Lateral tarsorrhaphy
1. Introduction
Goal of lateral tarsorrhaphy
The goal of lateral tarsorrhaphy is to protect the cornea and reduce symptoms of exposure, such as excessive tearing and pain.
Types of tarsorrhaphy
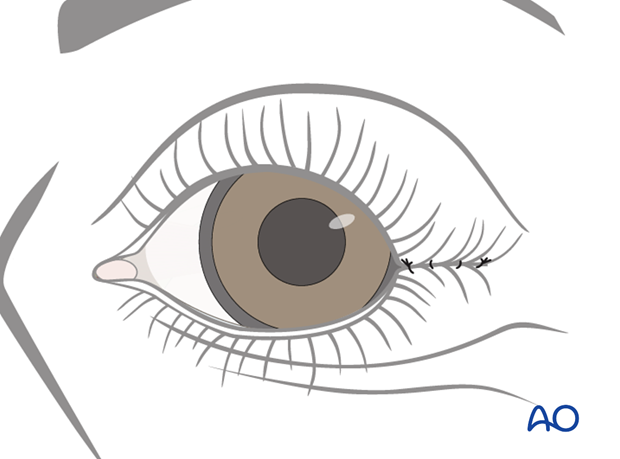
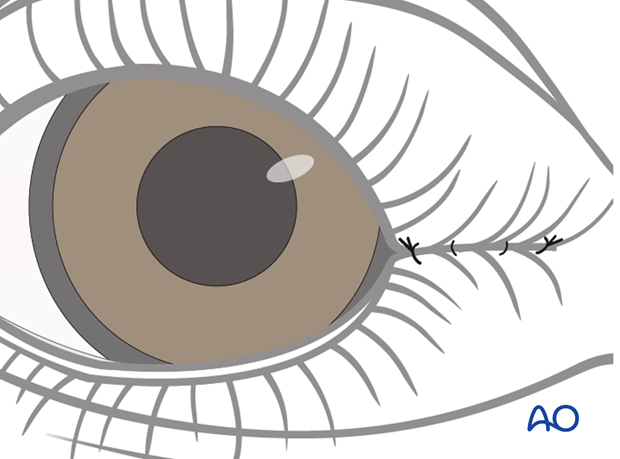
The procedure involves attaching the lateral portion of the lower and upper lids together to partially close the eye. It can be a temporary solution or a more definitive one.
The most commonly used tarsorrhaphy in paralyzed eyelids is permanent tarsorrhaphy, even if the patients are often unhappy due to both obstruction of lateral vision and cosmetic appearance.
For more information on temporary tarsorrhaphy please refer to the transcutaneous lower eyelid approaches in the midface section of the AO Surgery Reference.
This type of procedure can also be performed medially, to reduce medial ectropion.
2. Technique
This procedure can be performed either under local or general anesthetic.
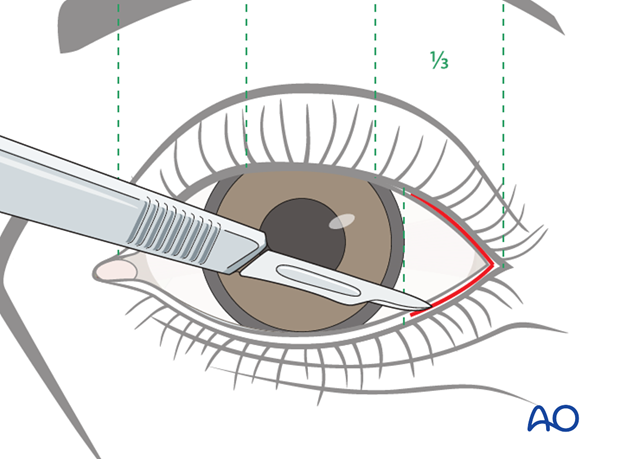
Incision
An incision is made in the lateral 1/4 to 1/3 of the upper and lower eyelid, stopping short of the lateral limbus of the iris.
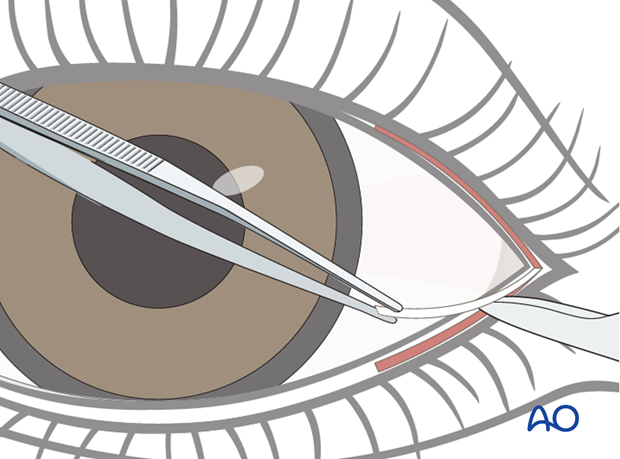
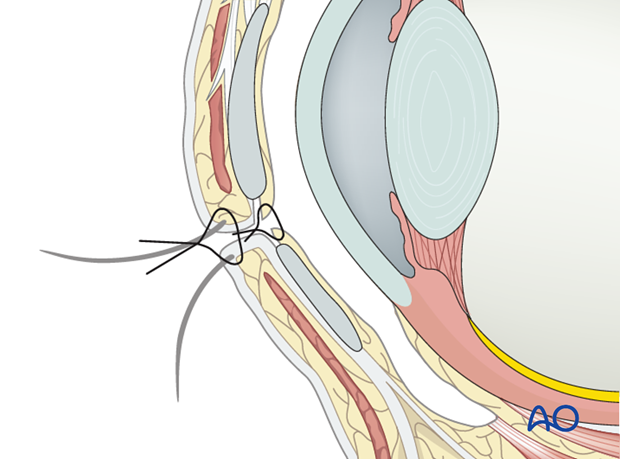
Lamellae splitting
The anterior and posterior lamella is split along the grey line to a depth of 3-5 mm.
A thin portion of epithelium of the lid margin can be excised at this stage in order to reduce the risk of dehiscence.
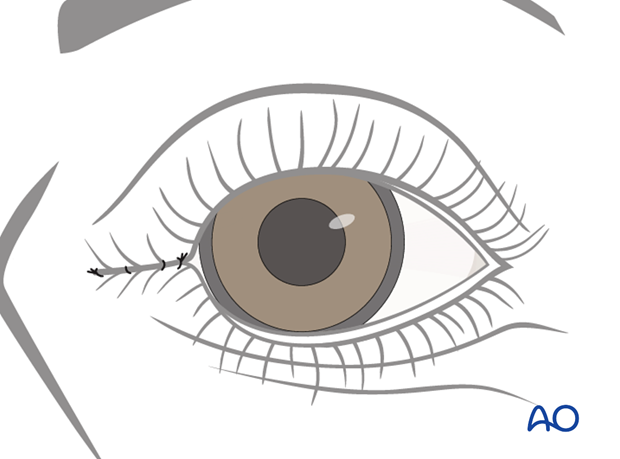
Suture
The posterior lamella, followed by the anterior lamella, of the upper and lower eyelids are sutured together using a resorbable suture.
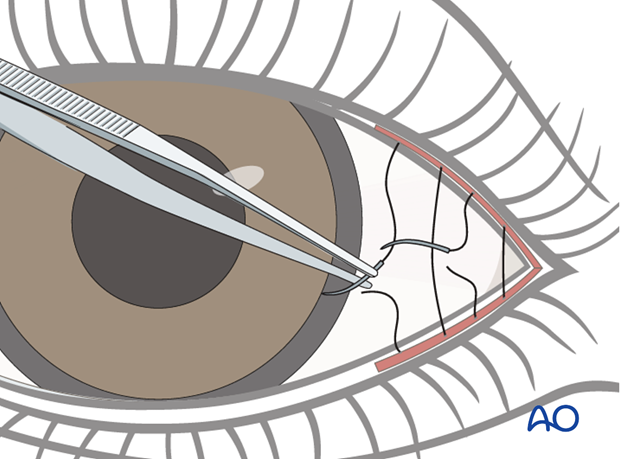
The posterior lamella sutures are inverted (buried) to prevent corneal irritation.
Care should be taken not to damage the eye lashes as this procedure is often reversed at the time of definitive eyelid surgery for eyelid closure.
3. Aftercare
Lubrication
It is important to maintain lubrication and protection of the eye.
Lubrication consists of natural tear substitutes during the day and ointment based lubricants during sleep, often together with taping the eyelid closed.
Protection
Physical protection through eyewear may be necessary depending on occupation and environmental conditions.













