Staged double-layer closure
1. First stage: extraction of maxillary teeth
Selective dental extractions of maxillary teeth 4 to 8 weeks before definitive closure of hard palate defect are performed.
The precise number and location of teeth extracted should be customized for every individual case based on defect size and location, quality, and quantity of surrounding soft tissues.
A custom-made vinyl polysiloxane temporary obturator is used.
Steps for placement:
- Mix the 2 components of the putty impression material following the manufacturer instructions
- Massage the putty to fill in and extend beyond the defect on the oral side
- Let the putty set as required by the manufacturer
2. Second stage: hard palate defect repair
Mucoperiosteal flaps
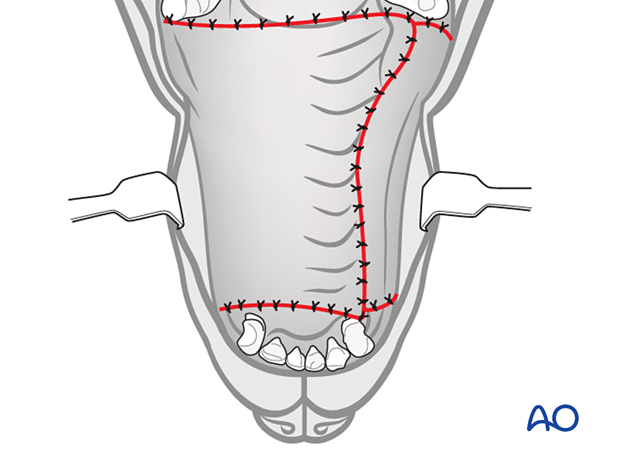
The surgical technique for definitive hard palate defect repair consists of creating 2 or 3 mucosal flaps to be applied using a double-layer approach.
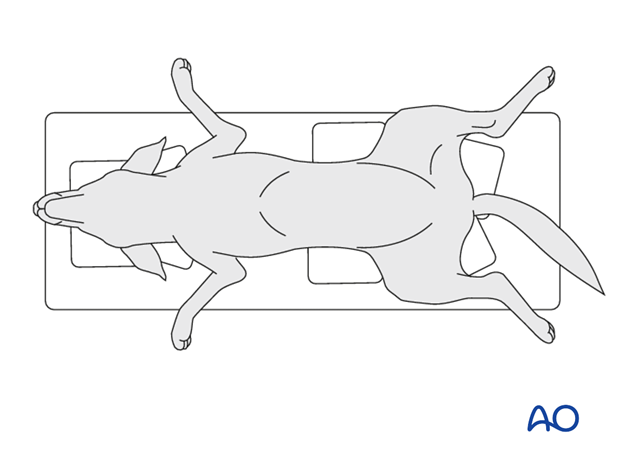
The patient is positioned in dorsal recumbency.
Maxillary or infraorbital nerve blocks are recommended during a cleft repair.
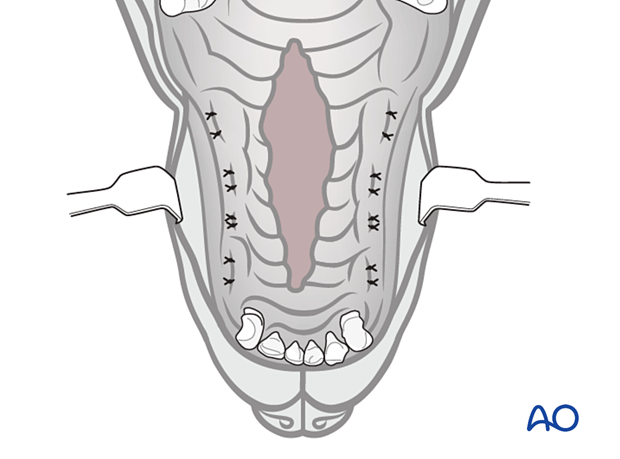
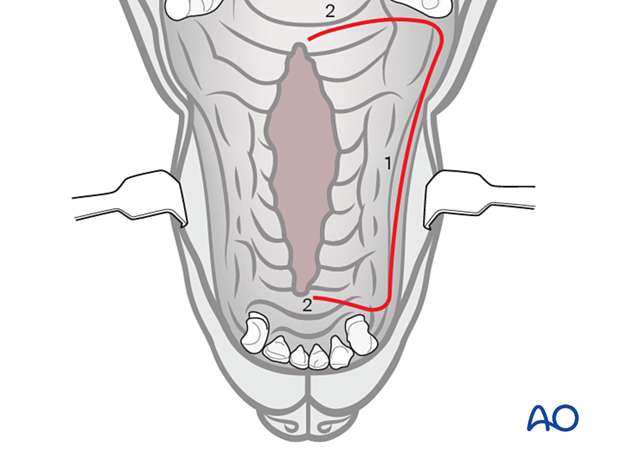
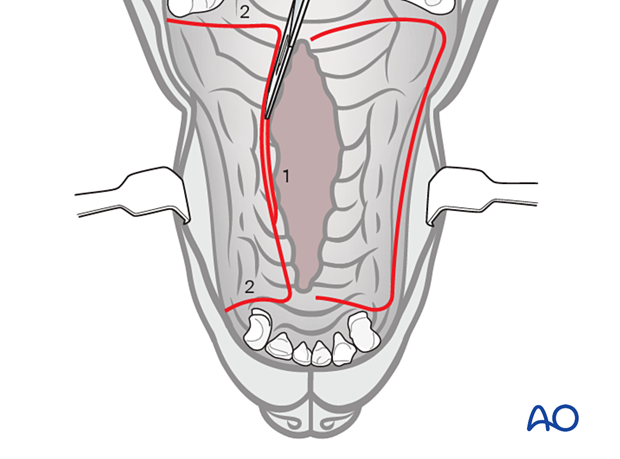
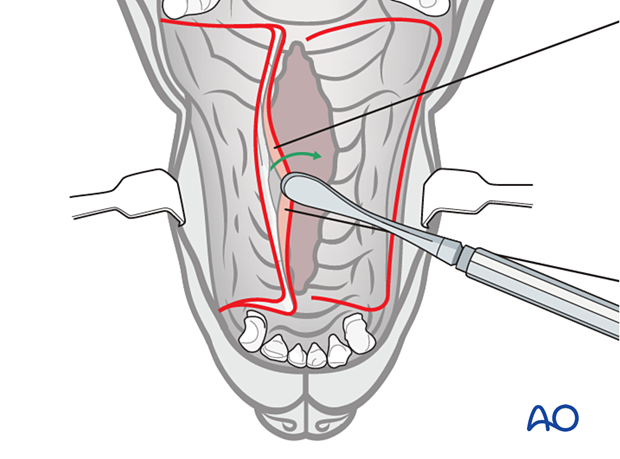
An incision (1) of the same length as the palatal defect is made on one of the cleft's side. The reflected flap must be large enough to cover the defect without tension.
Two perpendicular incisions (2) are made at the rostral and caudal ends extending to the cleft. The caudal incision must not lie over the soft palate to prevent the formation of an oronasal fistula.
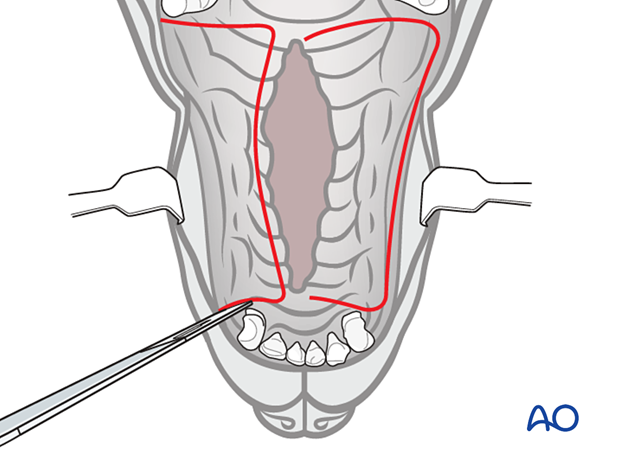
A single pedicle advancement flap is created on the opposite side. The flap made should be large enough to cover both the defect and the exposed palatal bone after the reflected flap creation.
The edge of the palatal mucosa at the defect edge is tangentially incised with a number 11 blade (1).
Two releasing incisions are created perpendicular to the cleft (2).
Use a periosteal elevator to create the single pedicle advancement flap.
Holes are created on the maxillary bone's exposed palatine process using either a small round diamond bur on an air-driven and water-irrigated high-speed handpiece or a Kirschner wire on a hand chuck. The holes are spaced approximately 3-5 mm away from each other and are aligned parallel to and approximately 2-3 mm away from the osseous defect's edge.
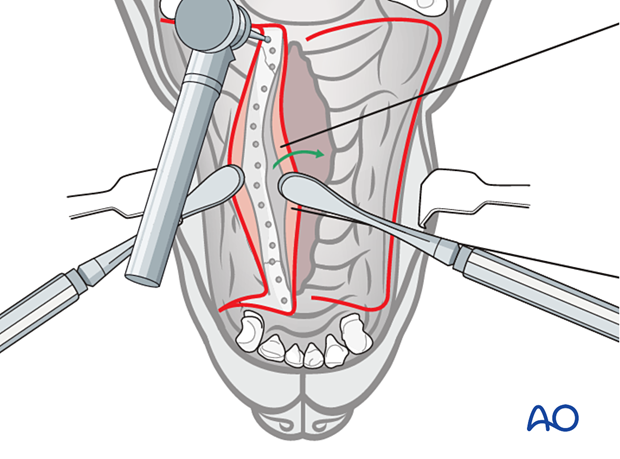
The reflected flap is raised using a periosteal elevator. Avoid trauma to the major palatine artery.
Bleeding is controlled by manual pressure and/or ligation of bleeding vessels.
Careful elevation is needed to avoid perforation of the flap base where the oral and nasal mucosa meet.
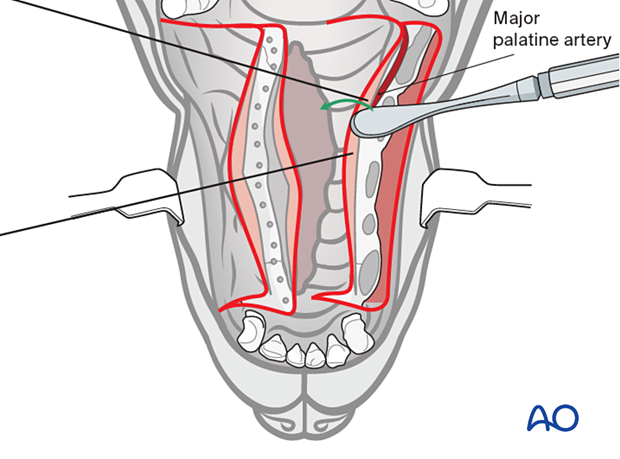
The reflected flap is reversed and secured to the holes with preplaced sutures.
3-0 or 4-0 rapidly resorbable monofilament suture material is used in a single interrupted or a horizontal mattress pattern to secure the flap to the palatine process of the maxillary bone.
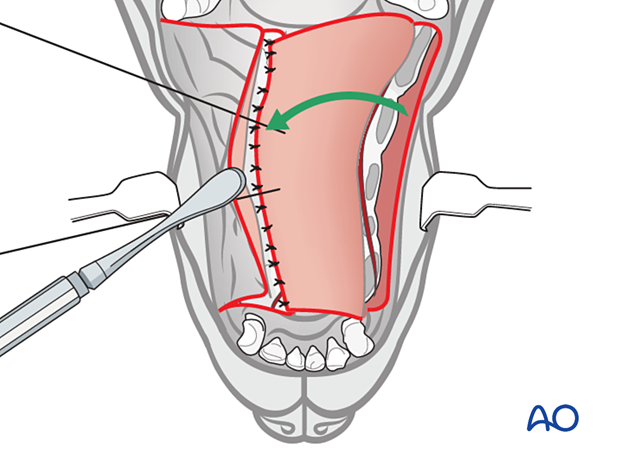
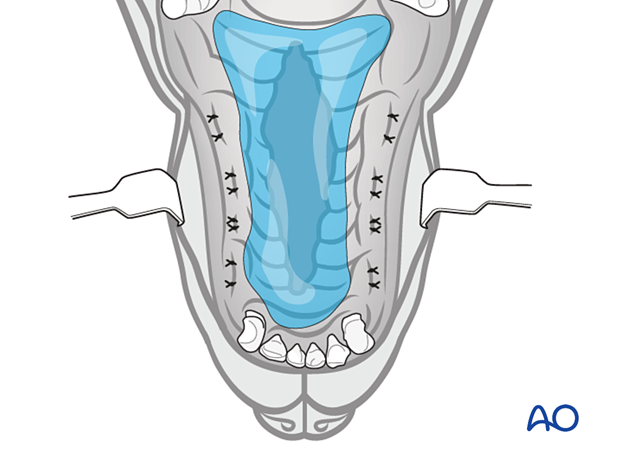
The single pedicle advancement flap, if large enough, is sutured to the soft tissue on the opposite side...
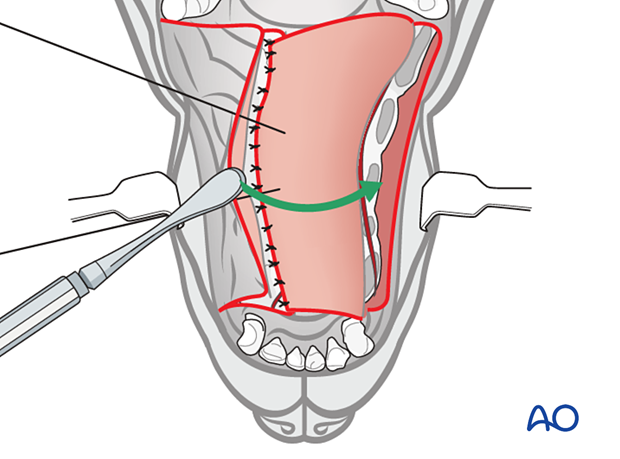
...covering the entire defect.
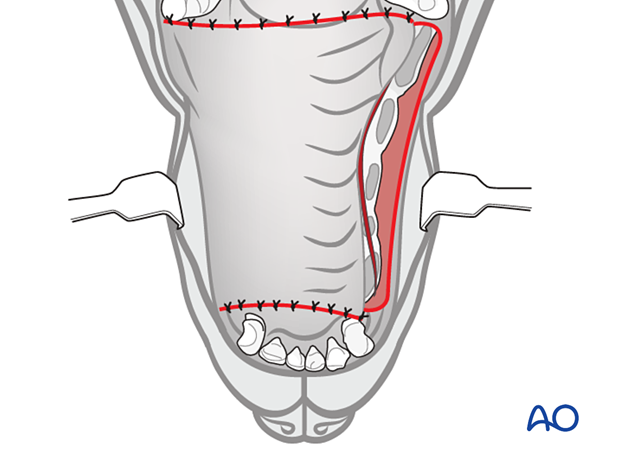
3. Variation with a third flap
A third flap is used if the first flap was not sufficient to cover the palatal bone's denuded area on the side of the reflected flap.
An alveolar and buccal mucosa single pedicle advancement flap is created on the ipsilateral side to the reflected flap.
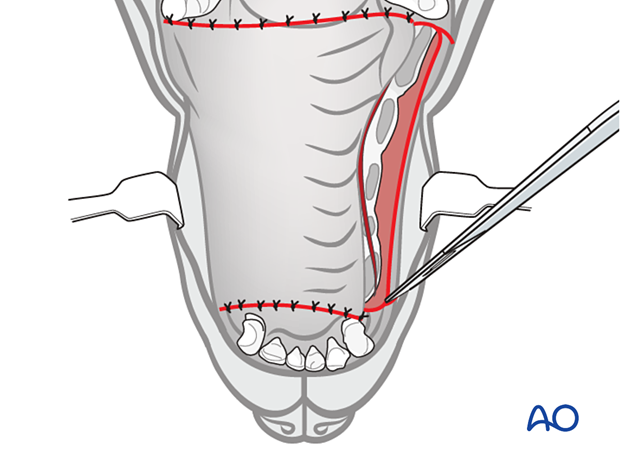
Care is taken to preserve the infraorbital neurovascular structures when incising or dissecting directly over them.
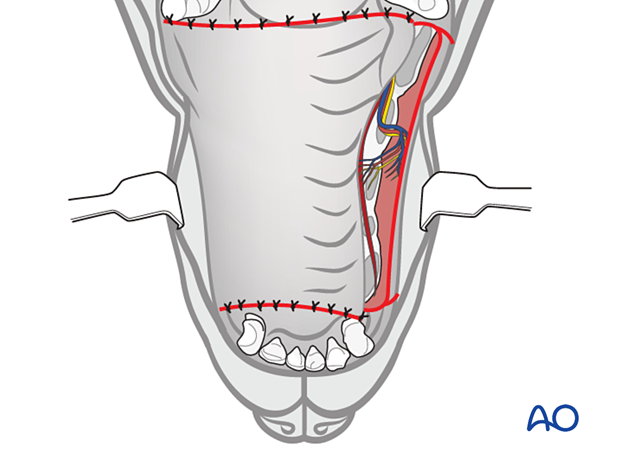
Once released, the flap is advanced and secured to the edge of the contralateral single pedicle advancement flap using 4-0 rapidly resorbable monofilament suture material in a simple-interrupted pattern.
Closure under tension
If there is tension on the suture line, dehiscence will likely occur.
If dehiscence occurs and the defect is clinically significant, the repair is delayed for 4-6 weeks to allow the tissues to heal.
4. Aftercare
Medications
Multimodal perioperative analgesia is provided by combining opioids and non-steroidal medications. Analgesia is provided for 5-7 days postoperatively.
A broad-spectrum antibiotic is continued for 10-14 days postoperatively depending on the nature, complexity, and duration of the surgical procedure and the presence of complicating factors (e.g., rhinitis).
Monitoring
Postoperative monitoring is required. Evaluate for oral swelling and impaired breathing. The patient is hospitalized overnight, and the surgical site is checked the next day. The surgical site is then evaluated weekly until healing is confirmed (6 weeks postoperatively). Skin sutures in cases of cleft lip repair should be removed 10-14 days postoperatively.
The most common complication is dehiscence. If it occurs and the resulting defect is of clinical significance, then repair is delayed for 4-6 weeks to allow the tissues to heal.
Diet
Although the placement of a feeding tube (e.g., esophagostomy or gastrostomy) could be considered, in most cases, oral intake of food can begin following complete recovery from anesthesia. A liquid or a soft blended diet is used for 2 weeks, followed by a slow conversion to a soft diet over the following 2 weeks. Chew toys must be avoided for 6 weeks.
Oral hygiene
The oral cavity should be carefully rinsed twice daily with an antiseptic oral rinse (e.g., chlorhexidine gluconate 0.12%).
5. Case example: Cleft of the hard palate repaired with a staged double-layer overlapping flap technique
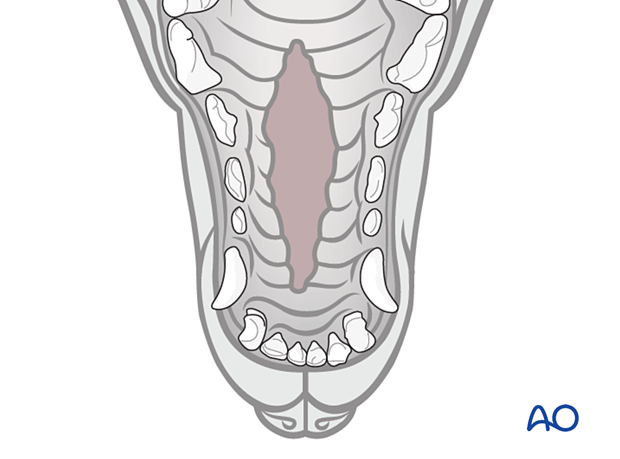
Midline cleft of the hard palate.

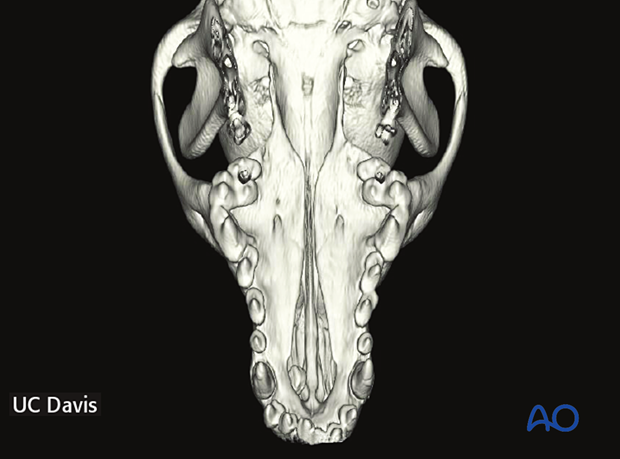
Preoperative 3D CT image showing a large bony defect in the area of palatine fissures compared to the soft tissue defects.
CT is needed for correct surgical planning to evaluate the size and shape of the bony defect.
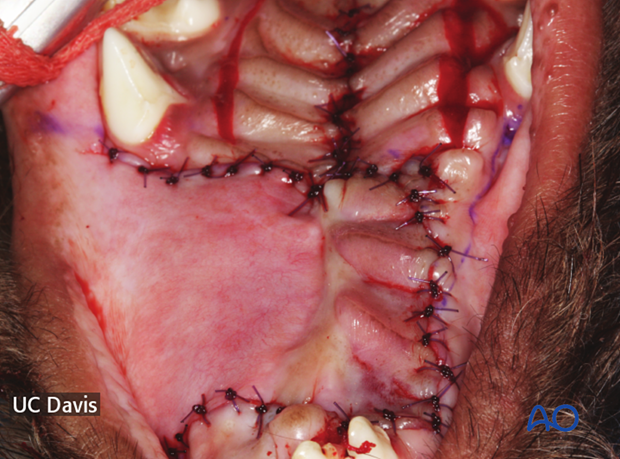
Six weeks after selective dental extractions, the rostral part of the hard palate defect was repaired with a double-layer technique.
The narrower defect in the caudal aspect of the hard palate was repaired using a von Langenbeck technique.