Masseter muscle transposition
1. Introduction
Local muscle flaps may enable dynamic movements of the oral commissure.
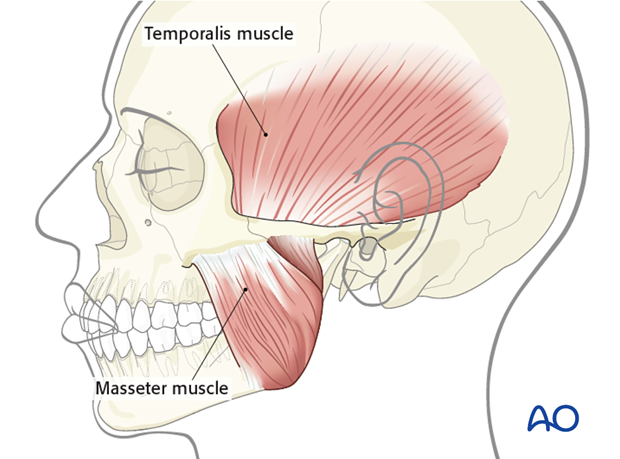
The two muscles that can be used for this purpose are the masseter and the temporalis.
Clinical assessment prior to surgery is necessary to determine that the muscles of mastication are functioning.
Traditional technique
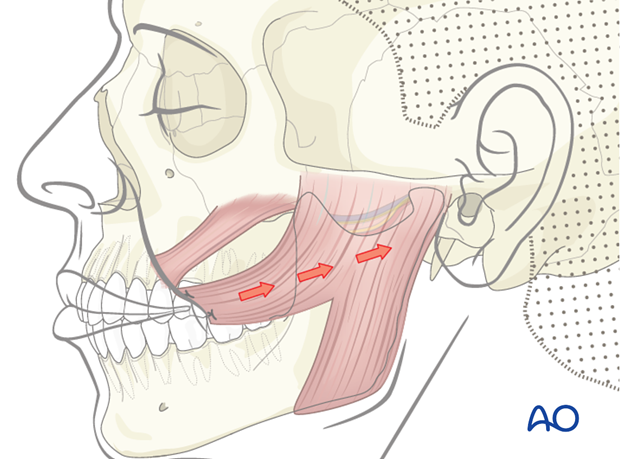
Traditionally, the masseter muscle transposition flap requires detaching the muscle insertion at the mandibular angle and reattaching it to the oral commissure.
The limitation of this technique is that the vector of pull is too horizontal and it does not simulate a natural smile.
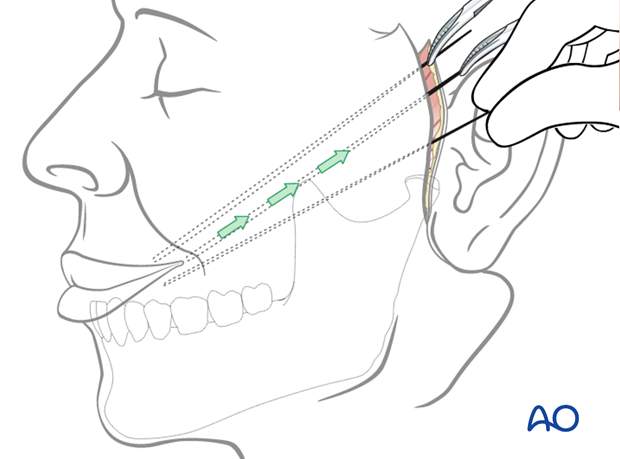
In order to improve the vector of pull and recreate a more natural smile, it is necessary to release the masseter muscle both from its origin (zygomatic arch) and insertion (mandibular angle).
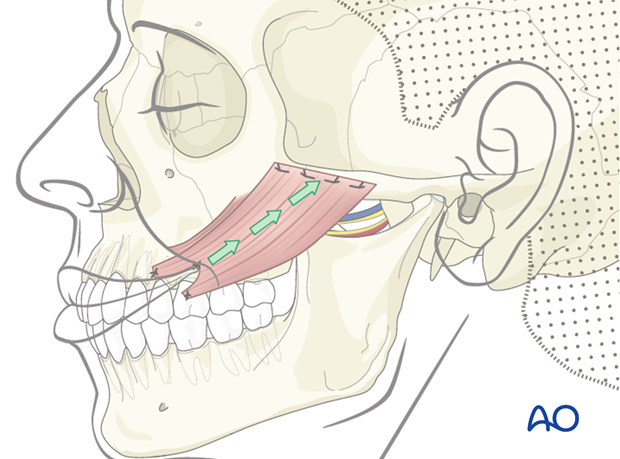
This allows mobilization of the entire muscle to better simulate the pull of the zygomaticus major.
2. Approach
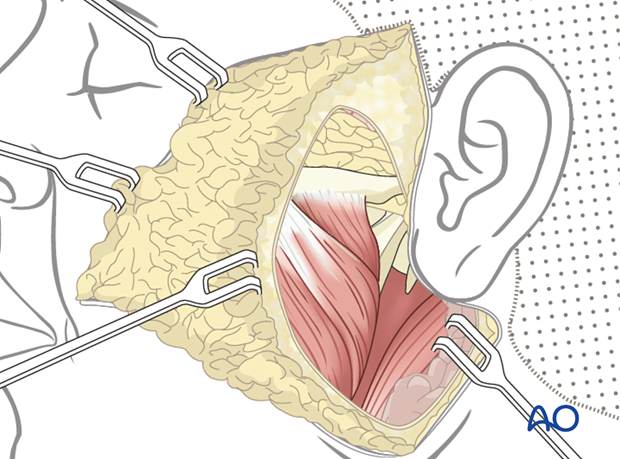
A parotidectomy type of incision is performed.
The parotid gland, if present, can be mobilized in order to expose the masseter muscle. The skin flap is elevated to allow exposure of both the commissure and the zygomatic body.
3. Technique
Flap preparation
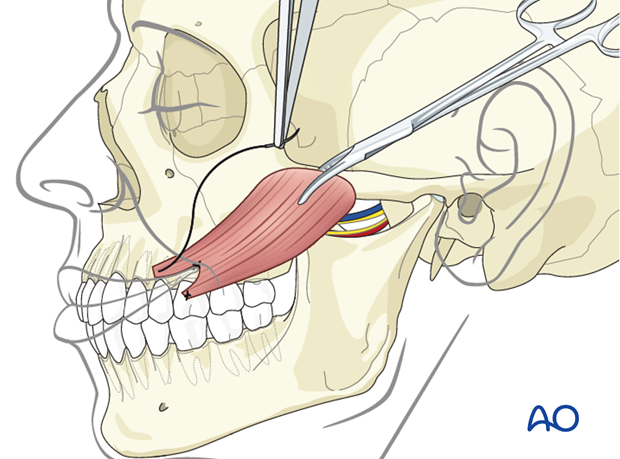
The margins of the masseter muscle are defined and the location of the sigmoid notch is palpated.
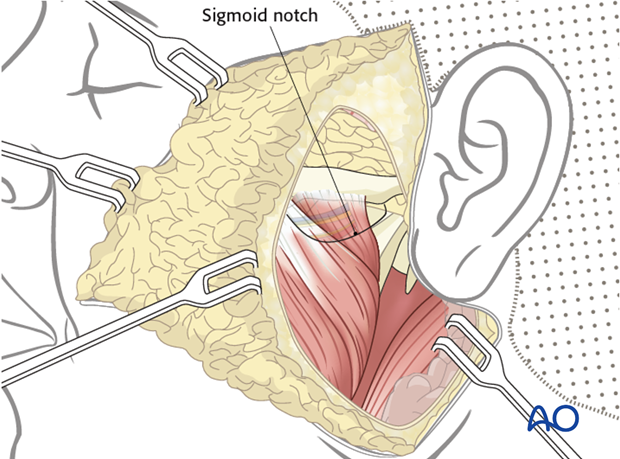
The muscle is detached from the angle and the ramus of the mandible, and mobilized from posterior to anterior to the sigmoid notch in the subperiosteal plane. This avoids injury to the neurovascular pedicle.
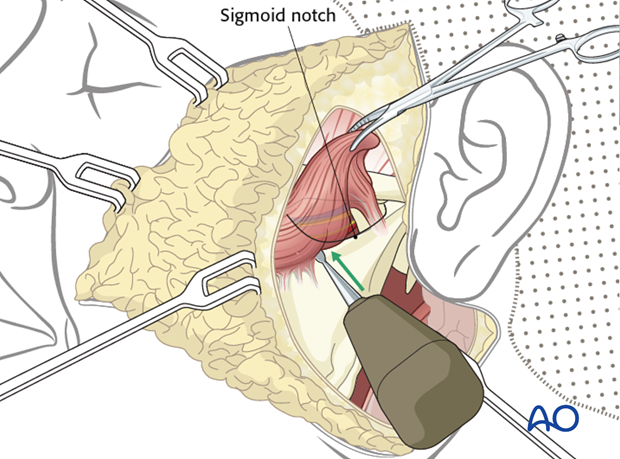
Attention should be paid to preserve the neurovascular pedicle, which enters the muscle through the sigmoid notch.

The origin of the masseter muscle is detached from superficial to deep off the zygomatic arch while protecting the neurovascular pedicle. This enables medialization and reorientation of the muscle to better match the vector of pull of the zygomaticus major.
Flap fixation
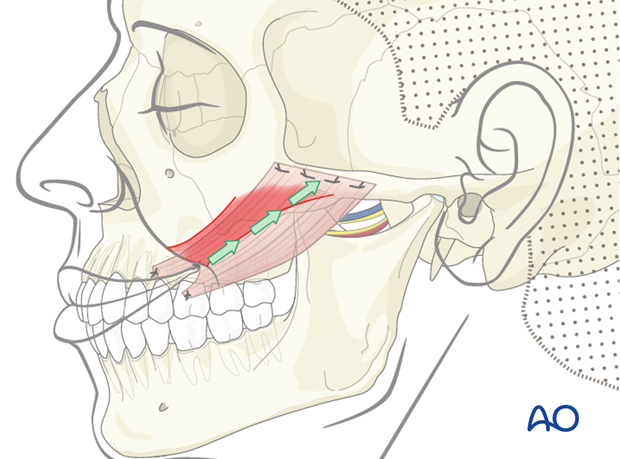
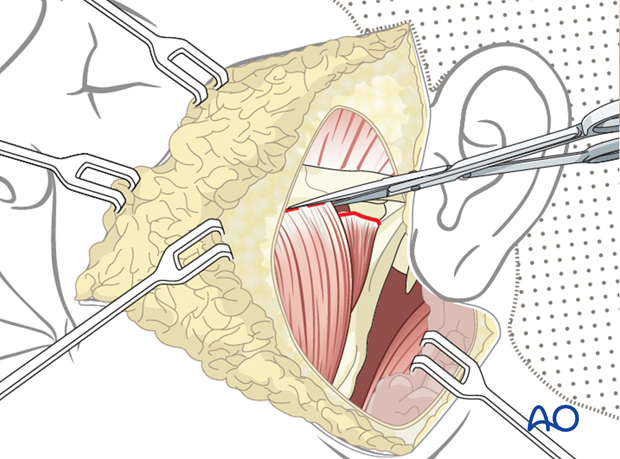
Three fixation points centered around the commissure are identified in the following order:
- Oral commissure
- Mid lower lateral lip
- Mid upper lateral lip
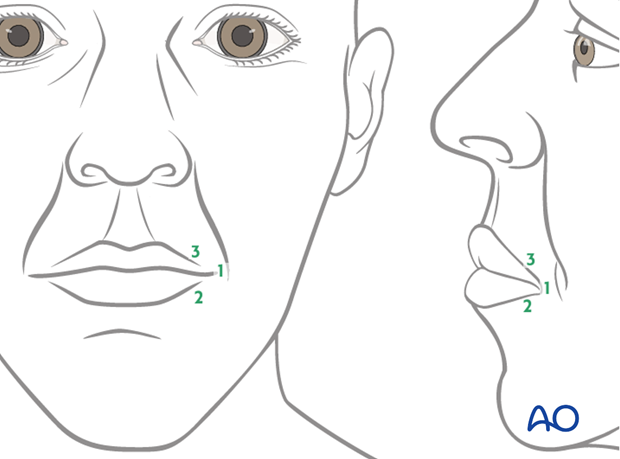
All points are identified through trial and error, using anchoring sutures and visual inspection. The goal is to achieve a natural smile vector and recreation of the nasolabial fold.
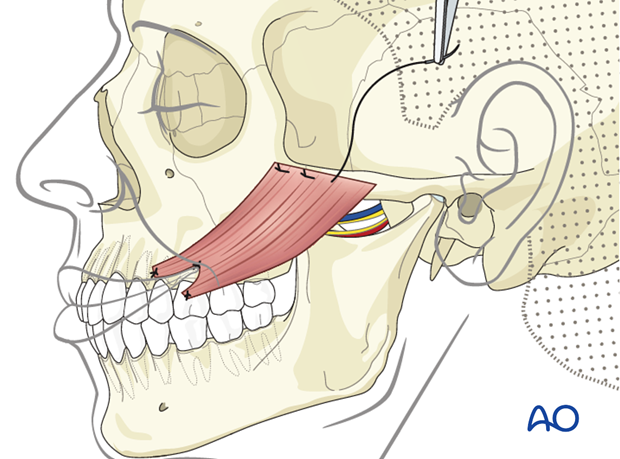
The muscle insertion is anchored to the three fixation points using permanent horizontal mattress sutures.
The muscle is placed under tension to achieve slight overcorrection of the smile and its origin is anchored onto the zygomatic body periosteum using permanent interrupted horizontal mattress sutures.
Closure
The skin incision is closed in layers.
4. Case example: complete facial paralysis after parotidectomy
a) 25-year-old male presenting with complete left facial paralysis, at 2 years postoperative after parotidectomy with resection of facial nerve.
b) Selective primary reconstruction was performed to minimize eye-smile synkinesis. The upper branches of the facial nerve have been reinnervated from proximal facial nerve with a sural nerve graft. Masseter muscle transfer was performed for dynamic smile reconstruction.

5. Aftercare
The need for aftercare is to reduce the chance of inadvertent release of the suspension procedure. This can include maintaining soft diet 2-3 weeks postoperatively and minimizing exertion and trauma to the area during this period.
Generally, 4-6 weeks postoperatively patients are encouraged to return to normal activities without restrictions.
Infrequently, some patients may need formal mouth opening exercise if they develop trismus.
Specific physiotherapy exercises are started after this time. The goals are to improve symmetry both at rest and during function, through biofeedback and patient practice (in front of a mirror).













