Lower eyelid - Lateral strip canthopexy
1. Introduction
Tearing in the paralyzed eyelid
There are several reasons for excessive tearing that occurs in patients with eyelid paralysis:
- Exposure. As the cornea dries, this leads to more tear production.
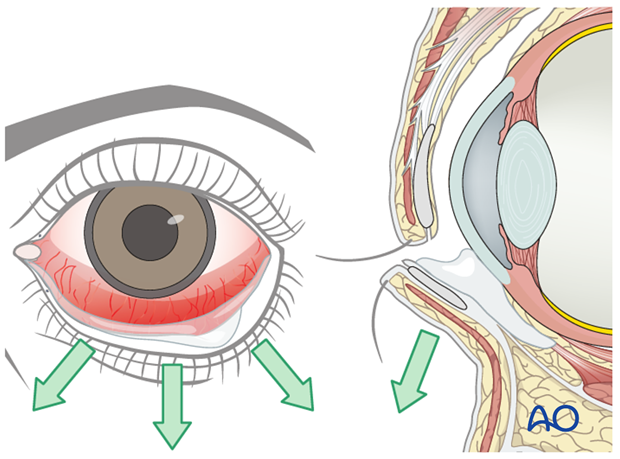
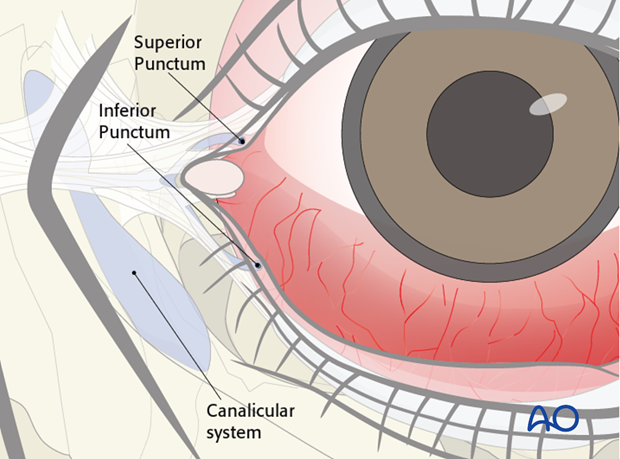
- Loss of lower eyelid support, secondary to flaccidity of the orbicularis oculi. As the lower lid falls away from the globe, the punctum and canalicular system works less efficiently to drain the tear film.
- The muscle driven pumping of the lacrimal sac cannot occur, which further increases tearing.
Closure of the upper eyelid reduces symptoms of exposure but does not improve the drainage system. Therefore, improving lower eyelid position also needs to be considered to further reduce tearing.
2. Planning and surgical preparation
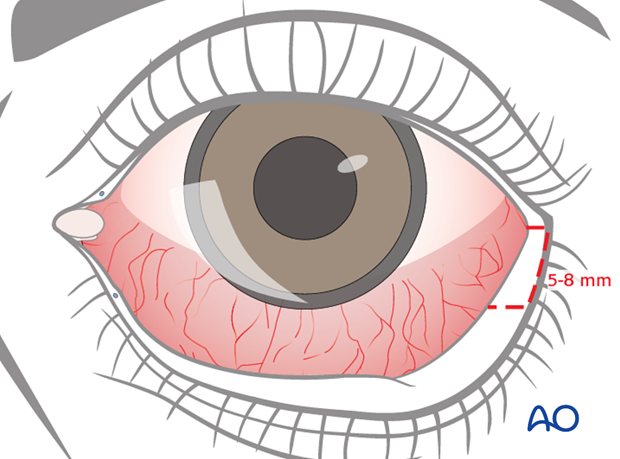
Clinically the patient is assessed to determine the degree of laxity of the lower eyelid and the amount of lower eyelid tissue to be removed.
In general, in patients with paralysis this is 5-8 mm.
3. Technique
This procedure can be performed either under local or general anesthetic.
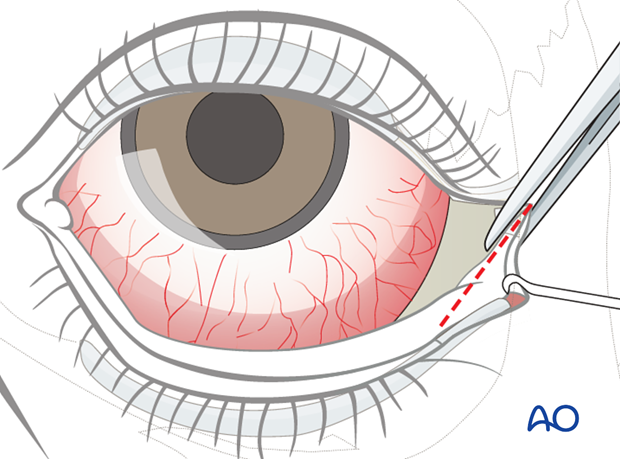
Lateral canthotomy and cantholysis
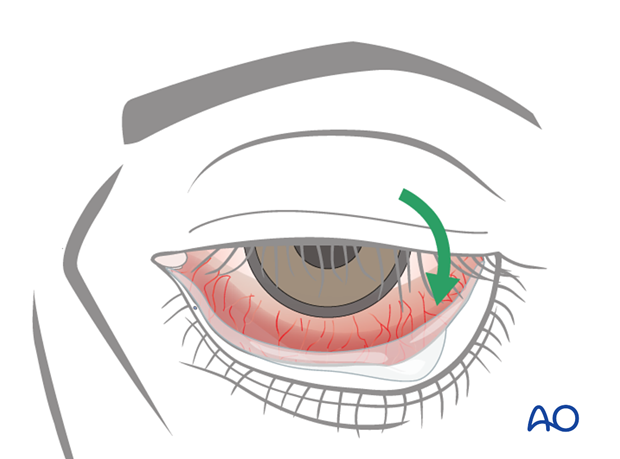
Fine scissors are inserted horizontally into the outer lid angle laterally, so that the instrument contacts the underlying bone of the lateral orbital rim (approximately 7-10 mm).
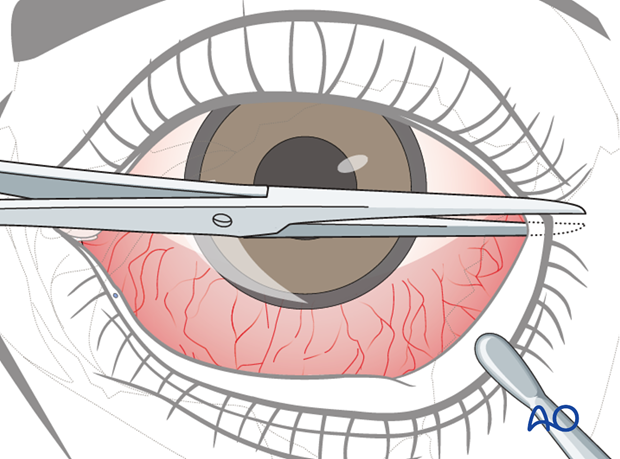
The lateral palpebral fissure is cut horizontally including the skin, the orbicularis oculi muscle, and the conjunctiva. The superficial fanning fibers of the lateral canthal tendon are also transected.
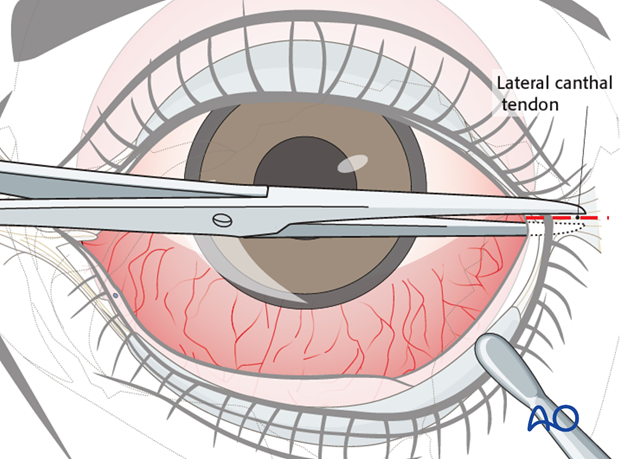
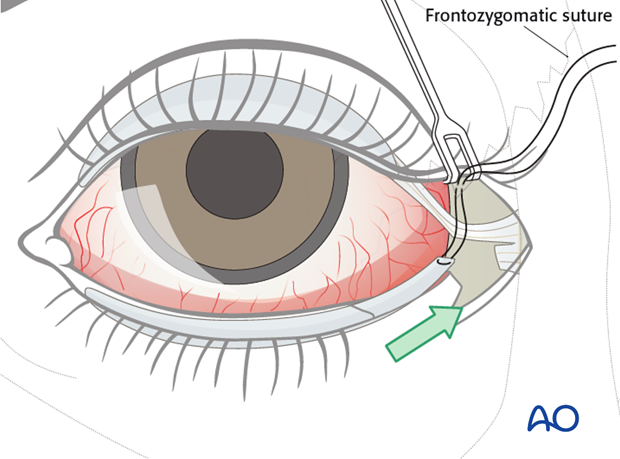
The lower eyelid is now everted. It is still fixed to the lateral orbital rim by the inferior limb of the lateral canthal tendon. The scissors are introduced vertically to transect this part of the lateral canthal apparatus (inferior cantholysis). The lower eyelid is freed and can be retracted more effectively to start swinging the lower lid outwards.
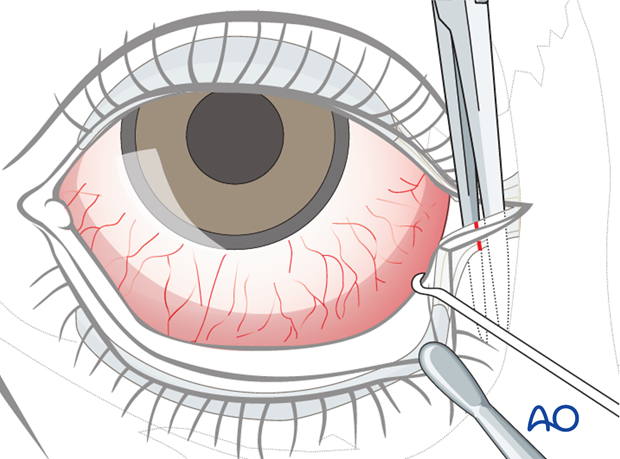
Lateral strip of tarsus
The anterior lamella including the gray line and eye lashes is removed. Approximately 5-8 mm of the anterior lamella is removed to expose the tarsus.
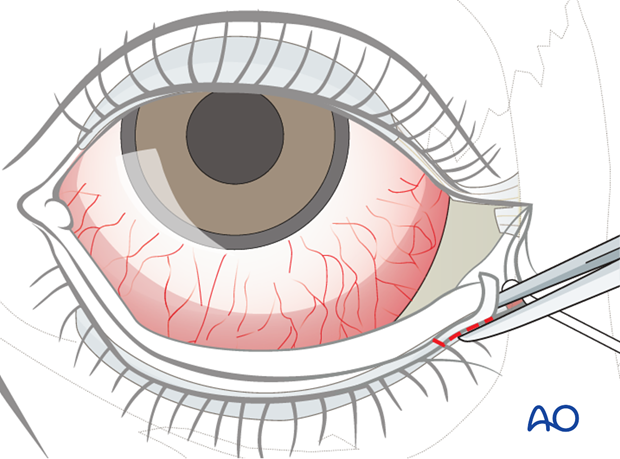
A cut is made inferior to the tarsus creating a strip.
The posterior conjunctiva overlying the tarsus can either be removed or left behind.
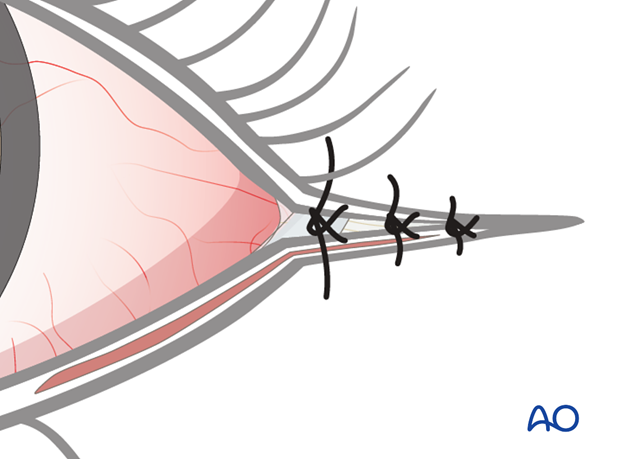
The lateral strip is attached either to the upper limb of the canthus or the periosteum within the lateral orbital rim using a double armed 5.0 resorbable suture.

Most surgeons will slightly over correct the placement of the suture superior to the lateral canthal angle, which is just inferior to the frontozygomatic suture.
This is to ensure long term proper positioning of the lateral canthus.
Closure
Prior to tying the suture, the conjunctiva can be reapproximated with a 7-0 resorbable suture.
Lateral tarsal sutures are tightened.
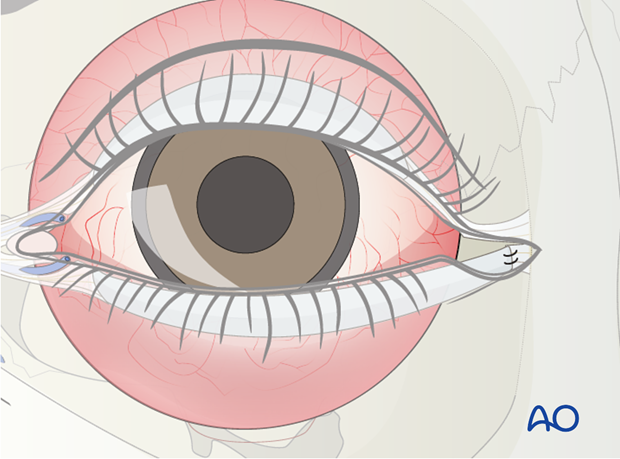
The muscle layer is repaired followed by skin sutures.
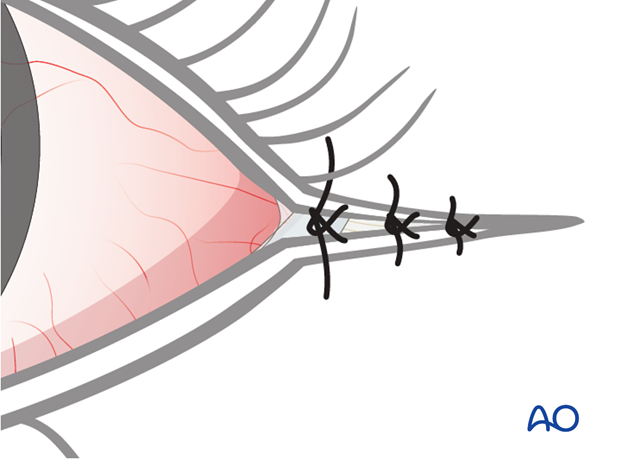
The ciliary margin including the grey line at the upper and lower eyelid junction is intentionally not sutured and left to heal secondarily. This often provides a better reconstruction of the lateral palpebral fissure compared to suturing and avoids rounding or blunting of the fissure.
4. Aftercare
Antibiotic drops are provided 3-5 days postoperatively.
Lubrication
It is important to maintain lubrication and protection of the eye.
Lubrication consists of natural tear substitutes during the day and ointment based lubricants during sleep, often together with taping the eyelid closed.
Protection
Physical protection through eyewear may be necessary depending on occupation and environmental conditions.













