Malignant tumors L1 to L5
Chondrosarcoma
Chondrosarcomas typically occur in the fifth decade of age with a male predominance (2:1). They represent 10% of all malignant primary spinal tumors and typically occur in the thoracic spine.
The prognosis depends on the location, size, and histological grade of the lesion. There is an overall five-year survival rate of 48–60% (90% for grade 1, 81% for grade 2, and 29% for grade 3 tumors). High-grade lesions have a propensity to metastasize.

Clinical presentation
- The most common clinical complaint is dull, aching back pain.
- Pain may be most severe at night.
Radiology
Often a large, lytic mass with a chondroid matrix. Higher-grade lesions tend to have larger areas without calcification.
Histological characteristics
- A lobulated tumor composed of hyaline nodules and focal ivory-like areas representing extensive enchondral ossification.
- Regions of hemorrhage and necrosis may be present in high-grade lesions.
- Microscopically, irregular-shaped lobules of cartilage are separated by narrow, fibrous bands.
- Grade 1 lesions are diploid, grade 2 and 3 lesions are aneuploid.
- Immunohistochemistry positive for S-100 protein and vimentin.

Treatment principles
- En bloc excision with wide surgical margins is the treatment of choice.
- Entry into the tumors leads to earlier local recurrence and shorter overall survival.
- The role of chemotherapy is limited.
- High-dose radiation therapy should be considered with positive margins.
Osteosarcoma
Osteosarcomas typically occur in the fourth decade of age with no gender predominance. Patients with secondary lesions tend to be older (> 60 years).
They account for 0.85–2% of primary osseous malignancies and may be primary or secondary (postirradiation).
Patients with these tumors have a poor prognosis, with a median survival of less than two years.
Clinical presentation
The most common clinical presentation is the insidious onset of nocturnal back pain.
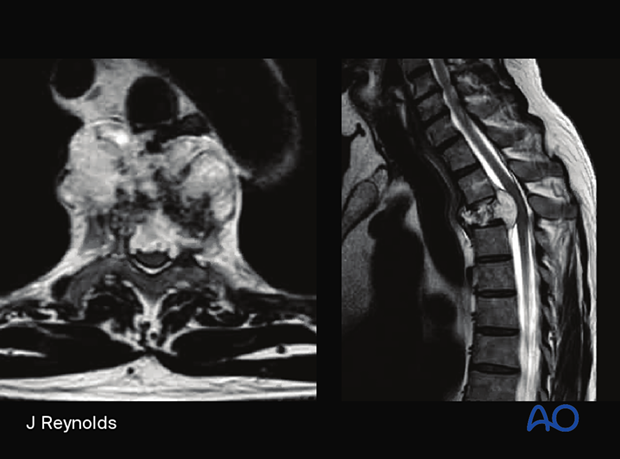
Radiology
Typically arises in the posterior elements. An aggressive lesion with sclerosis due to the production of immature bone. Margins are difficult to delineate.
Histological characteristics
- Grossly, the tumor appears as a heterogenous mass with ossified and unossified components.
- Microscopically, the tumor is characterized by malignant-appearing spindle-shaped or round cells with a high degree of anaplasia and a high mitotic rate.
Treatment principles
En bloc excision with wide surgical margins is the treatment of choice. Entry into the tumors leads to earlier local recurrence and shorter overall survival. Adjuvant and neoadjuvant chemotherapy/radiation therapy is beneficial.
Ewing’s sarcoma
Ewing’s sarcoma typically presents before 20 years of age, although a second smaller peak in the fifth decade is present. There is a 2:1 male-to-female ratio.
Five percent of all Ewing sarcomas occur in the spine. The sacrum is the most common site. It may spread along the course of peripheral nerves.
Clinical presentation
- Localized pain
- Fever, leucocytosis, and elevated inflammatory markers
- Neurological symptoms due to neural element compression
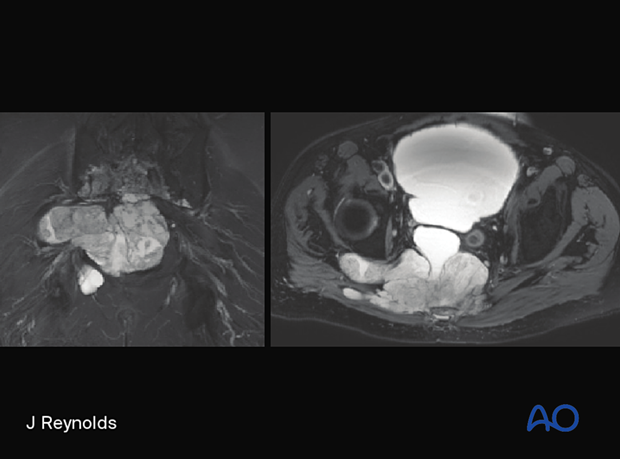
Radiology
Aggressive and permeative lytic lesion of vertebral body or sacrum. Can be associated with large soft tissue mass. Heterogenous contrast enhencement.
Histological characteristics
Grayish–white tumor with areas of hemorrhage and necrosis. Microscopic features include small round blue cell tumors and a high mitotic rate.
Treatment principles
Ewing sarcomas are treated with neoadjuvant chemotherapy. Aggressive en bloc resection with wide margins after chemotherapy can be associated with decreased local recurrence. Radiation therapy is used for incompletely resected tumors.
Chordoma
Chordomas typically occur in the fifth to sixth decade of age with a male predominance (2:1). They account for 2–4% of malignant primary osseous neoplasms and are the most common primary sacral neoplasms. 50% occur in the sacrum/coccyx, 15% in the skull base, and 15% in the vertebral bodies.
This is a very slow-growing tumor with a high rate of local recurrence (up to 90% in some series), especially with intralesional excision. Distal metastasis is seen in up to 5% of patients.
Clinical presentation
Clinical presentation depends on the location. The patient may present with pain, numbness, or weakness. Sacral lesions may present with a gluteal mass.
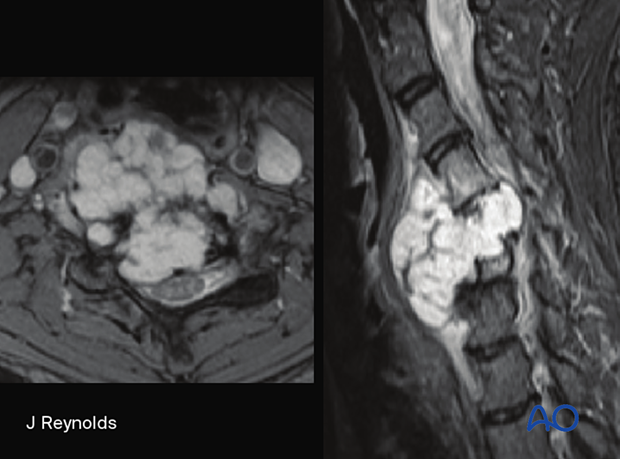
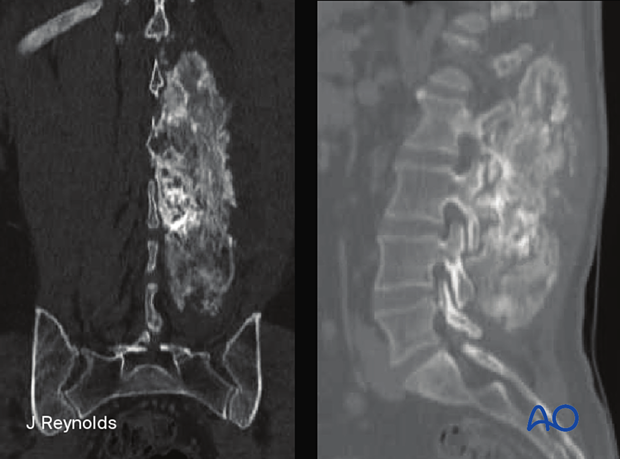
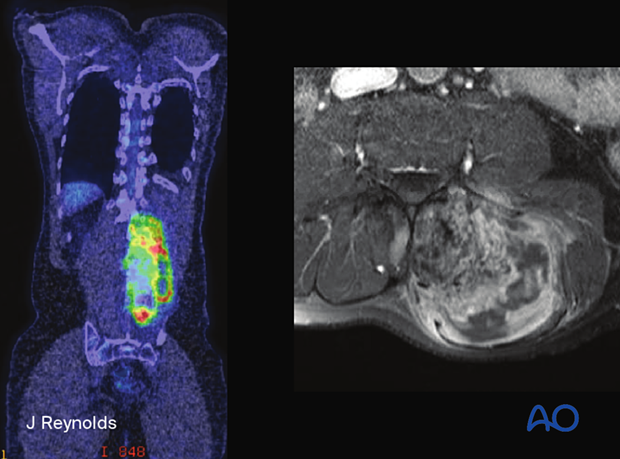
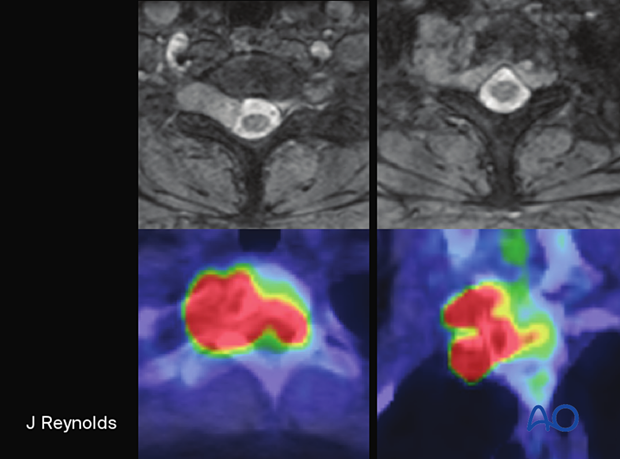
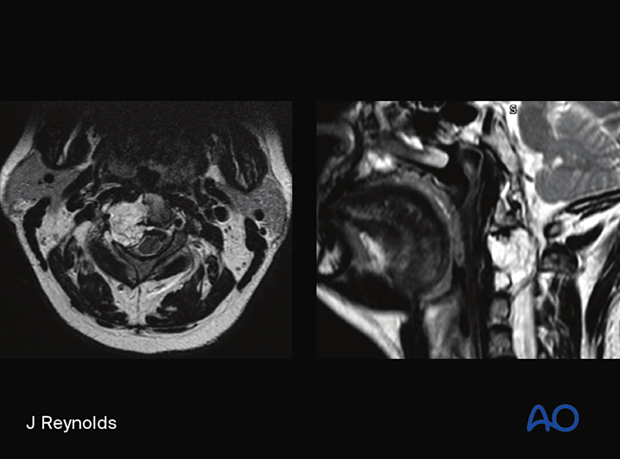
Radiology
Destructive lesion associated with large soft tissue mass. Hyperintense on T2 weighted images.
Histological characteristics
- Tumor arises from notochordal remnants
- Locally invasive
- Lobulated masses with a gelatinous texture
- Two subsets: typical chordomas and chondroid chordomas. In the typical variant, variable amounts of intracellular mucin are embedded in pools of extracellular mucin; in the chondroid variant, this gelatinous mucinous matrix is replaced by cartilaginous foci.
- Histologically, physaliferous cells are a hallmark
Treatment principles
En bloc resection with a wide margin yields the best clinical outcomes. There is a very limited role for traditional radiation therapy, although newer techniques such as proton beam and carbon ion radiotherapy have shown promise.
High-dose adjuvant radiation is recommended if margins are positive.
Biopsies must be planned with future tumor excision in mind so that the biopsy tract can be excised at the time of surgery.













