Selective reinnervation with proximal facial nerve and masseteric nerve
1. Introduction
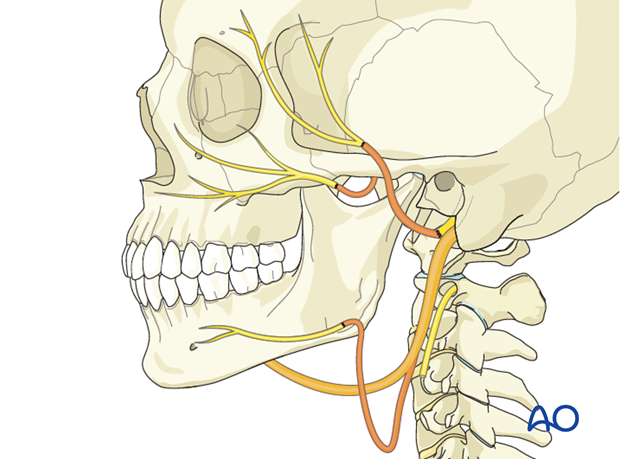
The principle of selective reinnervation is to use the ipsilateral proximal facial nerve to power eye closure and the ipsilateral masseteric nerve to power the smile.
Smiling and biting are synchronous actions. Patients can learn to perform both activities naturally at the same time. This is a distinct advantage over other nerve input options, such as hypoglossal or spinal accessory.
With ongoing practice and physiotherapy, some patients can learn to smile spontaneously. This may occur due to cortical adaptation.
General considerations regarding nerve repair techniques can be found here.
2. Proximal facial nerve to power eye closure
This technique is most commonly performed immediately following tumor ablation of the parotid gland, but it can be used whenever the proximal trunk of the facial nerve is available in order to limit synkinesis.
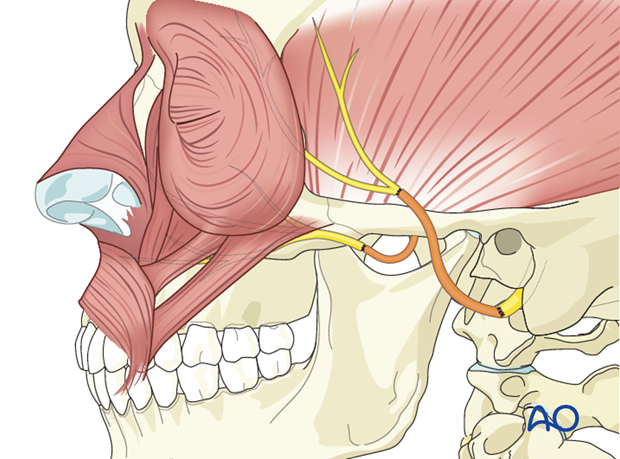
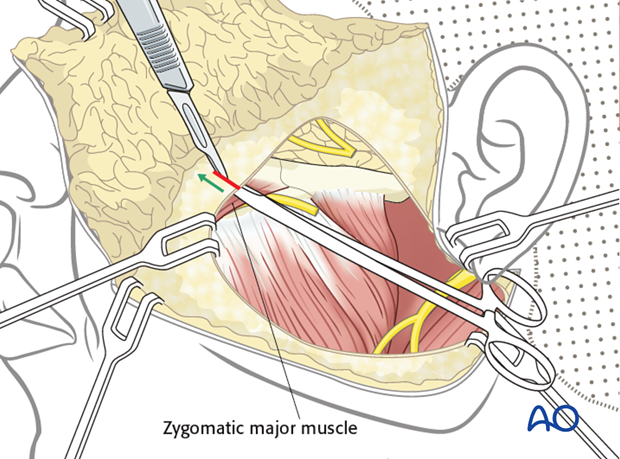
Approach and branches identification
A facelift or parotidectomy type incision is performed on the ipsilateral side.
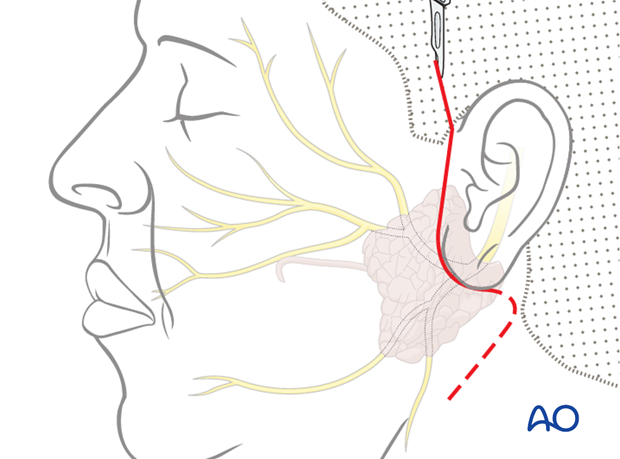
Proximal nerve identification
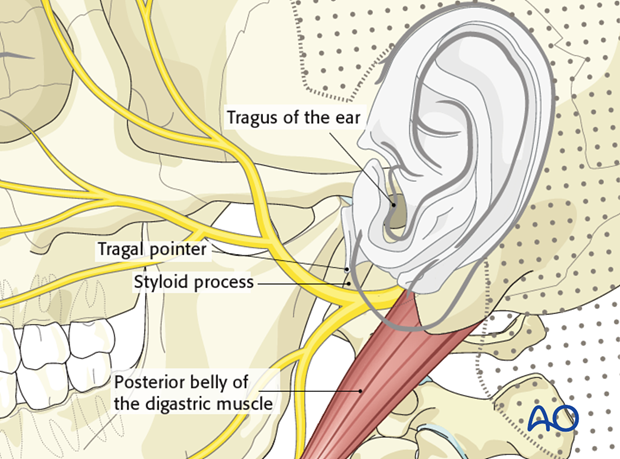
There are two common ways to identify the main trunk of the facial nerve:
- Identify the tragus of the ear. Dissect down the cartilage of the tragus to its inferior end called the “tragal pointer”. The nerve is found 1 cm inferior, anterior, and medial to the pointer.
- Identify the posterior belly of the digastric muscle. The nerve can be found immediately superior to the upper border of the muscle and at the same depth.
As a landmark for the facial nerve, the styloid process should be used with caution because it is situated immediately deep to the nerve.
A dissection is performed along the nerve through the parotid gland until the lacerated nerve branch is found.
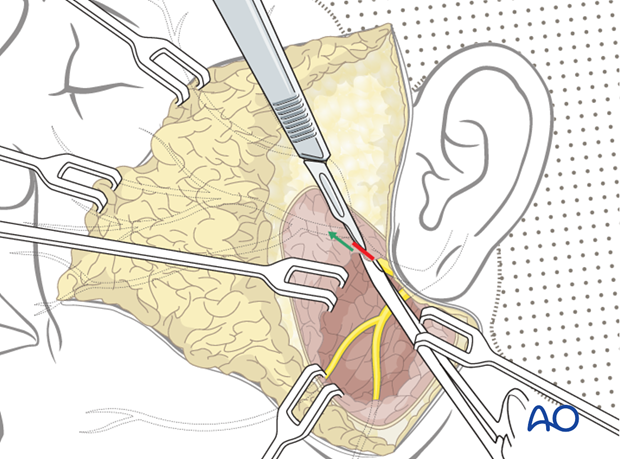
Preparation of distal ipsilateral nerves
On the ipsilateral (paralyzed) side the distal branches of the facial nerve are identified and exposed.
Intraoperative direct nerve stimulation may be possible up to 7 days from time of injury.
If not successful, the distal nerves are identified as they exit the parotid.
The distal nerves are dissected in retrograde fashion (from distal to proximal) through the parotid gland until the lacerated branches are identified.
Nerve graft coaptation
A nerve graft is needed from the proximal facial nerve to the distal upper branches.
Coaptation of the interpositional nerve graft is performed.
3. Masseteric nerve reinnervation
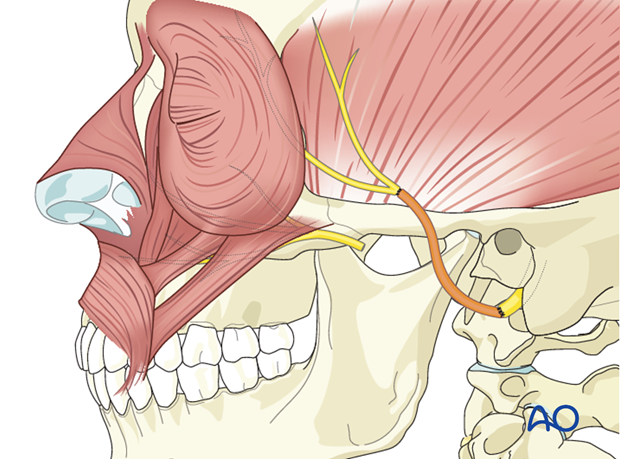
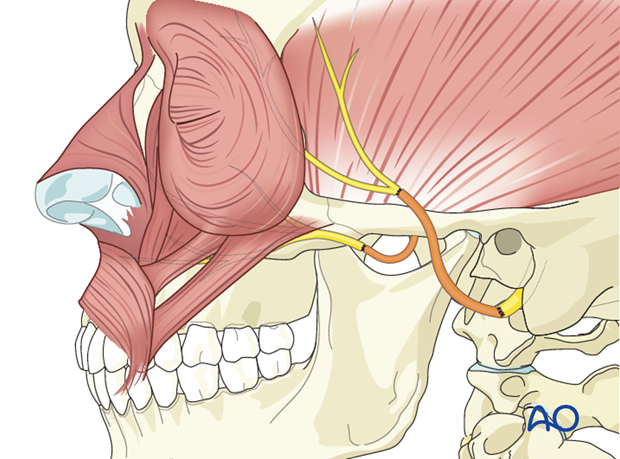
Masseteric nerve identification
The masseteric nerve is identified within the body of the masseter muscle at the level of the sigmoid notch.
A nerve stimulator is used to confirm activity prior to nerve division and preparation for coaptation.
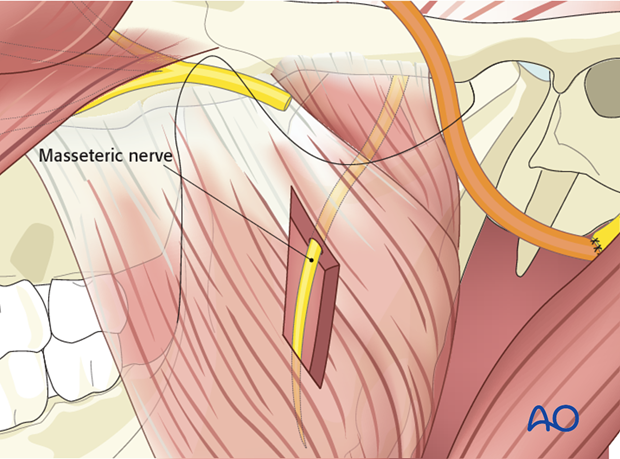
Masseteric nerve coaptation
A direct coaptation of the masseteric nerve to the nerve to zygomaticus major is performed to allow for commissure elevation.
4. Reinnervation of the lower division of the facial nerve
The lower division can be antagonistic to commissure elevation when trying to smile. Two options exist:
1. Avoid reinnervation of the lower division
Advantage: less invasive
Disadvantage: no tone to lower lip musculature leaving patients with asymmetry at rest
2. Reinnervate the lower division using the ansa hypoglossi
Advantage: lower lip tone and better symmetry at rest
Disadvantage: longer procedure
Note: the ansa to the marginal anastomosis is a direct nerve repair, not an interposition nerve graft.
Static suspension may be used to augment reinnervation procedures, in order to improve facial symmetry at rest, especially during the period of facial nerve recovery.
Closure
The skin incision is closed in layers.
5. Case example: Selective reinnervation excluding the lower division
- Primary reconstruction of eye closure was performed with an interpositional nerve graft between the proximal facial nerve and the orbicularis oculi branches.
- Selective reinnervation for independent smile was performed by direct coaptation of zygomaticus major nerve to masseteric nerve
Note that no reinnervation of lower facial nerve branches leads to ptosis of oral commissure and lower lip at rest.
6. Case example: Selective reinnervation using the ansa hypoglossi for the lower division
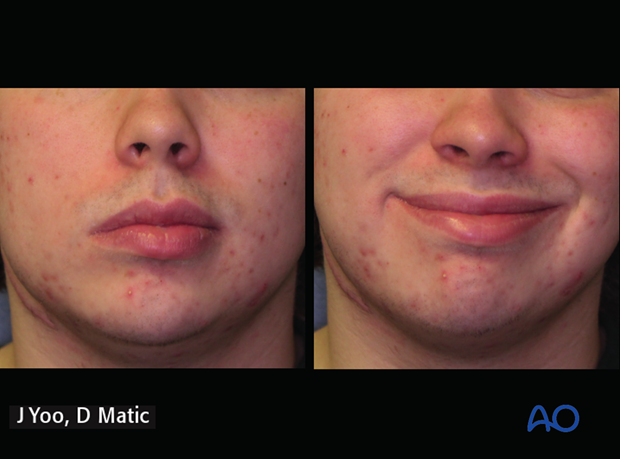
18-year-old male with complete facial paralysis secondary to a facial nerve schwannoma.

7 months postoperative following selective reinnervation.
- Masseteric nerve to upper division of facial nerve provides movement and facial tone
- Ansa hypoglossi direct coaptation to lower division of facial nerve provides lower lip muscle tone and midline position
The picture is showing the patient at rest and smiling.
7. Aftercare
Routine wound care is all that is necessary for the majority of the procedures.













