Temporalis muscle (antidromic) mini-sling
1. Introduction
Local muscle flaps may enable dynamic movements of the oral commissure.
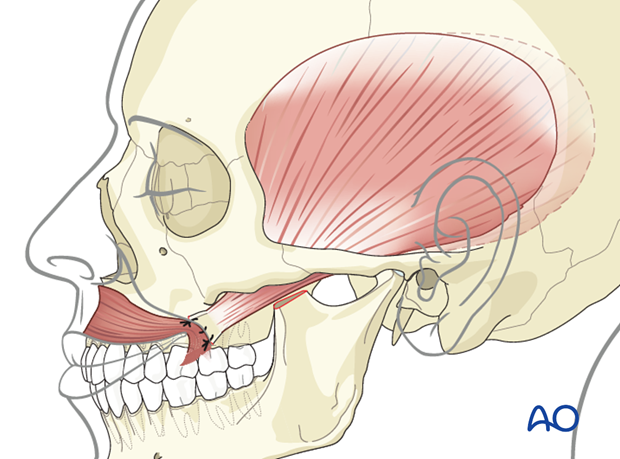
The two muscles that can be used for this are the masseter and the temporalis.
Clinical assessment prior to surgery is necessary to determine that the muscles of mastication are functioning.
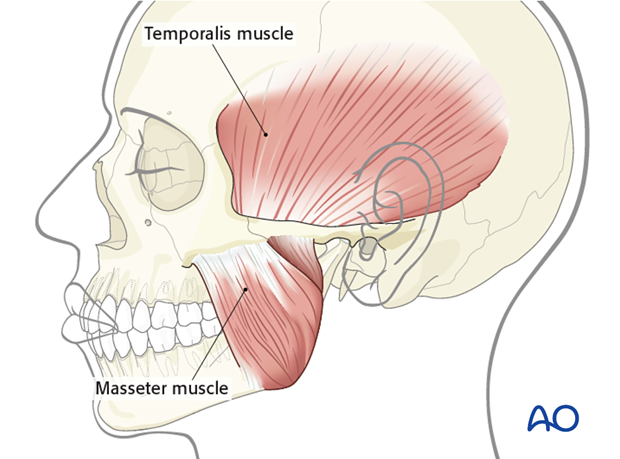
Traditional technique
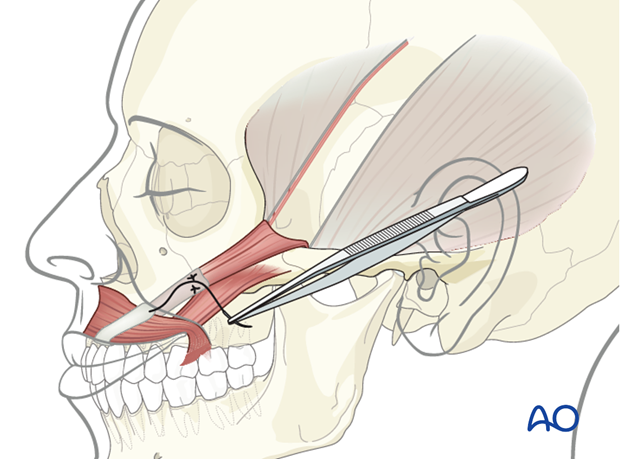
Traditionally, the temporalis muscle flap requires detaching its origin from the temporal fossa. This may involve either the entire muscle or a portion of it. The muscle is then turned over the zygomatic arch and anchored to the commissure. When the muscle origin is used as the dynamic component, it is termed "antidromic".
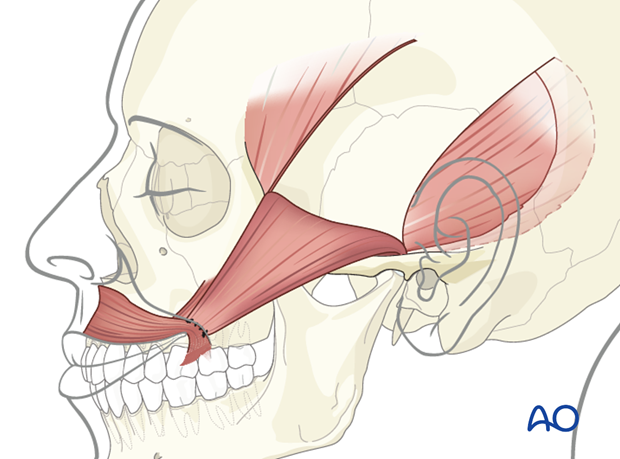
The limitation of this technique is the small excursion despite the correct vector. In addition, excessive bulk over the zygomatic arch and significant hollowing in the temporal fossa will occur.
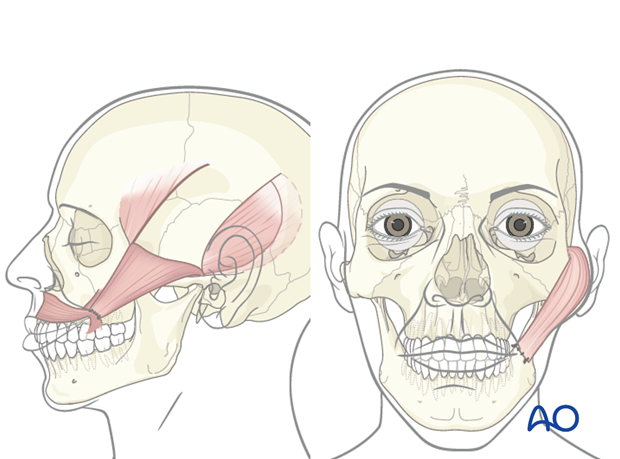
The temporalis mini muscle sling technique can be used as a dynamic reconstruction of the upper portion of the nasolabial fold. This technique achieves only minimal excursion (1-2 mm) and is best used in combination with other dynamic techniques.
Technique modifications
Several modifications have been described using the temporalis muscle transposition for facial paralysis. Recently, the orthodromic temporalis muscle transposition has gained popularity. The term "orthodromic" refers to the insertion point (coronoid process) of the temporalis muscle being used as the dynamic component.
Orthodromic temporalis muscle transposition involves releasing the muscle at its insertion on the coronoid and attaching it either directly or with the use of tendon graft to the oral commissure. The temporalis muscle origin can also be released either completely or partially, in order to increase muscle reach.
2. Approach
A parotidectomy type of incision can be extended superiorly into the hair bearing temporal area.
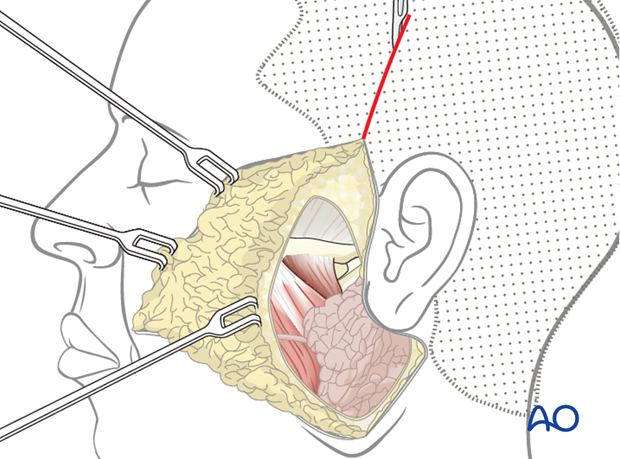
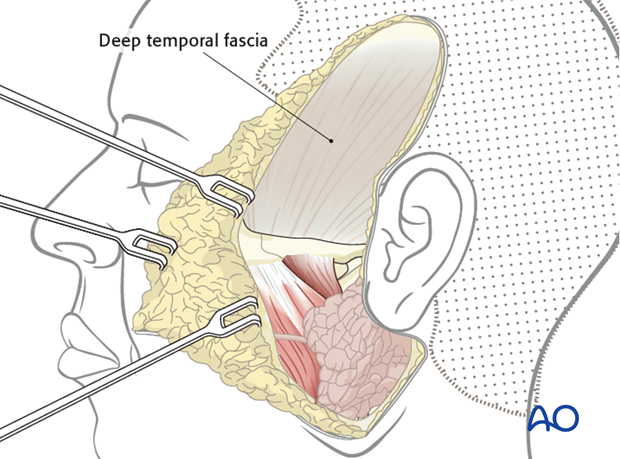
This allows dissection onto the deep temporal fascia which covers the temporalis muscle.
3. Technique
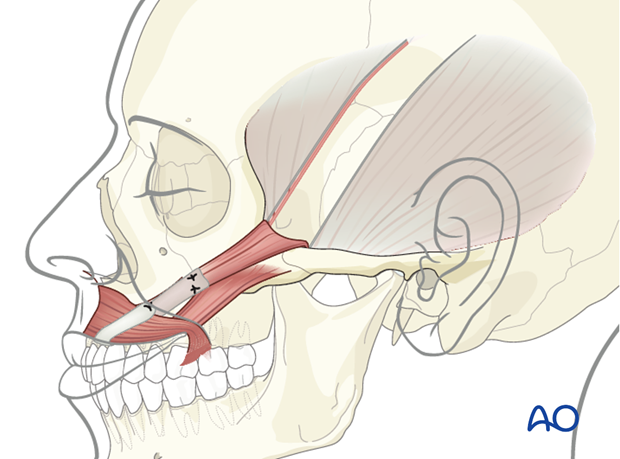
Flap preparation
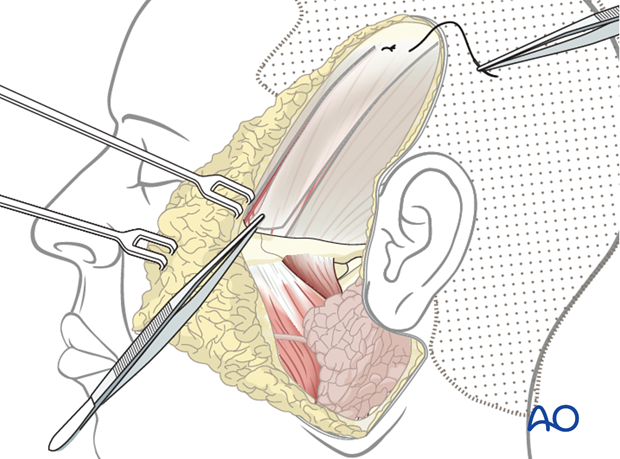
15 to 20 mm strip of muscle and fascia is incised in the mid portion of the temporalis muscle down to the temporal bone (vertical incisions).
Note: the inferior incision above the zygomatic arch goes only through the fascia.
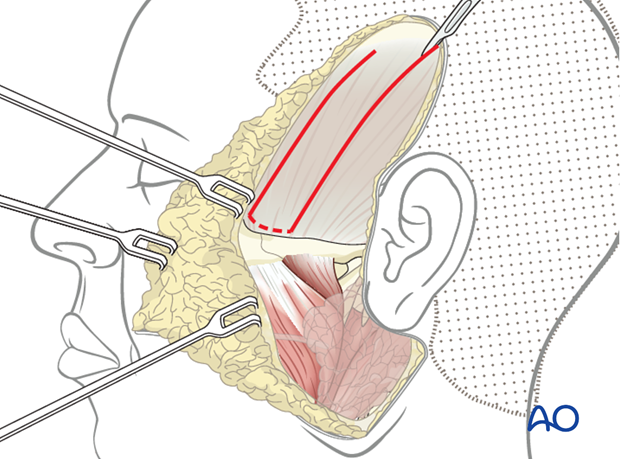
The deep temporal fascia is dissected from inferior to superior to act as an extension of the mini muscle slip.
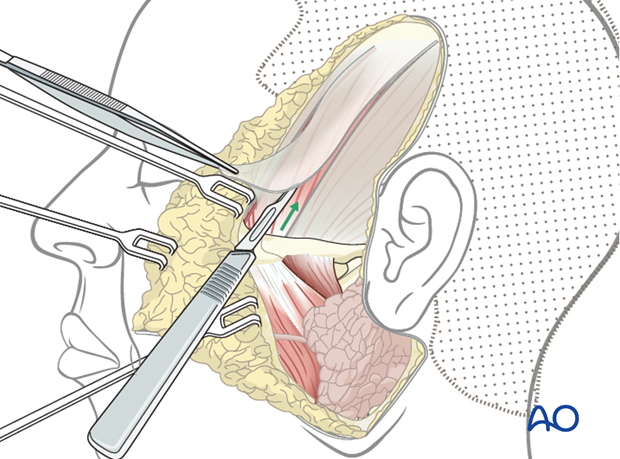
Horizontal mattress permanent sutures are used to anchor the distal end of the muscle slip to the deep temporal fascia.
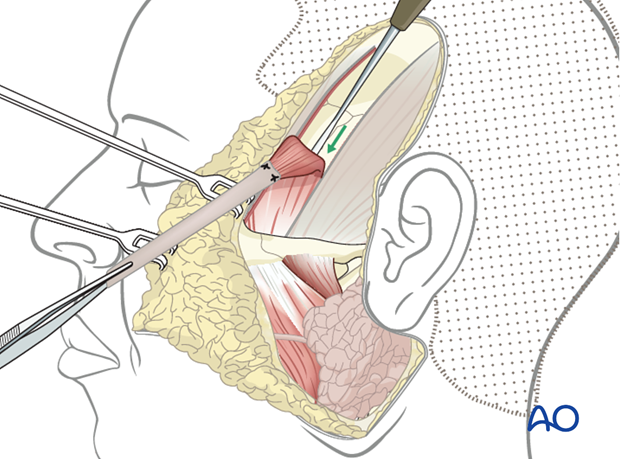
Periosteal elevator is used to elevate the muscle slip from superior to inferior off of the temporal bone.
Flap fixation
The slip of fascia is sutured and secured to the nasolabial fold using a non-resorbable 3-0 suture.
Closure
The skin incision is closed in layers.
4. Aftercare
The need for aftercare is to reduce the chance of inadvertent release of the suspension procedure. This can include maintaining soft diet 2-3 weeks postoperatively and minimizing exertion and trauma to the area during this period.
Generally, 4-6 weeks postoperatively patients are encouraged to return to normal activities without restrictions.
Infrequently, some patients may need formal mouth opening exercise if they develop trismus.
Specific physiotherapy exercises are started after this time. The goals are to improve symmetry both at rest and during function, through biofeedback and patient practice (in front of a mirror).













