Direct nerve repair
1. Introduction
The indication for nerve exploration is based on clinical patient evaluation.
Nerve injuries are typically addressed after associated injuries are repaired (e.g. fractures).
This procedure is performed under general anesthetic using only short acting or reversible paralytic agents.
This allows direct nerve electrostimulation during the operation.
2. Nerve exploration
The strategy for nerve identification depends on the site of the nerve injury.
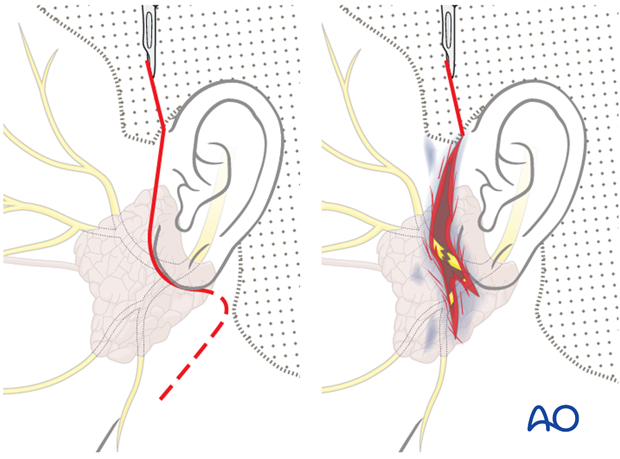
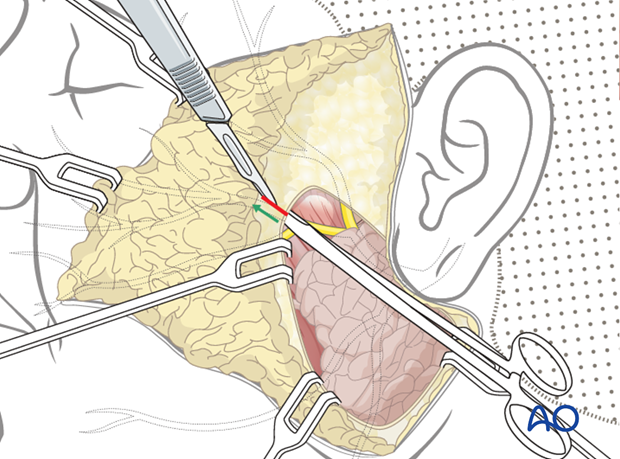
3. Nerve localization within the parotid gland
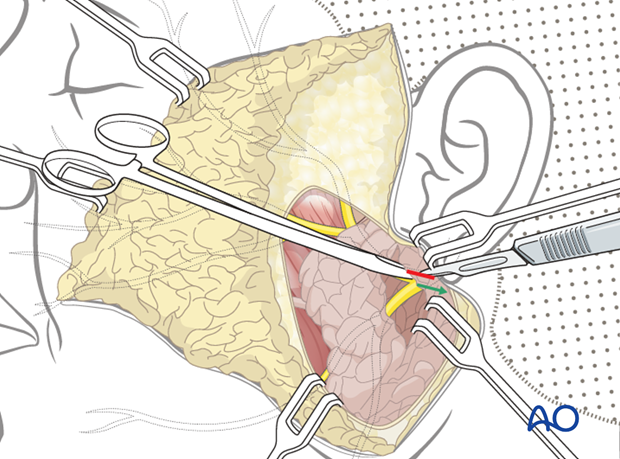
Nerve transections within the parotid gland are first explored in attempt to identify the cut distal and proximal ends.
The skin laceration may need to be extended.
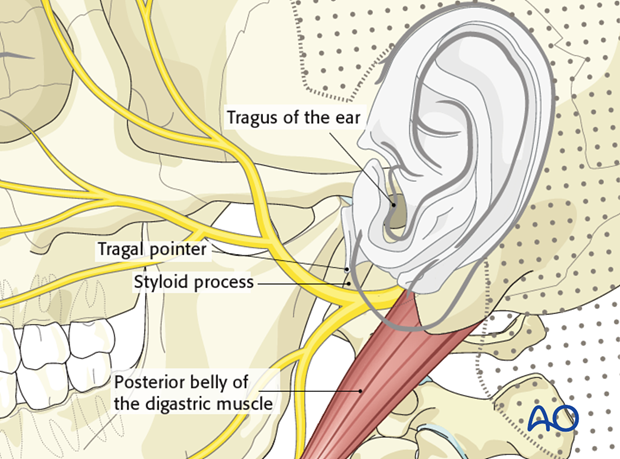
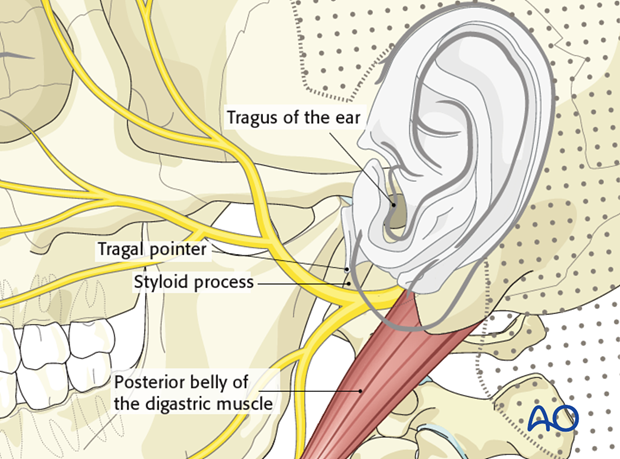
Identification of the main trunk of the facial nerve
There are two common ways to identify the main trunk of the facial nerve:
- Identify the tragus of the ear. Dissect down the cartilage of the tragus to its inferior end called the “tragal pointer”. The nerve is found 1 cm inferior, anterior, and medial to the pointer.
- Identify the posterior belly of the digastric muscle. The nerve can be found immediately superior to the upper border of the muscle and at the same depth.
As a landmark for the facial nerve, the styloid process should be used with caution because it is situated immediately deep to the nerve.
A dissection is performed along the nerve through the parotid gland until the lacerated proximal nerve branch is found.
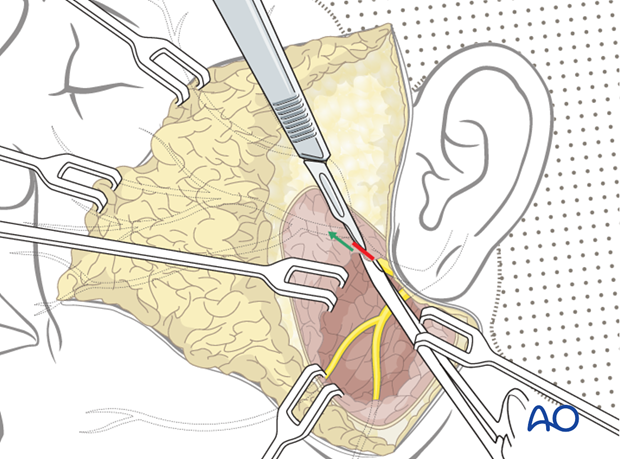
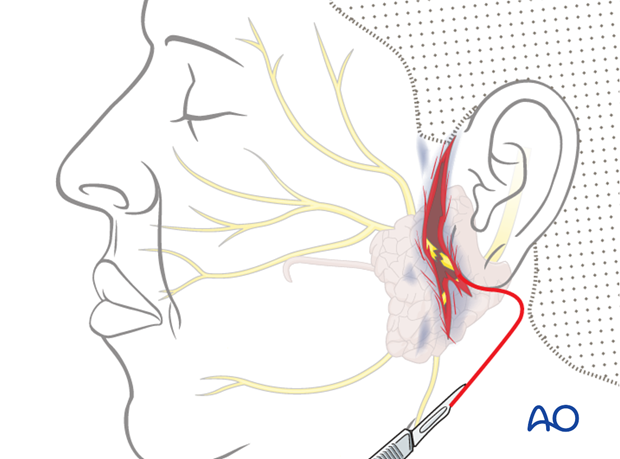
Distal nerve ending
Intraoperative direct nerve stimulation may be possible up to 7 days from the time of injury.
If not successful, the distal nerves are identified as they exit the parotid.
The distal nerves are dissected in retrograde fashion (from distal to proximal) through the parotid gland until the site of nerve injury is identified.
4. Nerve localization proximal to the parotid gland
Identification of the main trunk of the facial nerve
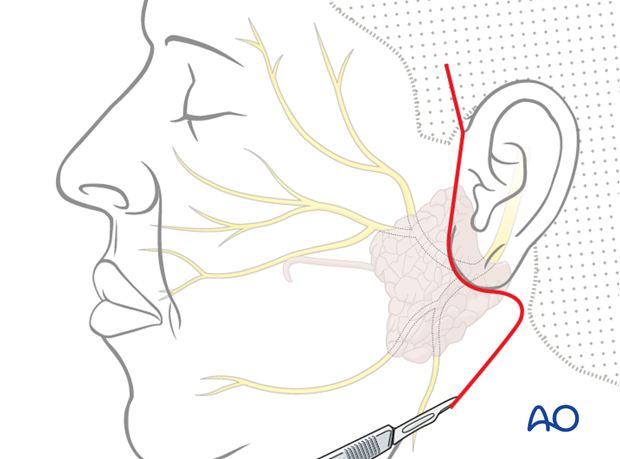
The main trunk of the facial nerve is identified through a limited facelift type of incision or parotidectomy (incorporating the laceration if possible).
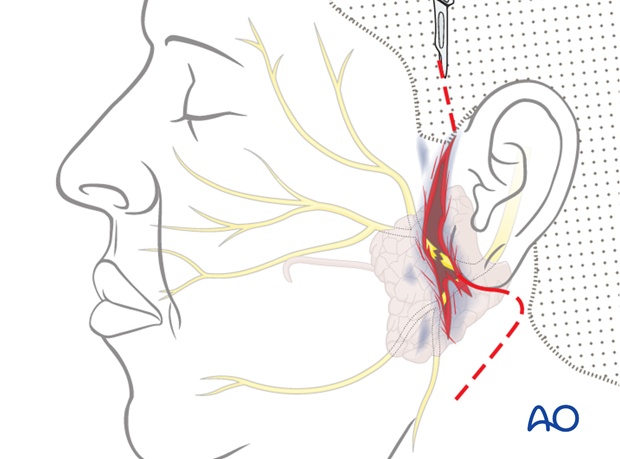
There are two common ways to identify the main trunk of the facial nerve:
- Identify the tragus of the ear. Dissect down the cartilage of the tragus to its inferior end called the “tragal pointer”. The nerve is found 1 cm inferior, anterior, and medial to the pointer.
- Identify the posterior belly of the digastric muscle. The nerve can be found immediately superior to the upper border of the muscle and at the same depth.
As a landmark for the facial nerve, the styloid process should be used with caution because it is situated immediately deep to the nerve.
Proximal/distal nerve ending
Dissect posteriorly until the lacerated nerve branch is found.
Parotidectomy type incision
If the nerve laceration cannot be found anterior to the stylomastoid foramen, a parotidectomy type incision is made to allow for further exploration.
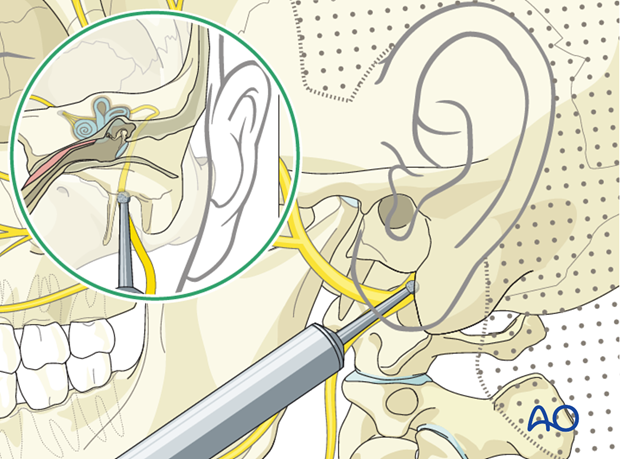
Drill out of the temporal bone
If necessary, a formal drill out of the temporal bone is performed to allow for identification and exploration of the intraosseous component of the facial nerve.
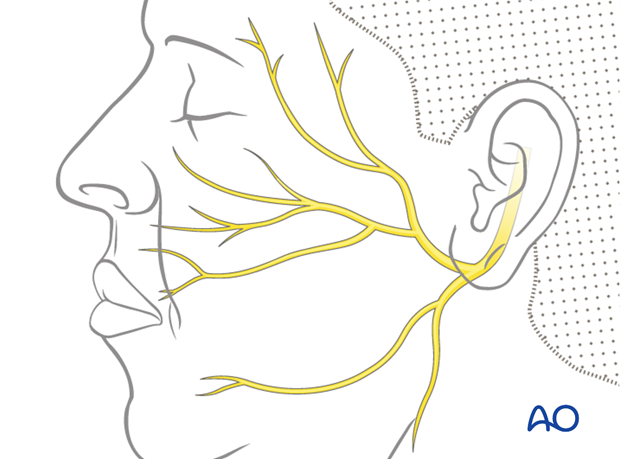
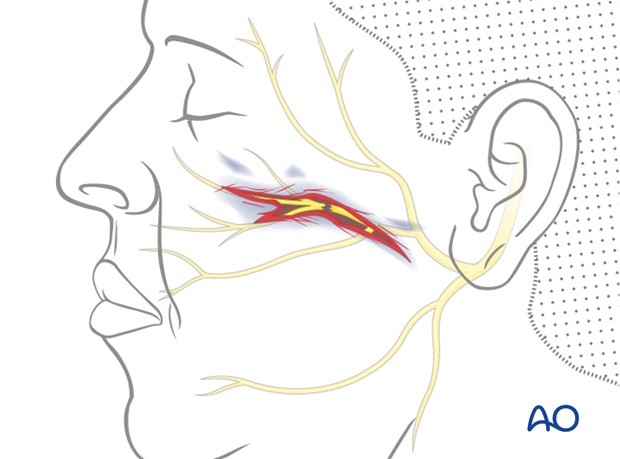
5. Nerve localization distal to the parotid gland
Both nerve ends are typically identified through the laceration, which can be extended if needed.
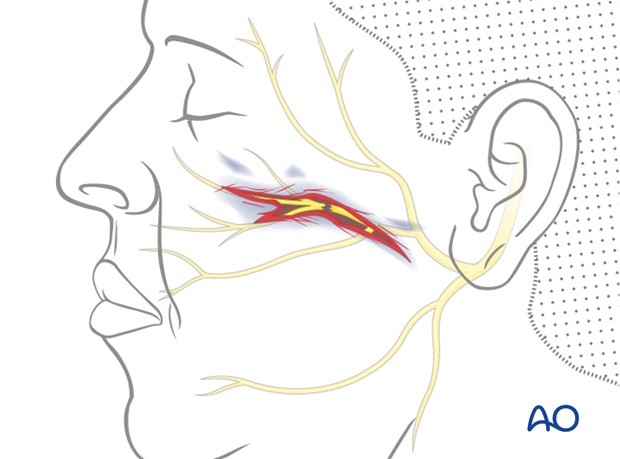
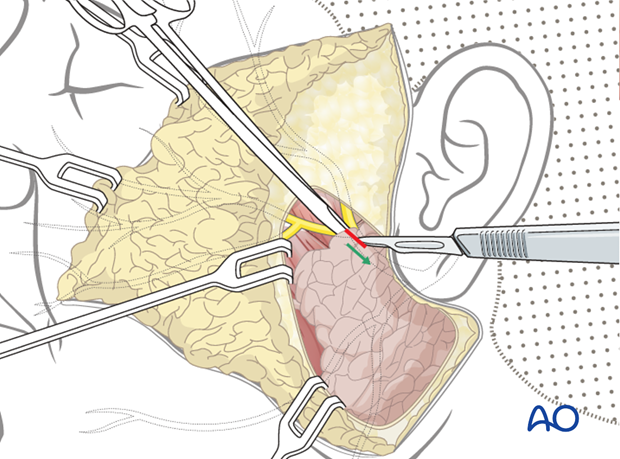
Proximal nerve ending
The proximal facial nerve branches are identified as they exit the anterior extent of the parotid gland.
The branches are dissected from proximal to distal until the lacerated ends are identified.
Distal nerve ending
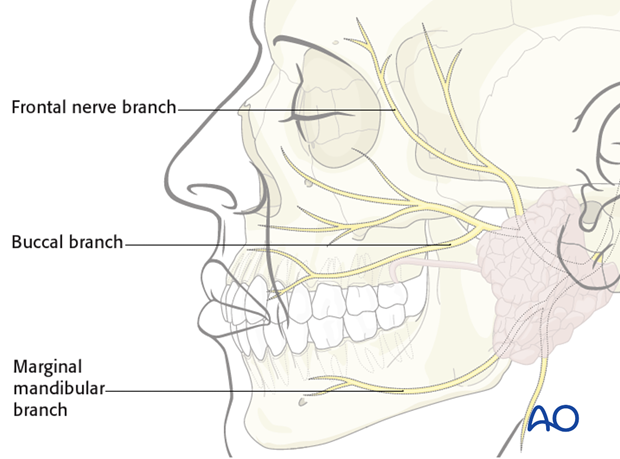
If the injury is within the first 7-10 days, the nerve can be identified by intraoperative stimulation.
- The frontal nerve branch courses superiorly, superficial to the zygomatic arch, up to 1 cm posterior to the lateral eyebrow.
- The buccal branch follows the Stenson's duct anteriorly.
- The marginal mandibular branch is most commonly located at the mandibular border, superficial to the facial vein.
The remaining of branches vary in anatomic location and there are no consistent landmarks to aid in identification.
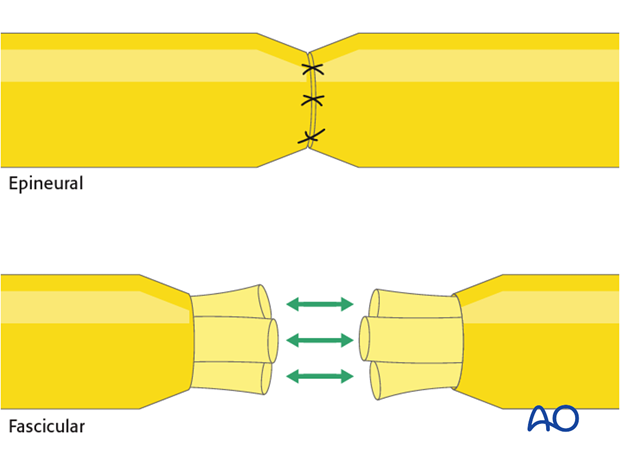
6. Direct nerve repair
There are several options for nerve repair (coaptation).
Generally, an epineural repair is performed. Proximal injuries may allow for a fascicular repair as well.
General considerations regarding nerve repair techniques can be found here.
Static suspension may be used to augment reinnervation procedures, in order to improve facial symmetry at rest, especially during the period of facial nerve recovery.
Closure
The skin incision is closed in layers.
7. Aftercare
Routine wound care is all that is necessary for the majority of the procedures.