Lining
1. Introduction
A full thickness defect will require replacement of missing lining, which must be thin and supple enough to conform to the overlying cartilage framework, without occluding the airway.
Traditional lining methods are:
- Prelamination or prefabrication
- Folding of the forehead flap for cover and lining
- Hinge over lining flaps
- A second flap for lining
- Intranasal lining flaps
- Skin grafts for lining
- Microvascular lining replacement with distant tissue
A general discussion on the different options is provided below as well as more details on the intranasal lining flaps.
The use of a folding flap as well as the use of microvascular lining replacement with distant tissue is described in detail in the section on full thickness defects.
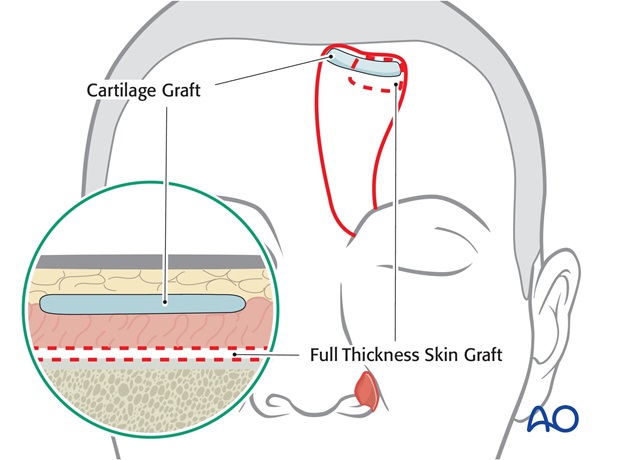
2. Prelamination or prefabrication
During a preliminary operation a composite skin/cartilage graft or a strip of cartilage with a full thickness skin graft are positioned under the distal forehead flap to replace lining for the alar rim.
The disadvantages include the need for a preliminary operation delaying the reconstruction, the unreliability of skin graft take, the limited cartilage support, and the difficulty of designing a three dimensional nose on the flat surface of the forehead prior to transfer of the flap. Although limited in use, it may be considered in an elderly ill patient unable to tolerate a more complex reconstruction under general anaesthesia.
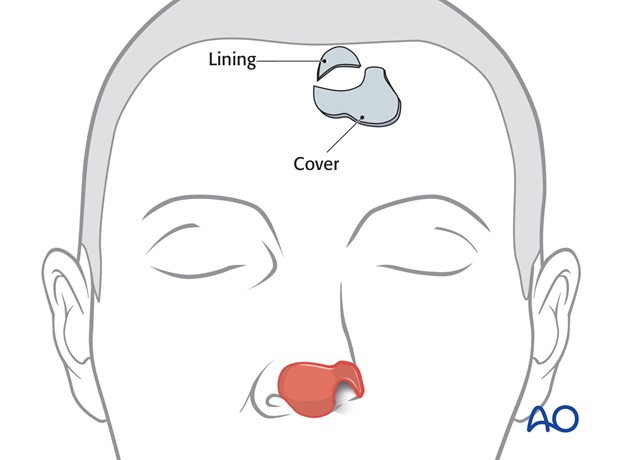
3. Folding of the forehead flap for cover and lining
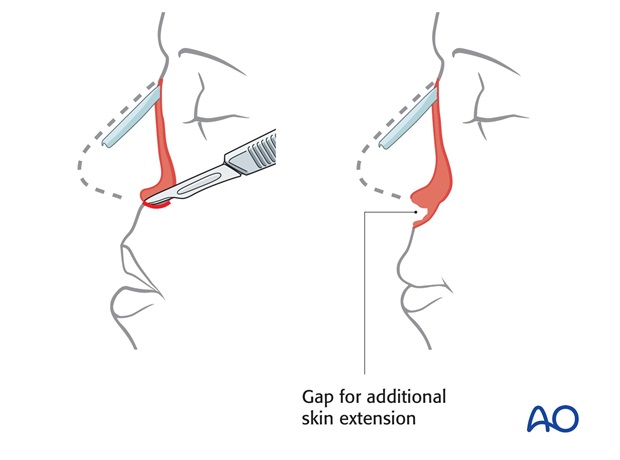
Additional skin can be added to the distal end of a forehead flap and folded upon itself to provide lining.
Traditionally, this precluded the placement of significant cartilage support and contour. The folded technique can be modified to overcome these limitations. This is the technique most commonly used by the author.
4. Hinge over lining flaps
When the full thickness of the nose is missing, the wound along the remaining nose can be allowed to heal secondarily with or without additional skin grafting to the external nasal surface. Once healed along the wound margin, the remaining external nasal skin, skin graft or scar can be hinged over along the rim of the defect like the page of a book to fill the lining defect. These turnover random flaps are vascularized along the healed initial wound margin.
The disadvantages of hinged over lining flaps include the delay required to permit the initial healing to cover the lining, unpredictable vascularity (especially if large or within a radiated field) and often associated airway stenosis created by scar contracture at their base.
Hinge over flaps are useful if limited in size or length and the residual nasal airway remains open.
5. A second flap for lining
A nasolabial, second forehead flap or facial artery myo mucosal (FAMM) flap can be transferred for nasal lining.
Because of their thickness and donor morbidity, these techniques are infrequently utilized. For additional information regarding thsese techniques, please refer to literature.
6. Intranasal lining flaps
Residual normal intranasal lining may remain after nasal injury. Based on their axial blood supply, remaining mucosa from the septum and lateral nasal wall can be transferred to replace missing lining.
The disadvantages of intranasal lining flaps include limited size and reach, risk of necrosis especially in the previously operated or traumatized nose, and lining retraction.
Although valuable techniques, the modified folded lining method is more commonly used.
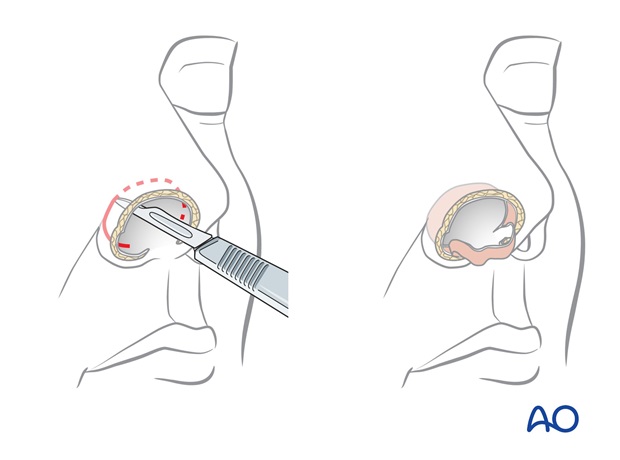
Bipedicle squamous skin flap
A bipedicle flap of residual stratified squamous skin within the remaining nasal vault can be incised along the intercartilaginous line and positioned inferiorly to line the reconstructed nostril margin. This technique is used if only a few mm of lining is missing along the nostril margin. (This avoids reconstructing the nostril margin with more easily traumatized intranasal mucosa).
The bipedicle donor site defect is filled with a skin graft or ipsilateral septal flap for lining.
Cartilage grafts are added to support the new nostril margin.
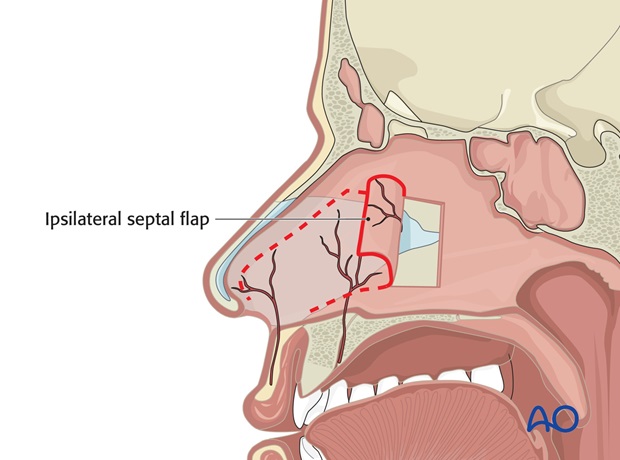
An ipsilateral flap, supplied by the septal branch of the superior labial artery, can be designed on a 1.5 cm base positioned over the nasal spine and can be rotated laterally to line the lateral nasal vault and nostril rim.
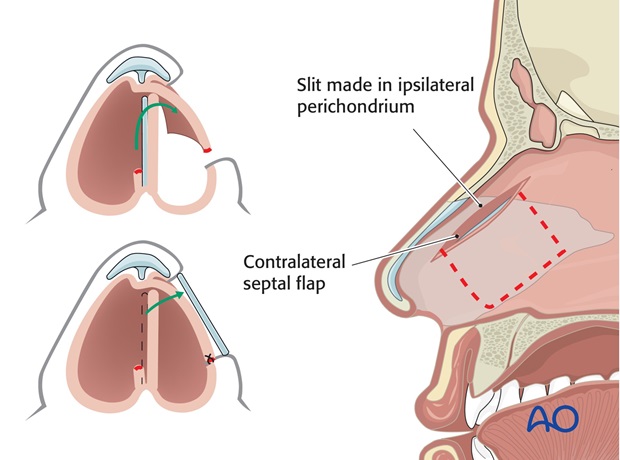
A contralateral septal flap, vascularized by the anterior ethmoid artery and based on the dorsal septum can be turned laterally to line the nasal side wall.
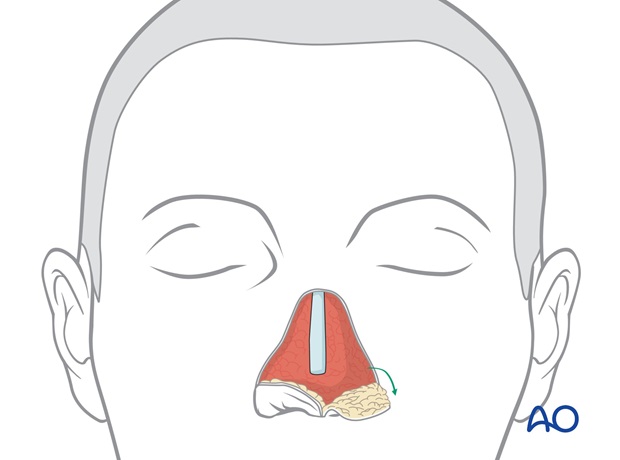
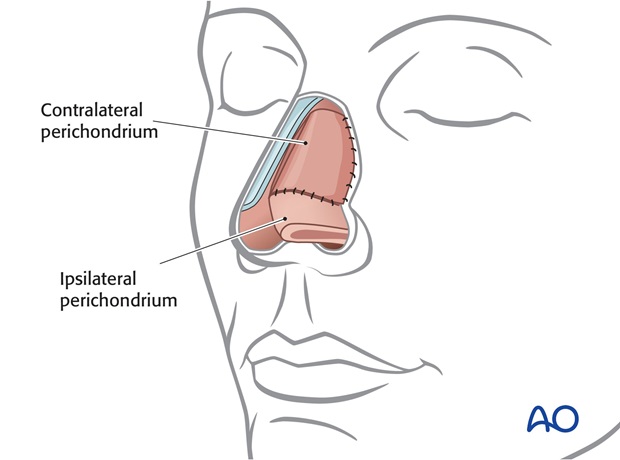
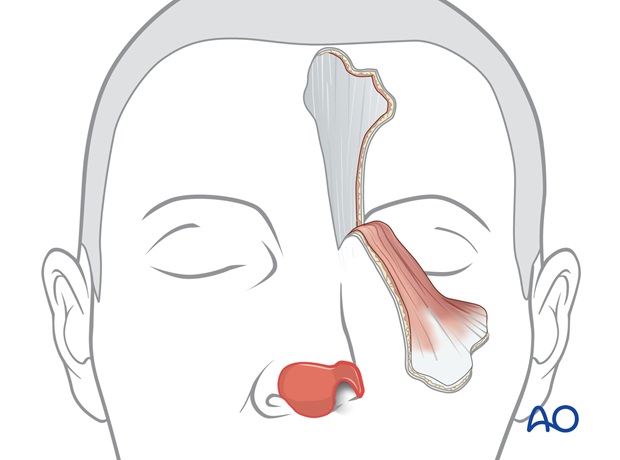
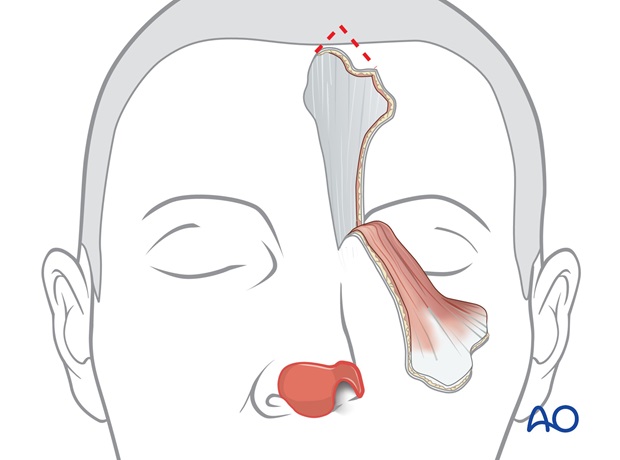
Combined ispsi- and contralateral septal flap
Most often an ipsilateral and contralateral flap are combined to line a unilateral defect of the ala and side wall.
The ipsilateral septal flap is elevated off the cartilaginous septum and swung laterally to provide lining for the nostril margin.
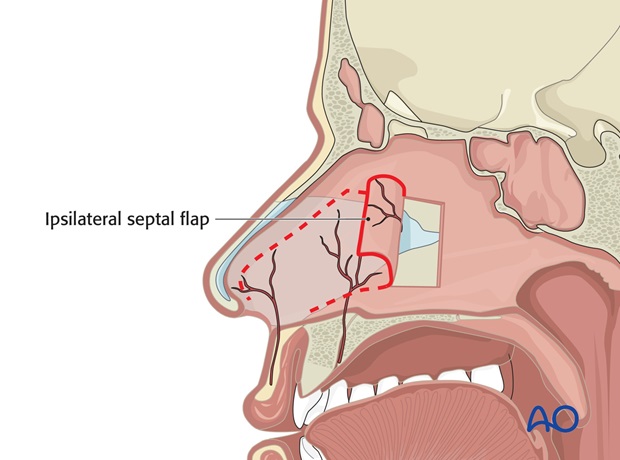
This exposes the underlying septal cartilage which is removed centrally as in a submucosal resection, leaving a 1.5 cm dorsal and septal "L" to support the dorsum and caudal septum.
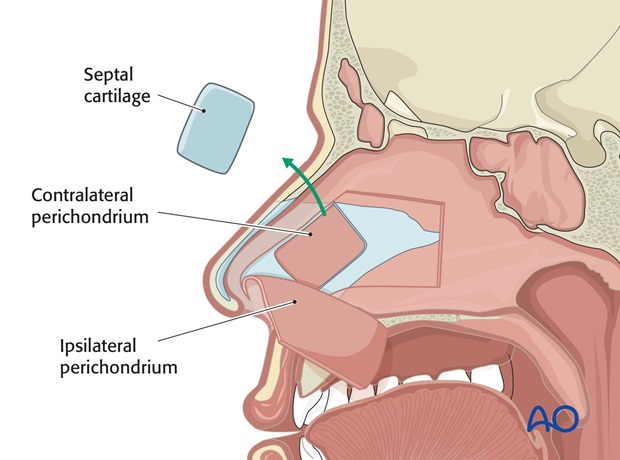
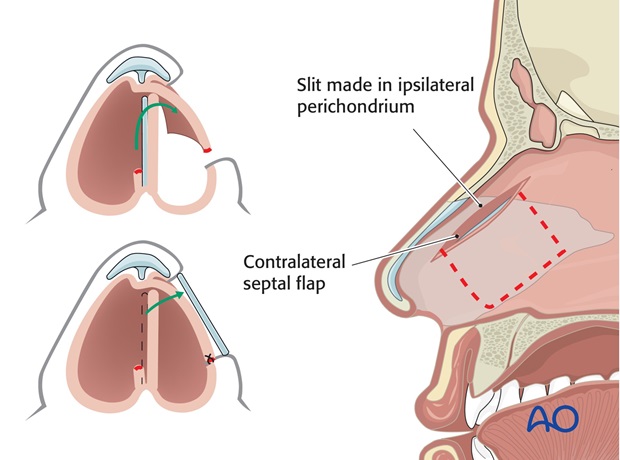
The contralateral septal mucosa is now visible and is incised as a U shaped flap, based dorsally on the bridge and supplied by the superior ethmoidal arteries.
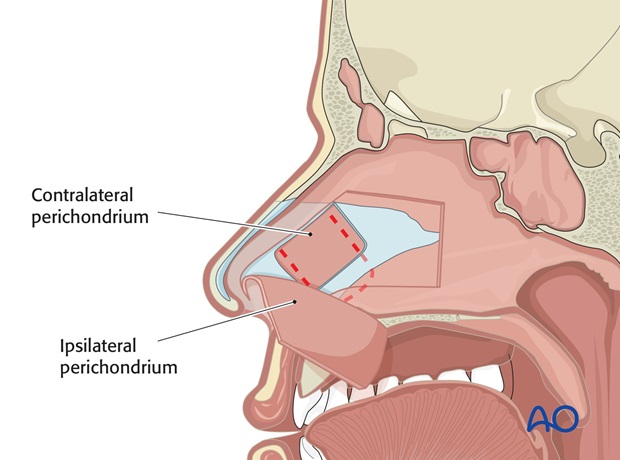
This is swung laterally through the surgically created septal fistula to line the remaining nasal sidewall defect. The two flaps are then sutured together and to the periphery of the defect to create a complete lining/sleeve.
If the ala remains intact, and lining is only required for the side wall, the ipsilateral septal lining is left in place. The contralateral flap can be elevated, the septal cartilage removed and, the contralateral lining flap passed through a slit in the ipsilateral intact lining which parallels the dorsum.
The harvested septal cartilage is later used as a side wall support graft.
Pre-and postoperative photographs of a full-thickness defect repaired with a 3 stage forehead flap, cartilage grafts, and ipsilateral and contralateral septal intranasal lining flaps.

Composite septal flap
A composite septal flap, containing the right and left septal mucosa and septal cartilage can be pivoted forward based on bilateral septal branches of the superior labial artery to supply central nasal support and a small amount of nasal vault lining.
This is applicable when significant amount of septum remains within the pyriform aperture.
In midline or subtotal nasal defects, the entire septum is incised under the nasal dorsum, along the nasal floor and vertically deep within the nose.
The right and left septum mucosa must be separated at the nasal spine and a small amount of septal cartilage excised to allow the composite flap to be swung anteriorly on a 1.5 cm soft tissue mucosal pedicle based only on right and left septum mucosa.

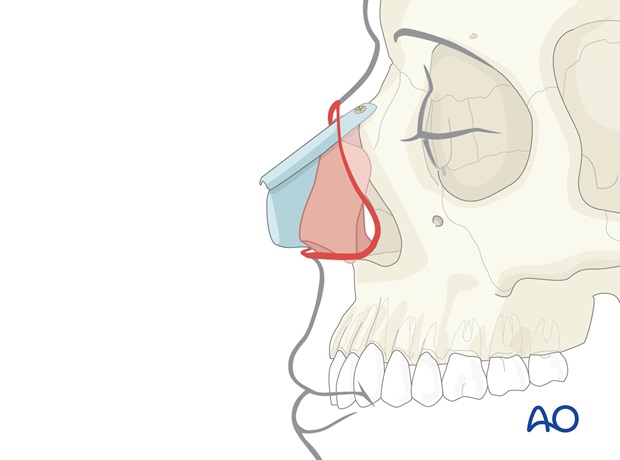
Once advanced, the flap is fixed with a suture or wire to the remaining nasal bones.
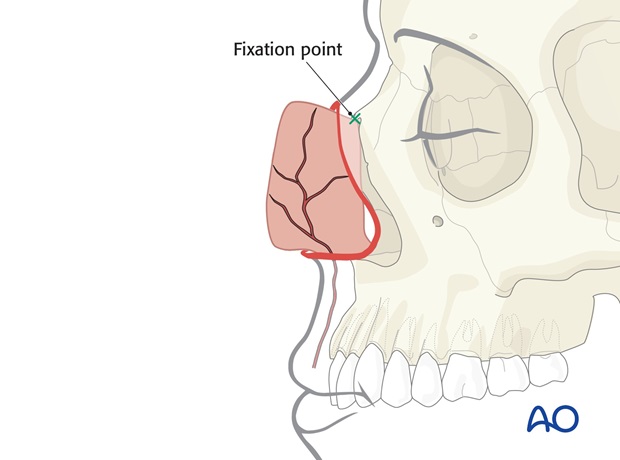
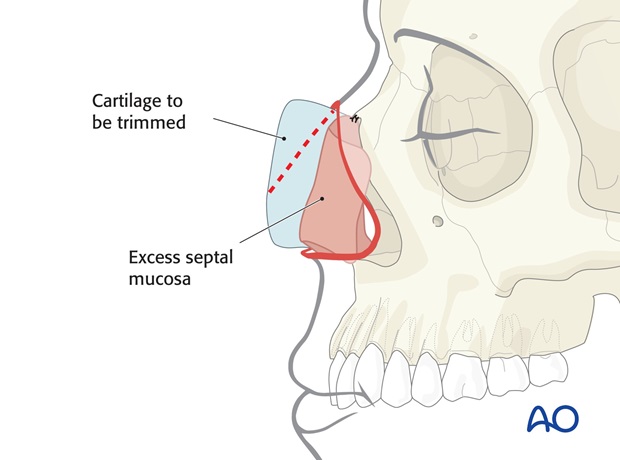
Excess septal mucosa along the dorsal leading edge can be swung laterally to fill small side wall and vault lining defects.
The leading edge of the septum is trimmed to establish the appropriate dorsal height.
In such complex cases, an additional dorsal rib graft will be fixed as a cantilever to the nasal bones to provide final dorsal support and shape.
A septal composite lining flap is inadequate in size to line the ala. Additional lining for the lateral nose must be provided by a delayed hinge-over skin flap from the residual alar remnant if intact or with a nasolabial flap.
Pre-and postoperative photograph of a subtotal nasal defect repaired with a 3 stage forehead flap, rib cartilage grafts and composite septal flap lining.

7. Skin grafts for lining
A skin graft will take on the raw surface of the forehead flap but traditionally, this precluded the placement of cartilage support. The skin graft method can be modified to overcome these limitations. Although an option to restore small areas of missing lining, the folded flap technique is more reliable.
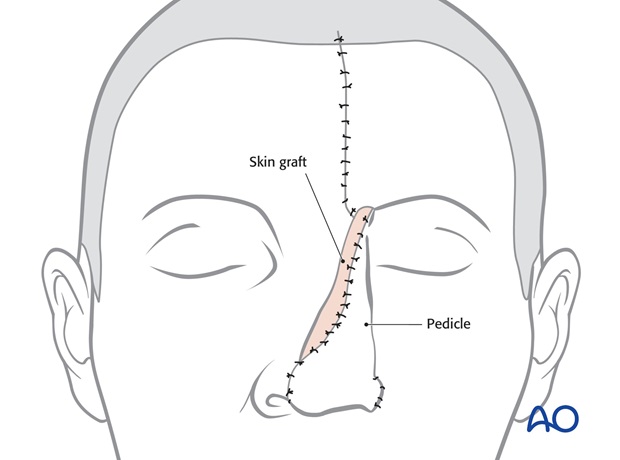
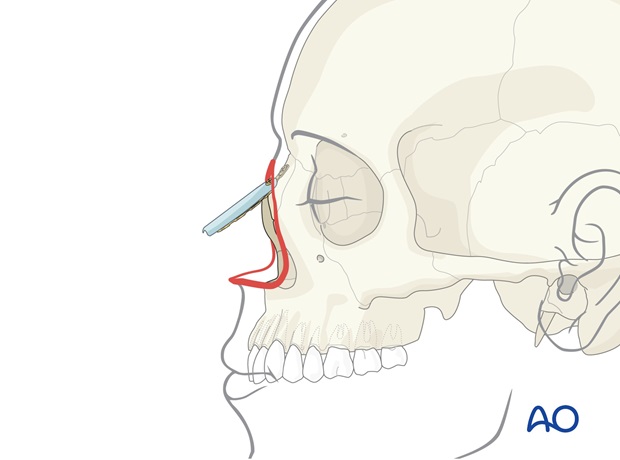
8. Technique: Folded flap
Unilateral or bilateral full thickness defects of the distal nose up to 2 – 2-5 cm in height can be lined by folding the distal end of a forehead flap. This permits a forehead flap to both provide external skin cover and internal lining.
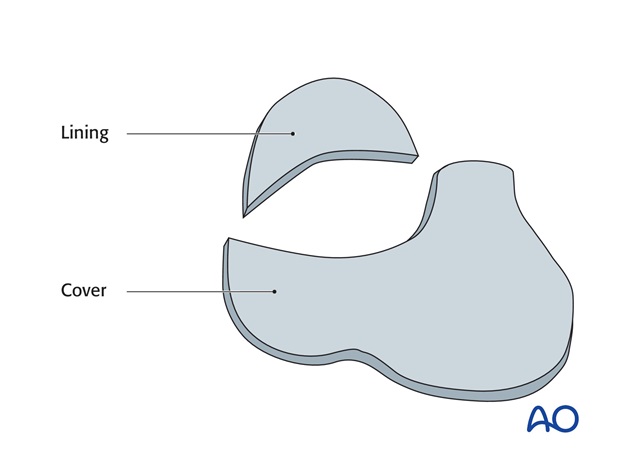
If significant parts of the nose remain, a template can be made of the remaining contralateral normal nose.
A second pattern is made of the lining defect.
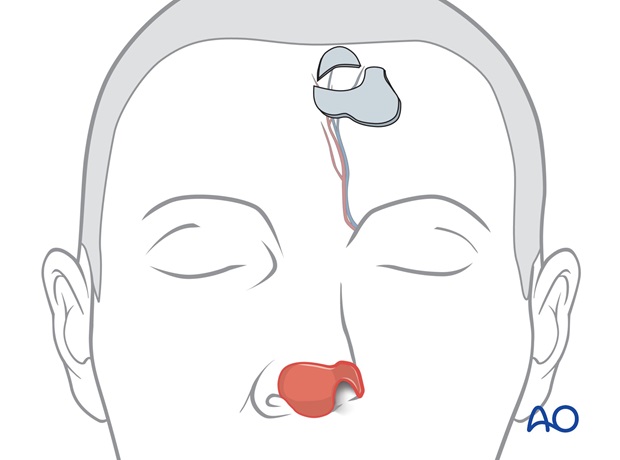
The templates are positioned under the hairline directly superiorly to its supratrochlear pedicle, which is located a few mm lateral to the frown crease (verified by doppler).
The lining template is oriented as a distal skin extension of the cover flap, carefully positioning it along the proposed nostril margin in the area of the lining deficiency. If lining is missing along both nostril margins, lining extensions are designed bilaterally.
The outline and the dimension of the flap will be designed to resurface parts or all of the dorsum, tip, and ala depending on the defect.
The paramedian flap is perfused by the supratrochlear vessels and can be based on either side of the forehead. Unilateral defects are more easily resurfaced with the ipsilateral flap because its pedicle is closer to the defect.
Either the right or left pedicle can be chosen for midline defects.
The lining pattern must be carefully marked so that when distal forehead flap is folded into the lining defect, the skin for lining will be correctly oriented.
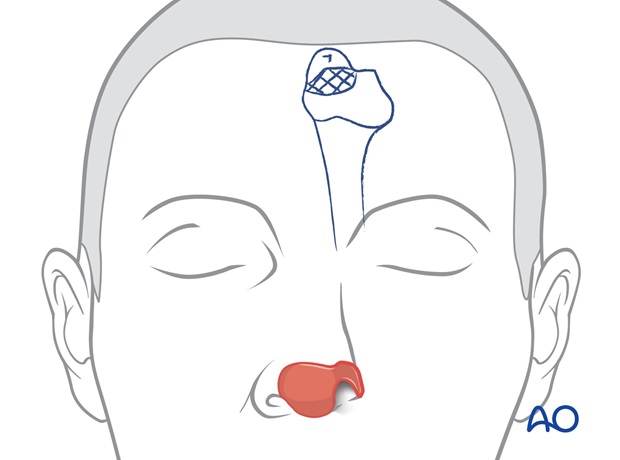
Centered over the supratrochlear vessels, the flap's pedicle is drawn inferiorly through the medial eyebrow, narrowing to 1.2 to 1.5 cm in width at the pedicle base.
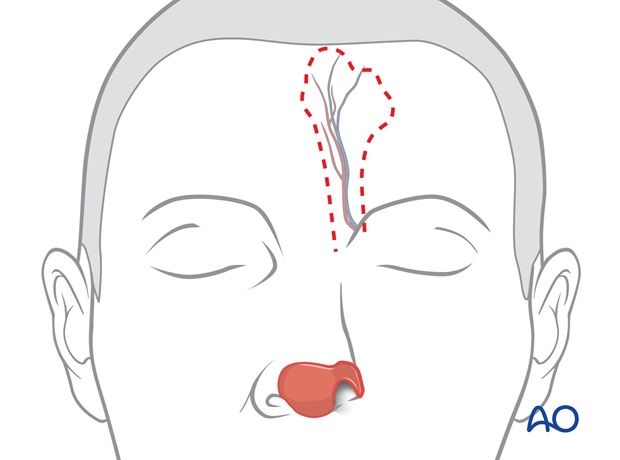
The border of the flap is incised, elevating the flap from distal to proximal over the periosteum to its pedicle base, with the underlying tissues and frontalis muscle, as a full thickness flap without thinning.
This maintains the skin vascularity through the deep dermis, frontalis muscle and axial supratrochlear vessels.
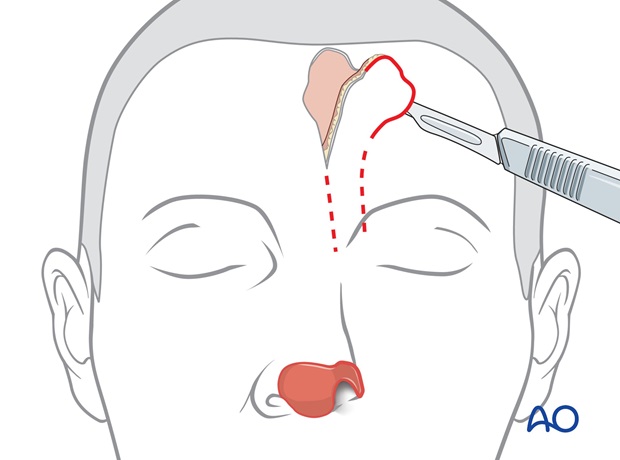
The flaps base is incised through the medial eyebrow separating the corrugator muscle until it can be rotated medially to cover the nasal defect without tension.
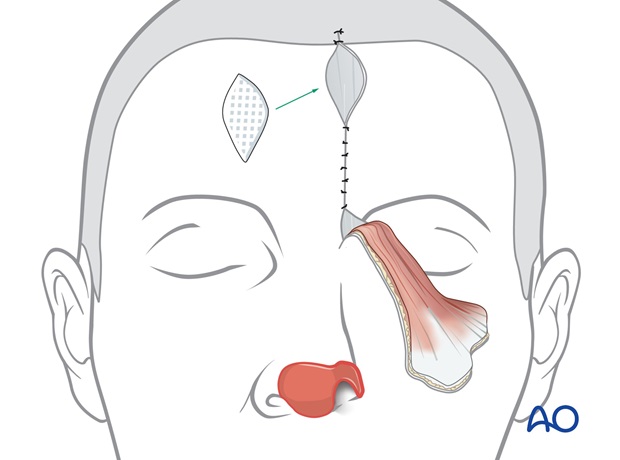
Closure of donor site defect
A scalp dog ear is excised and the forehead is widely undermined.
The forehead defect is closed in layers.
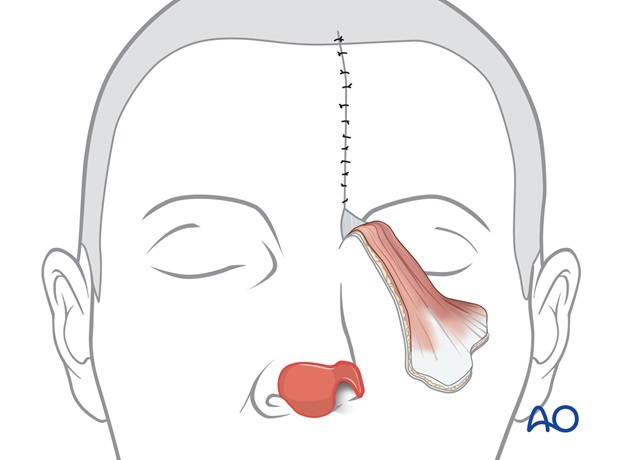
If the superior aspect of the defect cannot be closed primarily, it is allowed to heal secondarily over several weeks. The open area is covered with a petrolatum gauze for one week.
Flap inset
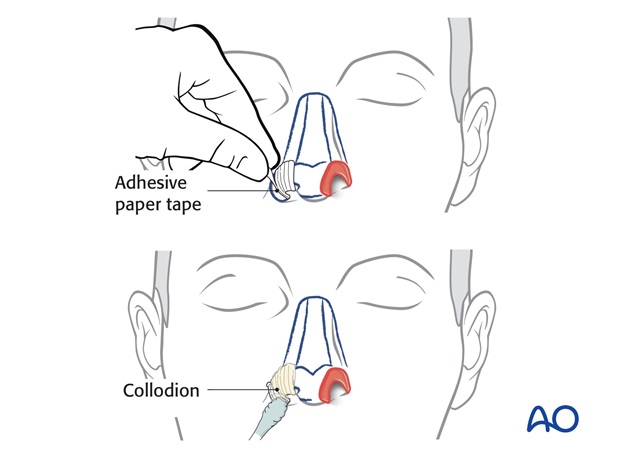
The distal end of the forehead flap is folded inwards into the nose. Normally the flap is not thinned of excess subcutaneous fat or frontalis muscle, but if the flap is especially stiff, the deep soft tissues can be thinned in the area of lining.
The blood supply of a full thickness forehead flap is abundant and the flap tolerates folding without ischemic problems.
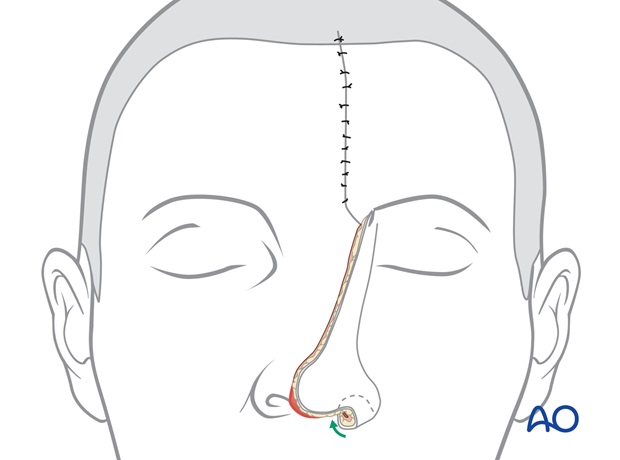
The lining extension is sutured into the lining defect and the external skin sutured along the periphery of the skin loss.
Primary cartilage support grafts are placed as necessary in all areas with underlining, normal residual nasal lining. But, normally no cartilage is placed in the area of forehead flap folding because it is difficult to position, fix, and design grafts in that area.
The closure of the forehead donor defect is similar to that of a routine forehead flap because the additional skin harvested for lining lies within the skin area normally incised in dog ear incision.
For more details please refer to the three stage forehead folded flap reconstruction for large full thickness defects.
Pre-and postoperative photographs of a small full thickness defect repaired with a three stage forehead folded flap.

9. Microvascular lining replacement with distant tissue
Distant tissue transferred as a free flap may be required for especially large and complex nasal defects with or without radiation injury, because local or regional tissues like a forehead flap are unavailable in dimension, volume, or blood supply to supply the needs of the defect. A microvascular flap can vascularize an ischemic wound, supply midfacial bulk, and provide an inner lining layer for the reconstructive nose.
The skin quality of distant tissue does not match the skin colour and texture so a forehead flap will be required to supply missing covering skin.
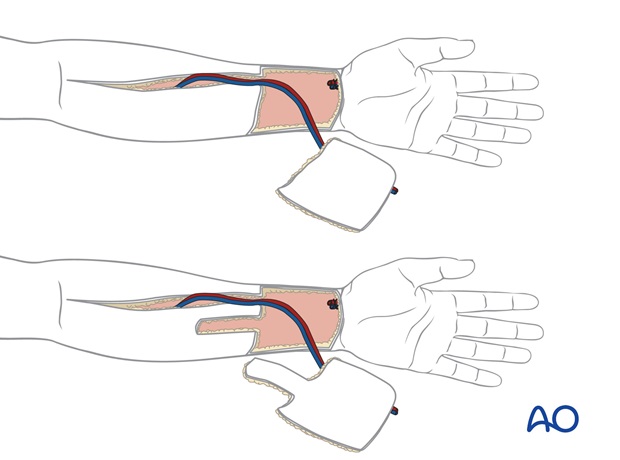
Most often, the radial forearm flap is used for lining because of its availability and relative thinness.
Nasal lining
In subtotal and total nasal reconstructions lining will often be required for the vault, nasal floor, and columella. Frequently, the septum is absent.

Approximately 8 cm of lining is needed from one alar base across the tip to the other alar base to reline the vault.
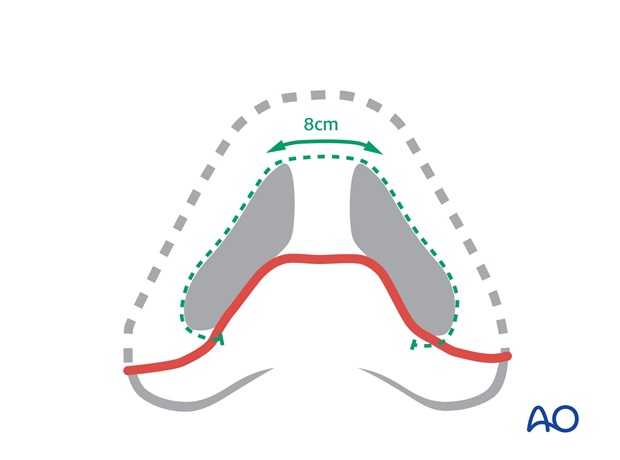
Loss of the nasal floor pulls the upper lip inward
by scar contraction. This must be replaced to reposition the lip. The nasal floor is part of the platform on which the nose sits.

The septum is not reconstructed but lining for the columella must be provided to create a soft tissue pocket in which a columella strut can be positioned.
A radial forearm flap can provide a large area of relatively thin skin based on a long vascular pedicle. An approximately 8 x 7 cm skin paddle is marked on the distal volar forearm over the radial vessels.
The forearm flap is designed as a single paddle or with a proximal extension if lining for the nasal floor is needed to release contraction of the lip.
It is harvested in a standard fashion, transferred to the face and anastomosed to the facial or cervical vessels.
Dorsal support
As the septum is largely absent, a rib graft is positioned as a cantilever graft to project from the remaining radix and nasal bone. This is fixed with one or more screws to the residual nasal bones.
Primary cartilage grafts for the columella, tip, or ala support are not placed at this time.

The dorsal graft may also be supported by a fixation plate.
The thin distal ulnar border of the flap is folded inwards to create lining for the vault and columella.
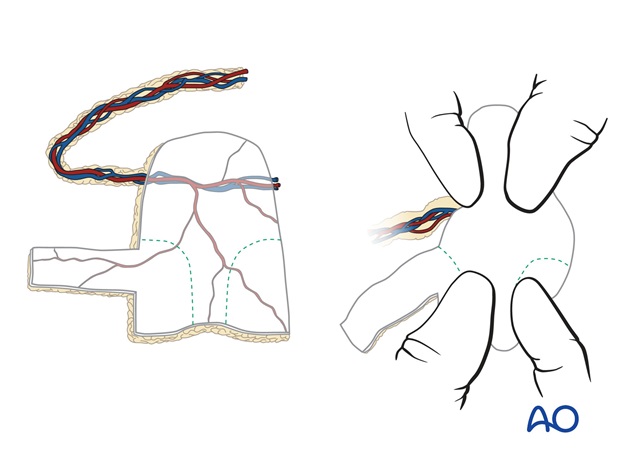
If necessary, the contracted scar within the injured nasal floor is released and the additional skin extension transferred to fill the deficiency.
The proximal external skin with the vascular pedicle is turned back over the lining to envelope the dorsal rib graft. The radial vessels are located at the proximal external skin component of the paddle.
For more details please refer to the four stage forehead flap with radial forearm for lining, used in the reconstruction of a large full thickness defect.

Pre-and postoperative photographs of a large full thickness defect repaired with a four stage forehead flap with radial forearm flap for lining.














