Closed reduction
1. General consideration
Most pediatric palatoalveolar fractures can be treated conservatively or with closed reduction. The closed treatment will avoid devascularizing the bone and interference with growth, which occurs with open treatment, and therefore closed treatment should maintain growth potential in the pediatric palatoalveolar bone.
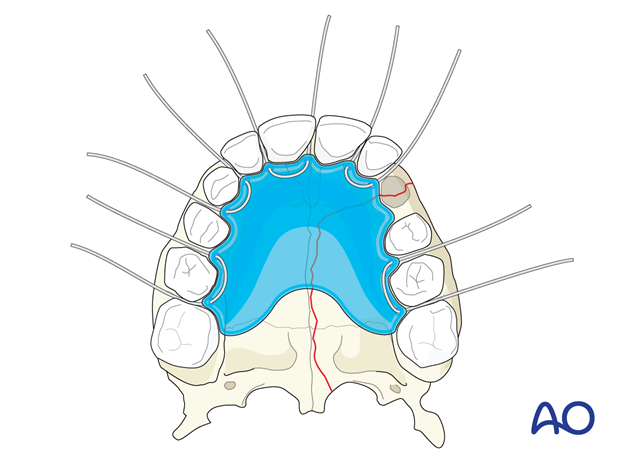
The goal of closed treatment is to realign the dental arch to its premorbid state and restore palatal width and occlusion. Due to the high rate of greenstick fractures, closed reduction is a very effective treatment in children.
2. Techniques
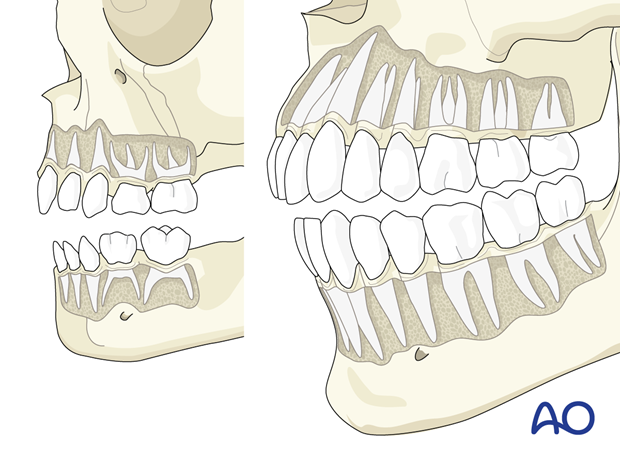
Pediatric dentition (deciduous teeth) is dissimilar to adult teeth in regard to the shape of the crown and root length. The deciduous teeth are not bell-shaped and have shorter roots than adult teeth, making them more difficult to ligate with circum-dental wires and more susceptible to avulsion.
The use of dental cast and fabrication of acrylic splints is the most widely used technique. However, with the advent of cone-beam CT and rapid 3D printing becoming more available in hospital centers, digital workflow has replaced the traditional dental cast technique.
Depending on the age of dentition, the technique can vary.
Deciduous dentition only
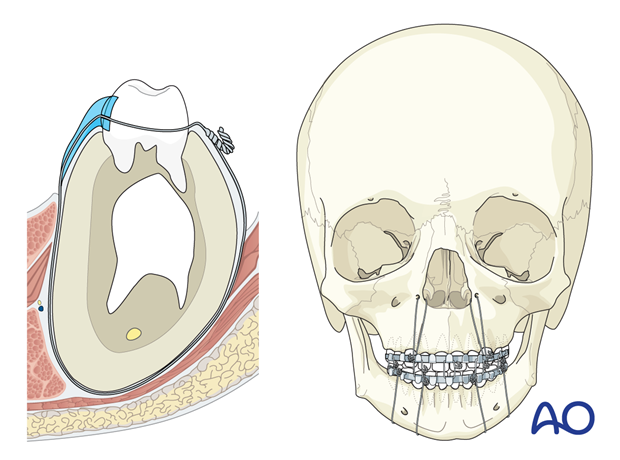
Acrylic splint fabrication and monomaxillary or bimaxillary fixation with circummandibular wiring/pyriform aperture wiring.
Mixed dentition (deciduous and permanent teeth)
Acrylic splints over arch bars.
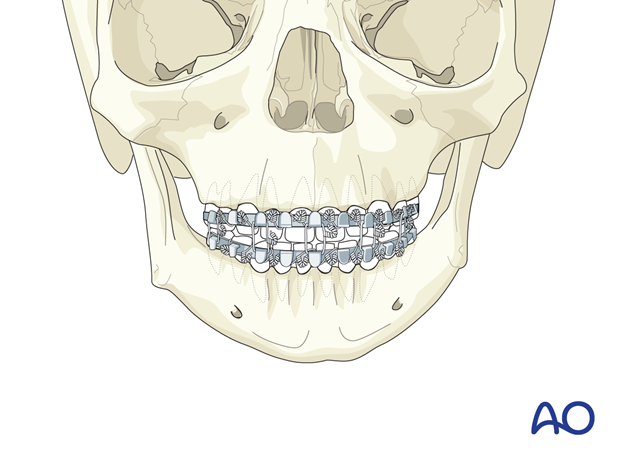
Permanent dentition
Arch bar fixation with or without a palatal splint.
Intramedullary fixation screws
The use of IMF screws is not generally advised in the pediatric population due to the presence of developing tooth buds within the mandible and the maxilla. If screws are used, they can only safely be placed below the anterior nasal spine and in the menton, where there are generally no tooth buds.
For a detailed description of closed treatment techniques, please refer to the CMF adult trauma section.
3. Aftercare
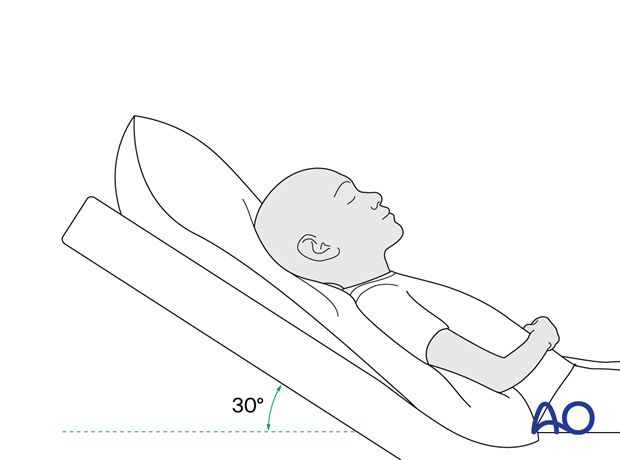
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make solid recommendations for postoperative care.
- No aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) prescribed for 7 days.
- Provide analgesia as necessary.
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable). More information can be found in the article: Mundinger GS, Borsuk DE, Okhah Z, et al. Antibiotics and facial fractures: evidence-based recommendations compared with experience-based practice. Craniomaxillofac Trauma Reconstr. 2015 Mar;8(1):64-78.)
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Regular perioral and oral wound care must include disinfectant mouth rinse, lip care, etc.
Postoperative imaging
Postoperative imaging should be performed within the first days after surgery to assess reductions and possible malpositioning. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Diet
Diet depends on the fracture pattern.
A soft, non-chew diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Intranasal feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Patients in MMF will remain on a liquid diet until such time the MMF is released.
Clinical follow-up
Close clinical follow-up is essential in children due to their high incidence of ankylosis and sometimes difficult postoperative compliance. Children should avoid all contact sports for a minimum of 6 weeks following dentoalveolar fractures; occlusal splints during sport are recommended for the first year following trauma.
Long-term follow-up is recommended to ensure that there are no facial and tooth growth disturbances.
MMF
The duration and use of MMF are controversial and highly dependent on the particular patient and the complexity of the trauma. In children, MMF should be for the shortest duration possible to minimize the risk of TMJ ankyloses (if the fractures involve the head of the condyle).
Oral hygiene
A soft infant toothbrush should be used to clean the teeth surfaces. Nonalcoholic oral mouth wash should be prescribed and used at least three times a day and after meals to help sanitize the mouth.













