Prone position for approaches to C0–C7
1. Positioning
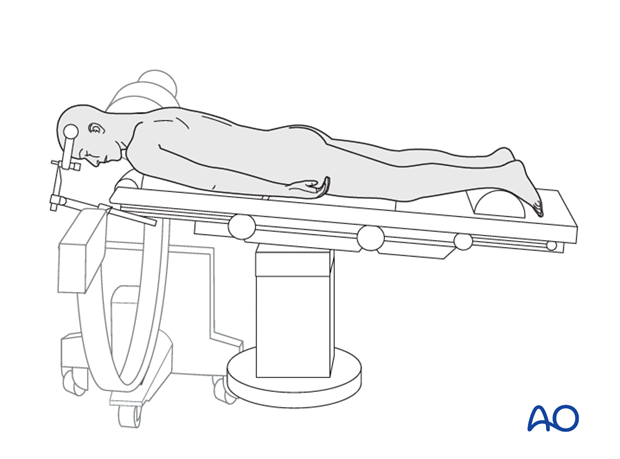
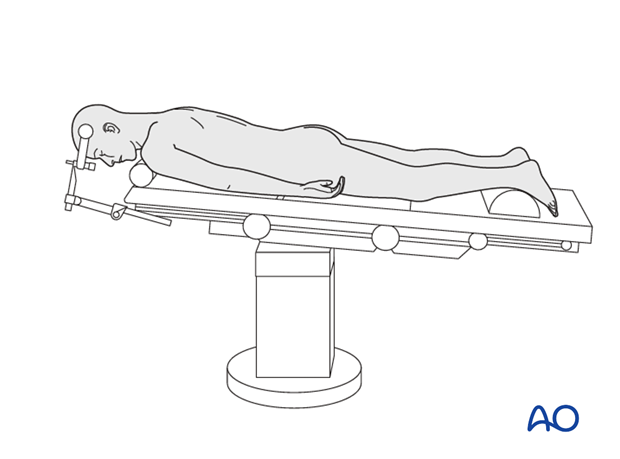
The patient can either be positioned on a radiolucent table or a Maquet table, prone on two horizontally placed padded bolsters (one at the level of the sternum and the other one at the level of anterior iliac spine or on a frame.
- The abdomen should hang free to avoid increased intraabdominal pressure and to prevent excessive bleeding
- Adequate padding needs to be provided to elbows and knees to avoid pressure sores
- The head is rested on a Mayfield three-pin head holder to avoid pressure on the eyes
- The arms are positioned safely downwards without any pressure points
When using a Mayfield head holder, select the pin entry points so that the clamp can be rotated freely over the nose once the patient is put into the prone position. To facilitate exposure, the cervicothoracic junction is extended, and the upper cervical spine is flexed.
Make sure that there are adequate personnel to receive and turn the patient from a supine to a prone position on the operating table if needed.
In patients with unstable tumors, who are at risk of neurological deterioration during positioning, baseline electrodiagnostic signals can be obtained to allow for comparison after positioning. Other options in high-risk patients include awake positioning or a wake-up test after positioning.
Using a ‘spinal cord at risk’ protocol is recommended in cases where intraoperative neurological deterioration is expected.
2. Anesthesia
With highly unstable cervical tumors, either an awake or fiberoptic intubation should be considered. In patients with severe spinal cord compression, it is essential to avoid hypotensive anesthesia, and the mean arterial blood pressure should be maintained above 80 mmHg.
3. Preoperative antibiotics
Antibiotics should be administered 30–60 minutes prior to the incision.
A cephalosporin antibiotic with good Gram-positive coverage is generally recommended.
4. Spinal cord monitoring
Spinal cord monitoring is optional and should be considered in cases with severe spinal cord compression or when spinal cord manipulation is anticipated.
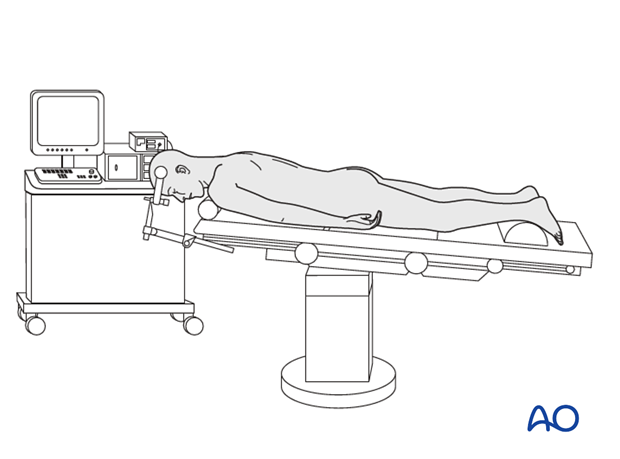
5. Fluoroscopy/x-ray control
The incision can be planned based on the lateral x-ray.
An intraoperative CT scan can be used together with spinal navigation. This can assist in instrumentation placement, osteotomy cuts, and tumor delimitation.