Static suspension with tendons
1. Introduction
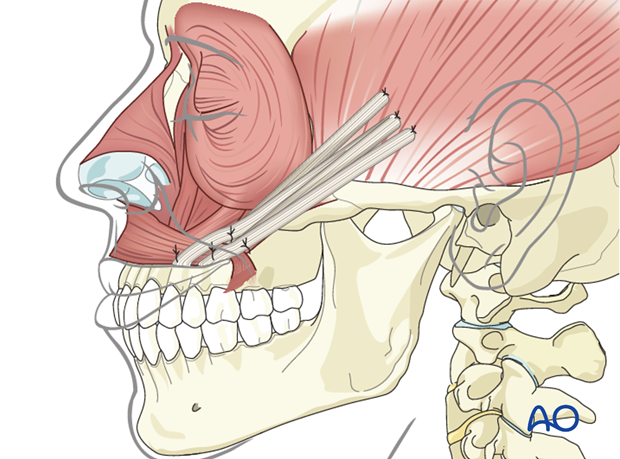
The goal is to achieve symmetry of the lower face only at repose.
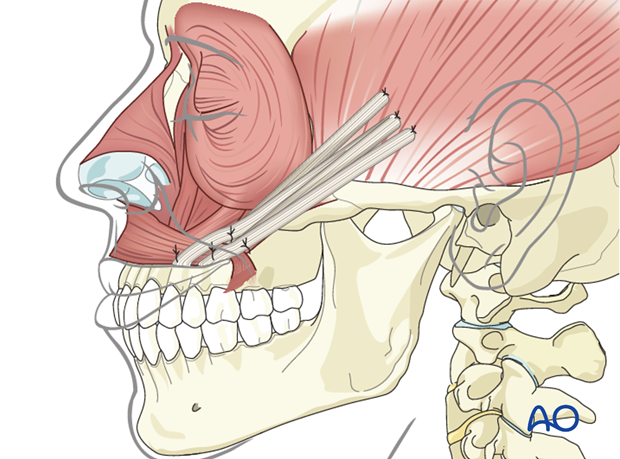
This involves static suspension of the oral commissure and lateral ala to recreate a nasolabial fold.
2. Approach
Primary reconstruction
Approach in primary reconstruction is performed through the existing surgical exposure (often a parotidectomy type incision).
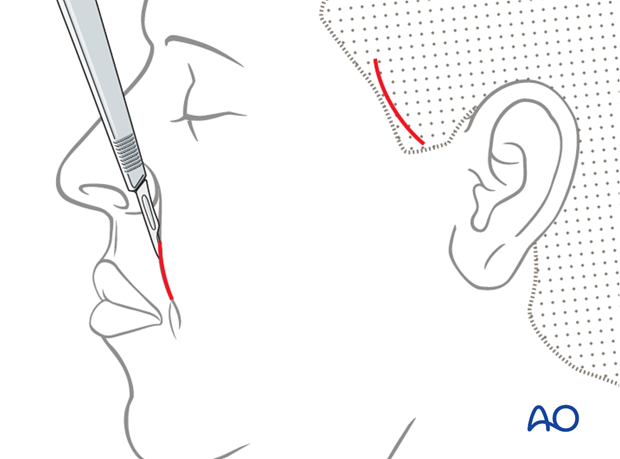
Secondary reconstruction
In secondary reconstruction hairline and nasolabial fold incision are required. It is beneficial to mark the nasolabial fold with the patient in sitting position prior to general anesthesia.
Secondary reconstruction will be illustrated as an example.
3. Technique
Tendon harvest
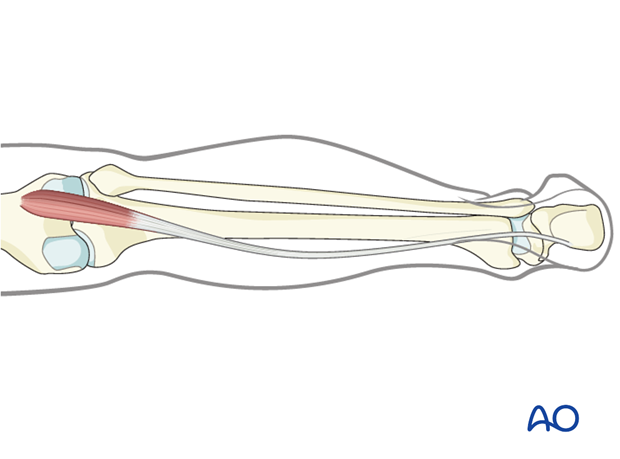
For midface resuspension, a longer tendon is often required. As a result, the plantaris longus is the preferred option.
Options to identify the tendons include:
- Preoperative MRI
- Intraoperative exploration
Other tendon options include palmaris longus or long extensors of the toes (3rd or 4th).
The full length of the selected tendon is harvested.
Advantages of using a tendon graft
- Resists lengthening
- Lower relapse rate
- Small scar
- Very long sling (especially with plantaris longus)
- Minimal to no donor deficit
Disadvantages of using a tendon graft
- Separate donor site scar
- Tendon absent in some patients (plantaris longus, palmaris longus)
Other suspension options include acellular dermal matrix, fasciae latae, Gore-Tex or other alloplastic materials.
Tendon sling positioning
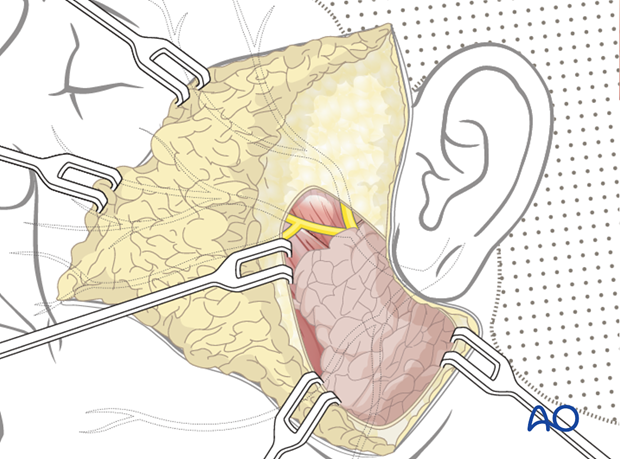
In secondary reconstruction, the tendon is tunneled from the temporal incision to the fixation points around the mouth.
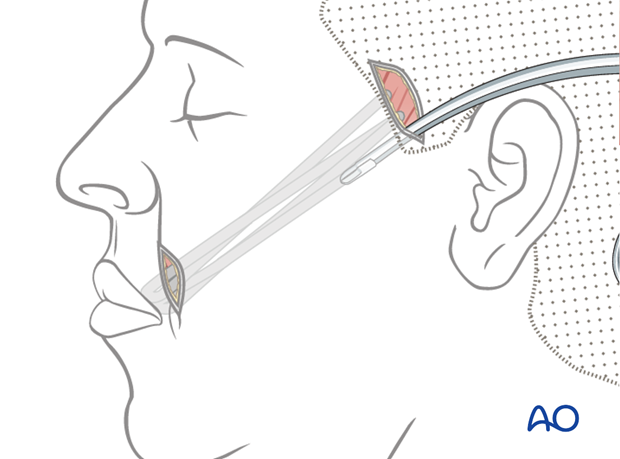
This allows positioning of the tendon to follow a similar vector of pull as the zygomaticus major muscle.
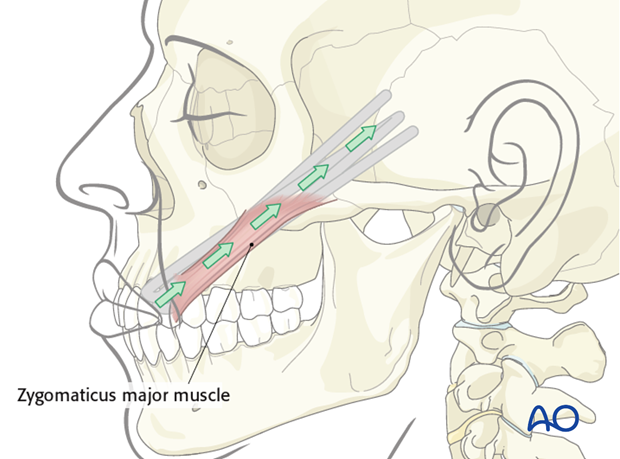
Separate tunnels are created. The tendon is woven back and forth through them to achieve multiple points of fixation, recreating the nasolabial fold and suspending the commissure.
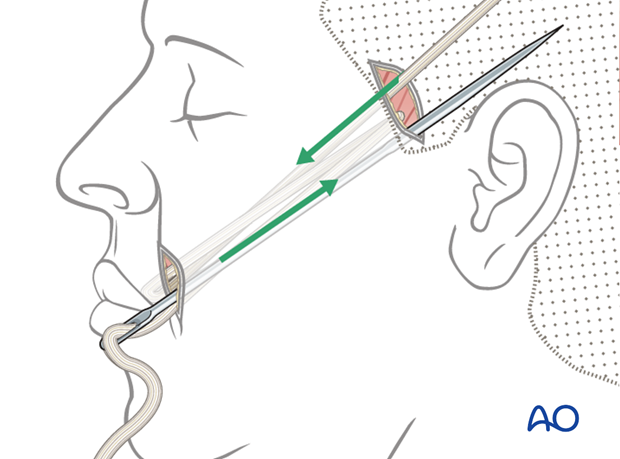
Tendon sling anchoring
The tendon is tightened to obtain overcorrection, because clinically there is a degree of relapse postoperatively.
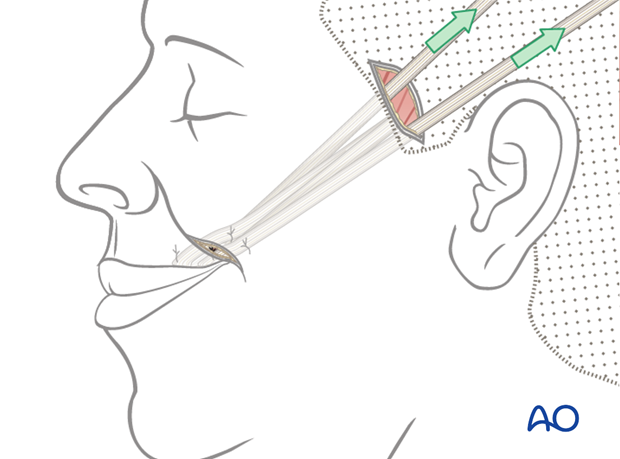
The tendon ends are anchored at the fixation points.
At the temporal incision, permanent suture is used to anchor the tendon to the deep temporal fascia.
At the mouth fixation points, the tendon is secured to the orbicularis oris muscle using permanent sutures.
Closure
Skin incisions are closed in layers.
4. Case example: irreversible facial paralysis following temporal bone resection
7 years postoperative following temporal bone resection and irreversible facial paralysis.
Reconstruction with static sling using palmaris tendon.
Symmetry at rest maintained long term, but severe asymmetry with movement.

Video of this patient at 7 years follow-up
5. Aftercare
The need for aftercare is to reduce the chance of inadvertent release of the suspension procedure. This can include maintaining soft diet 2-3 weeks postoperatively and minimizing exertion and trauma to the area during this period.
Generally, 4-6 weeks postoperatively patients are encouraged to return to normal activities without restrictions.
Infrequently, some patients may need formal mouth opening exercise if they develop trismus.
Specific physiotherapy exercises are started after this time. The goals are to improve symmetry both at rest and during function, through biofeedback and patient practice (in front of a mirror).













