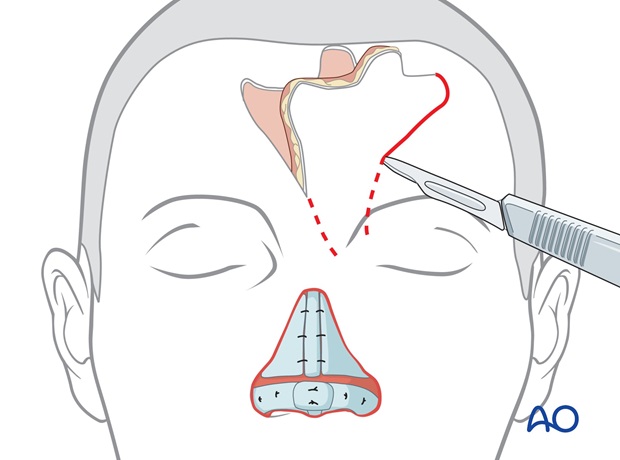
The flaps base is incised through the medial eyebrow separating the corrugator muscle until it can be rotated medially to cover the nasal defect without tension.

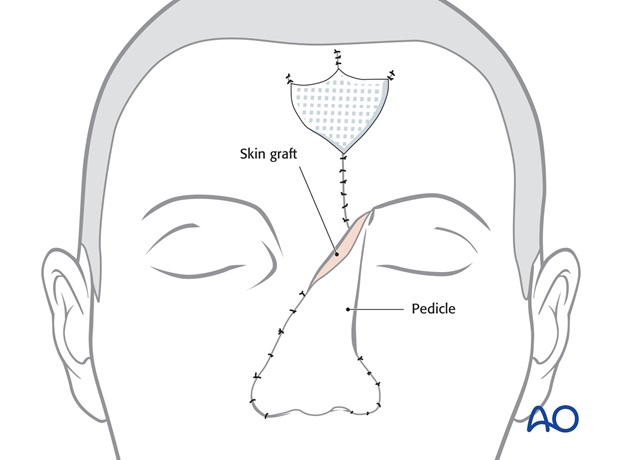
Closure of donor site defect
The forehead defect is closed in layers after wide undermining and excision of the "scalp dog ear".
If the superior aspect of the defect cannot be closed primarily, it is allowed to heal secondarily over several weeks. The open area is covered with a petrolatum gauze for one week.

Flap inset
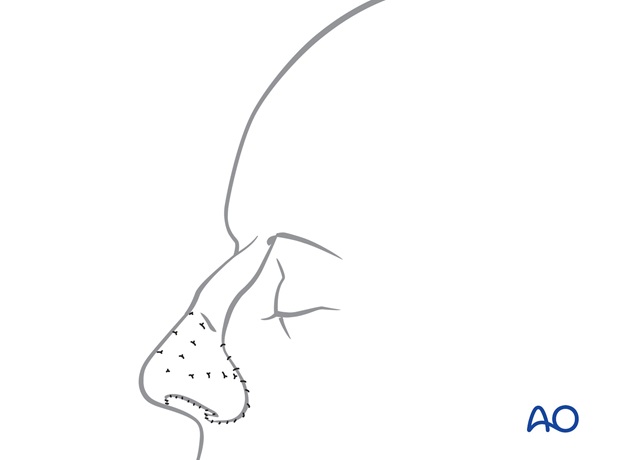
The forehead flap is sutured into the recipient site with a single layer of sutures.
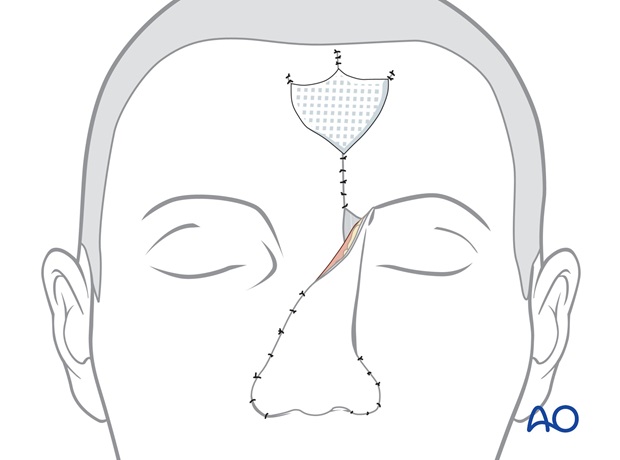
A full thickness skin graft harvested from the groin is placed on the raw deep surface of the pedicle for cleanliness.
8. Stage 3: Thinning of the flap
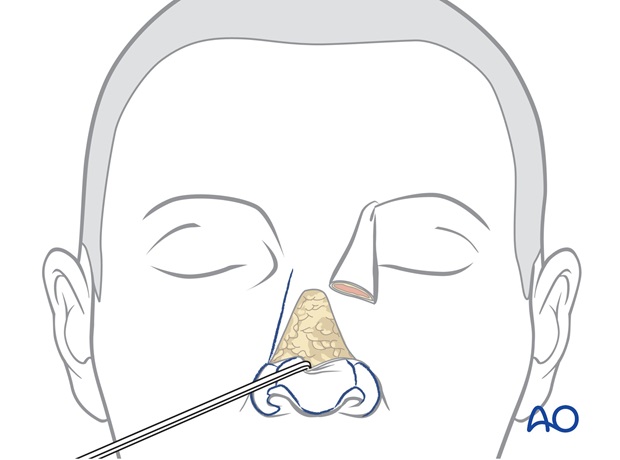
One month later the bulky flap has healed to the recipient site. Because of its elevation and rotation it is effectively physiologically delayed, augmenting its blood supply.

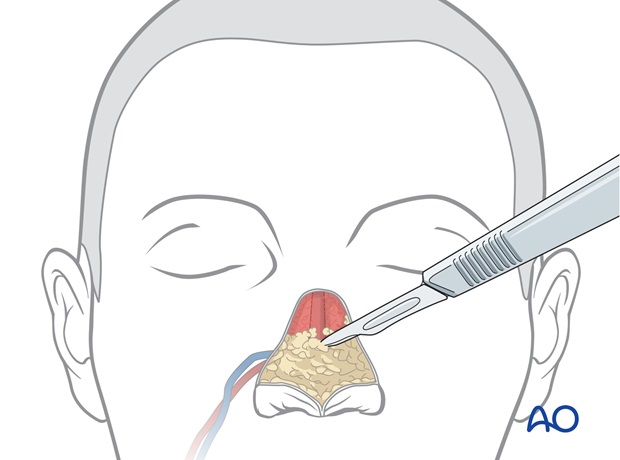
The borders of the flap are incised and the flap is completely elevated off the recipient site with 2-3 mm of subcutaneous fat, creating a uniformly thin skin flap for nasal cover.
Underlying excess subcutaneous fat and frontalis muscle are completely exposed and are excised to debulk the nose and sculpt a nasal shape into the previously transferred tissues.
Old cartilage grafts can be removed, reshaped or repositioned as necessary to improve the hard tissue framework. An imperfectly designed or malpositioned graft can be revised or additional grafts added for shape or projection.
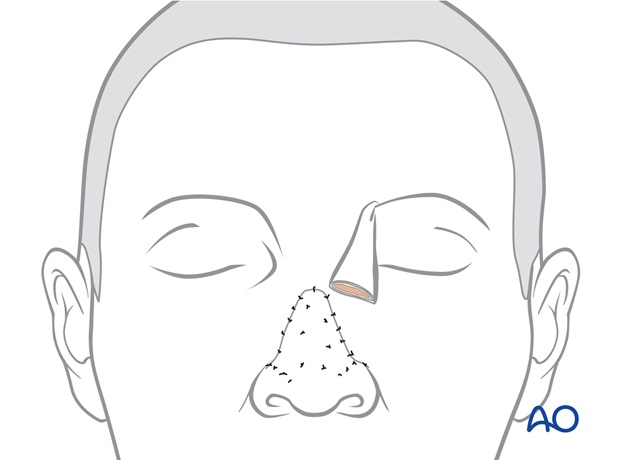
The thin skin flap is returned to the recipient site fixing its cutaneous surface to the underlying bed using percutaneous quilting sutures and its peripheral borders with single layer skin sutures.
9. Stage 4: Pedicle division
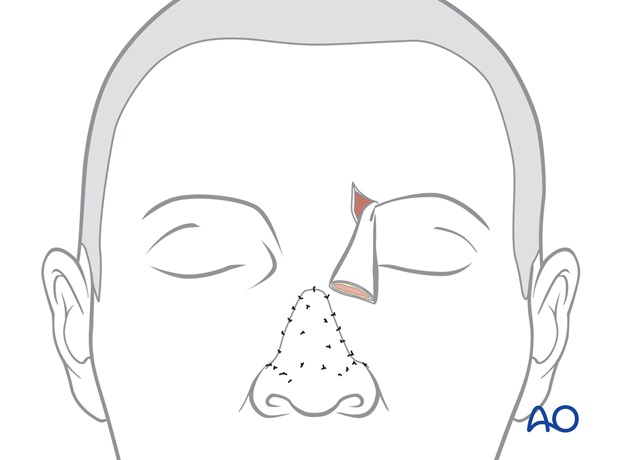
The site of pedicle division is marked, leaving excess tissue that can be trimmed at the time of fine tuning the reconstructed subunit.
The site of pedicle division is outlined.
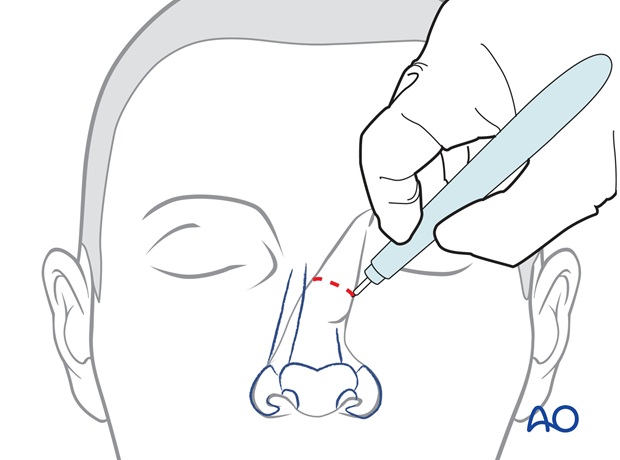
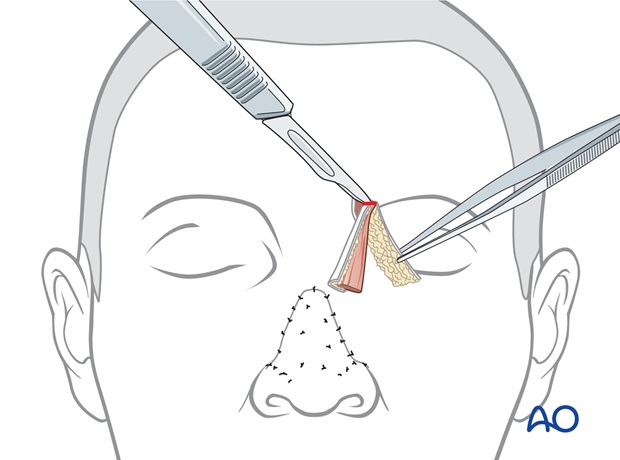
The pedicle is divided. The skin of the nasal inset is elevated with 2-3 mm of subcutaneous fat over the superior aspect of the reconstructed nose.
Trimming
A forehead flap can be extensively re-elevated towards the nostril margin and the columella inset. Because the operation is performed under general anaesthesia without local anaesthesia, the flaps colour and capillary refill can be evaluated.
Underlying subcutaneous fat or excess cartilage over the superior nose is excised to sculpt the sidewall dorsal contour and deepen the alar crease.
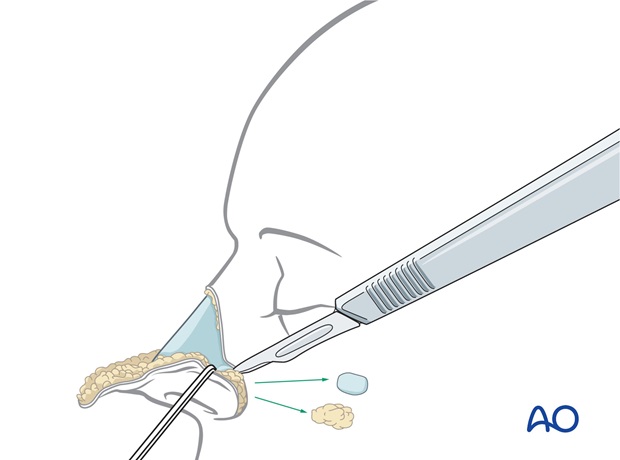
Excess forehead skin is trimmed and the forehead skin inset with percutaneous quilting sutures and a single layer skin closure.
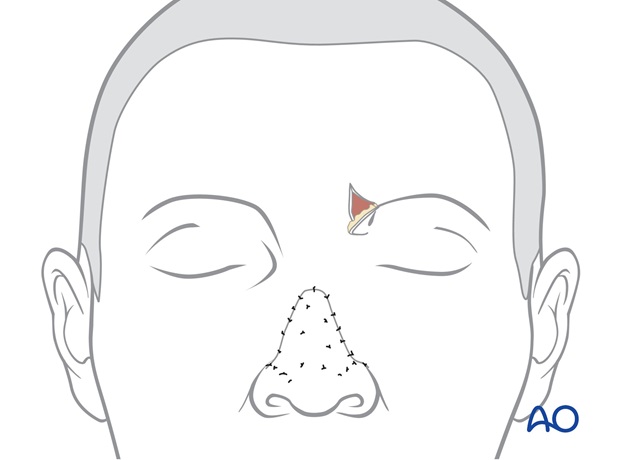
Forehead closure
The inferior part of the forehead scar through the medial eyebrow is reopened.
The skin of the proximal forehead pedicle is elevated with several mm of subcutaneous fat from the underlying excess soft tissue and previous skin graft of the proximal pedicle. The excess underlying soft tissue bulk is excised.
The skin of the proximal pedicle is trimmed, returning the medial eyebrow to its normal position and inset as a small inverted V whose scars simulate the normal frown crease.
It is fixed in place with a temporary quilting suture and a layered skin closure.
Revision surgery
Almost all major nasal reconstruction will require a revision procedure four months after the initial reconstruction to improve the final result.

Case
Pre-and postoperative photographs of a large full thickness defect repaired with a four stage forehead flap with radial forearm flap for lining

10. Aftercare following nose reconstruction
Skin graft
The bolus skin graft dressing should be kept dry. The forehead donor site can be washed within 24 h.
Forehead nasal reconstructions
Routine showering is permitted within 24 hours of all surgical sites. Dressings are worn at the discretion of the patient.
Quilting sutures are removed after 48h. Routine skin sutures are removed after 7 days. Sun exposure is avoided for several months after surgery.













