Cleft lip and palate
Morphology
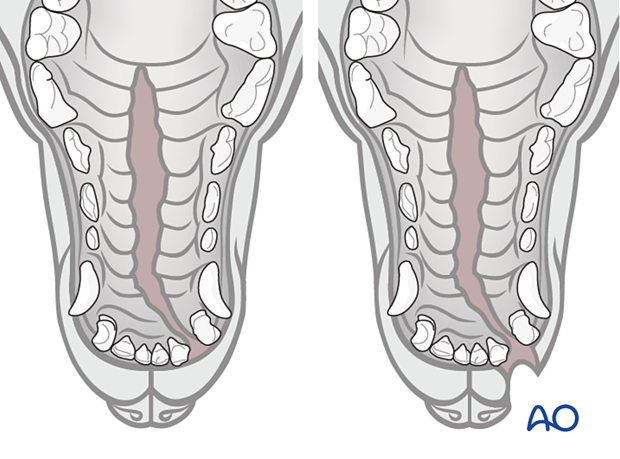
A cleft lip-palate (CLP) is a combination of a cleft palate (CP) that involves the structures of the secondary palate and a cleft lip (CL), which is a defect involving the structures of the primary palate.
The morphology of the defect/abnormality will depend on the type of cleft.
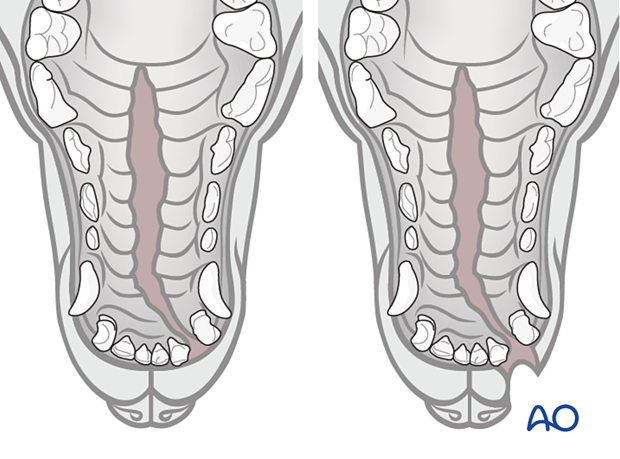
In small clefts, the incisive bones are aligned with the maxillary segments. In large bilateral clefts, the incisive bones are almost completely separated from the maxillary bones.
Epidemiology and etiology
Orofacial clefts affect ~3% of puppies (CL 26%, CP 59%, and CLP 15%). The incidence of orofacial clefts and the incidence of specific cleft phenotype varies across breeds. Brachycephalic breeds and mastiff/terrier breeds are predisposed to orofacial clefts. Clefts occur in 41.7% of offspring produced by phenotypically cleft parents, but the clefts' severity does not relate to the clefts' severity in parents.
Etiopathogenesis is complex and includes genetic and environmental factors (incl. teratogenic factors, nutritional factors, mechanical trauma, and geographic region).
Evaluation of the patient
A complete physical examination of the patient is needed to evaluate general health and possible concurrent congenital anomalies (cranial and extracranial). Animals with CP are presented due to poor body condition/growth, inability to nurse with drainage of milk from the nares during or after nursing, chronic nasal discharge due to respiratory infections such as rhinitis and/or aspiration pneumonia.

Oral examination findings may include malocclusion, and abnormal number and/or shape of teeth, mostly associated with maxillary incisor teeth.

Complete blood count and serum biochemistry are recommended, and the results are mostly indicative of inflammation, but may be normal.
Thoracic radiographs are indicated. If aspiration pneumonia is confirmed, a tracheal wash is suggested to determine appropriate antibiotic therapy based on culture and sensitivity testing.
The nasal cavity is examined for the presence of any complicating factors, such as nasal foreign bodies and fungal infection that may result in failure of surgical procedure. If any fungal infection is confirmed, this should be treated before a surgical repair is attempted.
In assessing patients for a palatal surgery, the defect's size and shape are evaluated under general anesthesia. CT imaging is recommended, and dental extractions, if needed, are done before cleft repair.
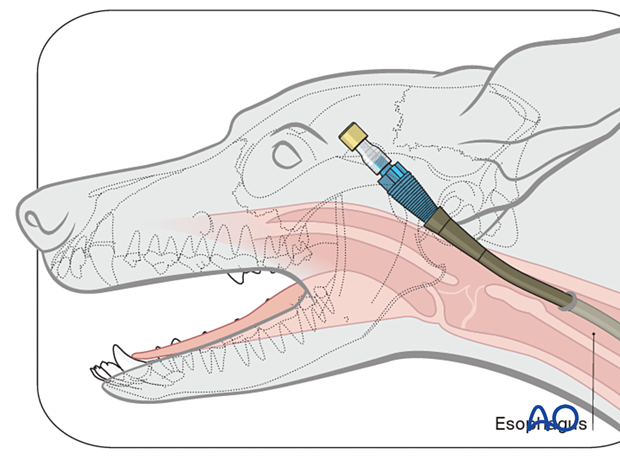
If the patient cannot eat independently, alternative routes of alimentation (e.g., esophagostomy or gastrostomy feeding tube) are needed.
Imaging
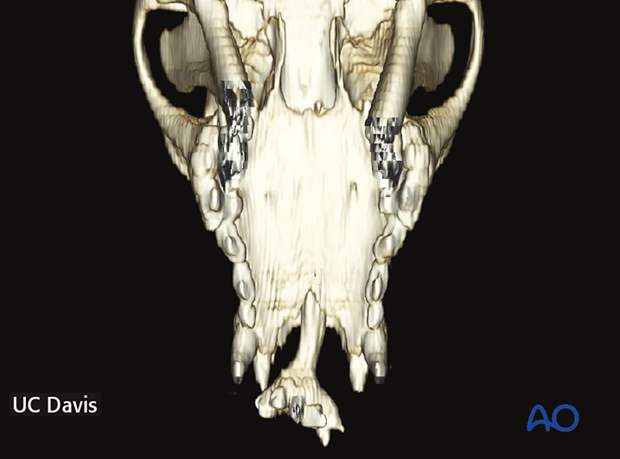
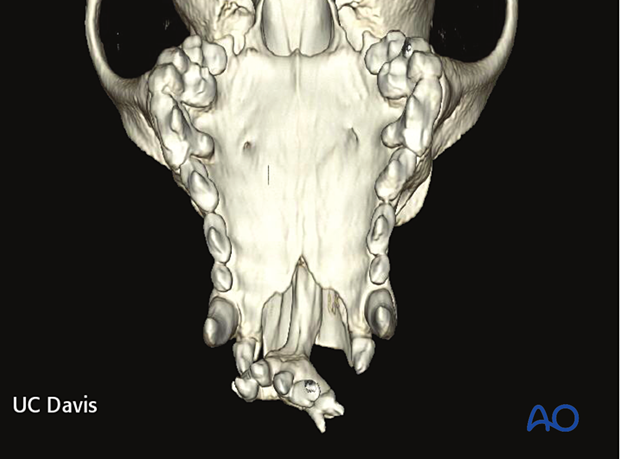
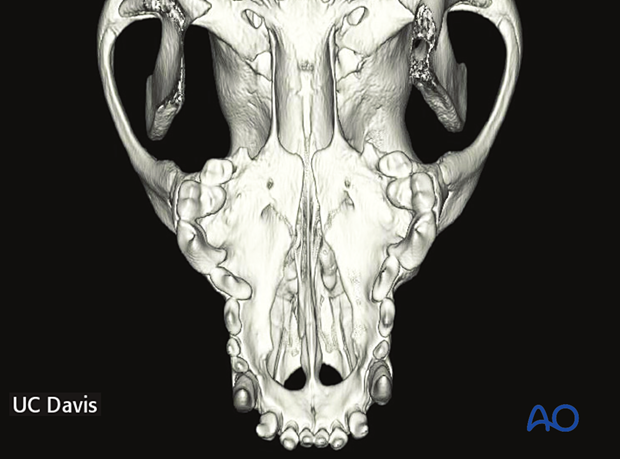
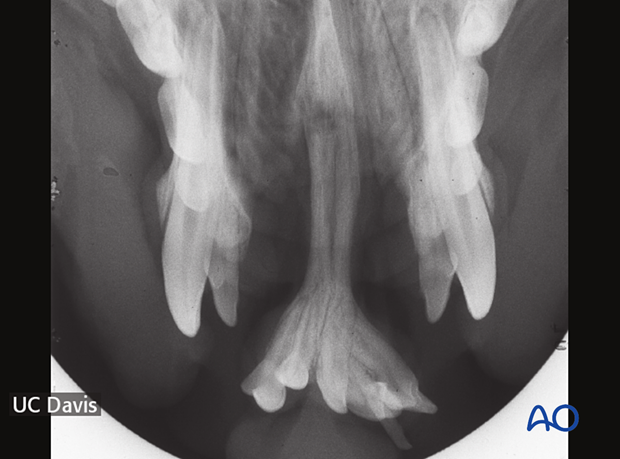
A CLP defect is a clinical diagnosis facilitated by radiographs, including occlusal intraoral radiograph and two (left and right rostral maxilla) lateral intraoral views obtained by a bisecting angle technique.
A CT and 3D reconstruction are recommended and performed to evaluate better the relationship between soft and hard tissues and to diagnose any coexisting craniofacial abnormalities.