Neurological examination
1. Spinal cord anatomy
Knowledge of spinal cord anatomy is crucial for the interpretation of the results of the physical examination.
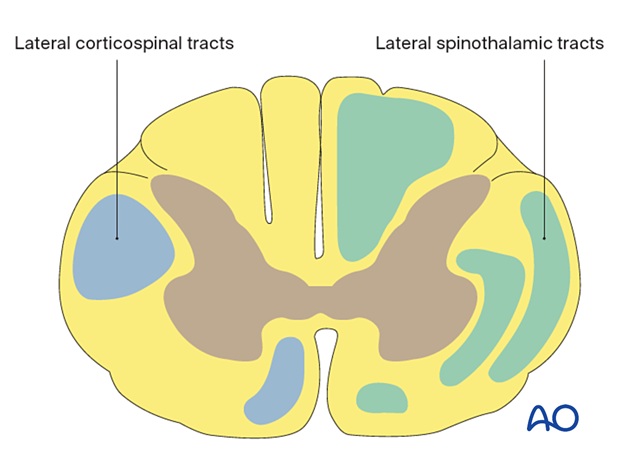
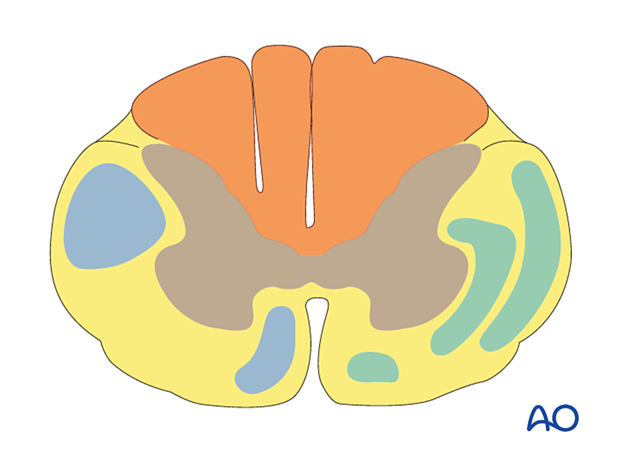
- The lateral spinothalamic tracts are responsible for transmitting pain and temperature sensation
- The lateral corticospinal tracts are responsible for motor function
- These tracts carry a specific topographical organization
- The most central portions represent the function of the more proximal areas of the body, and the more peripheral portions represent the function of the distal areas of the body
- The posterior columns transmit position sense, vibratory sensation, and deep pressure sensation
2. INSCI
To assess the neurologic status of the patient, the International standards for neurological classification of Spinal Cord Injuries (INSCI, formerly referred to as the ASIA standards) are used systematically.
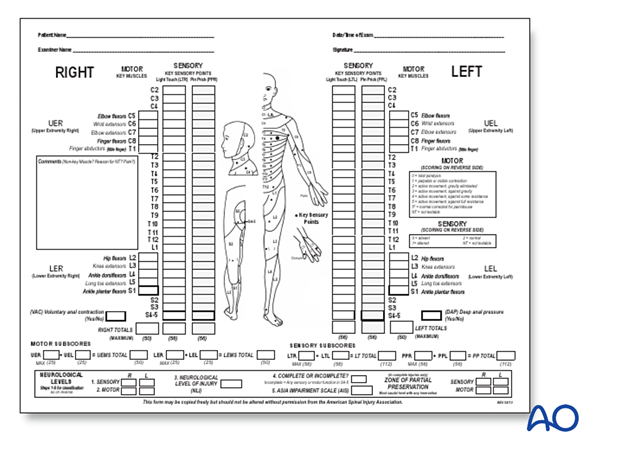
3. Motor function
Manual Muscle Testing (MMT) of the following key muscle groups in the upper and lower extremities should be performed.
There are six levels of muscle strength, ranging from 0–5, as indicated on the INSCI assessment sheet.
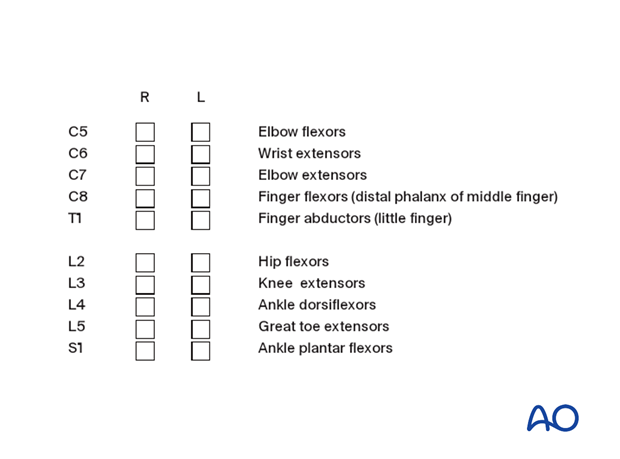
Examine the strength of key muscle groups in the upper limb. The key muscles are listed below, along with the spinal cord level in parentheses.
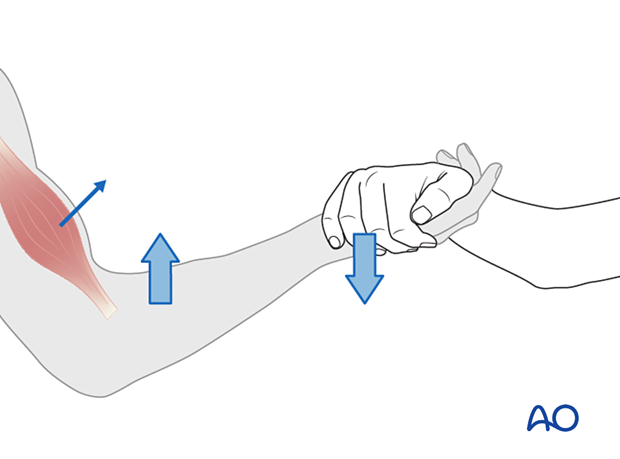
Elbow flexors (C5)
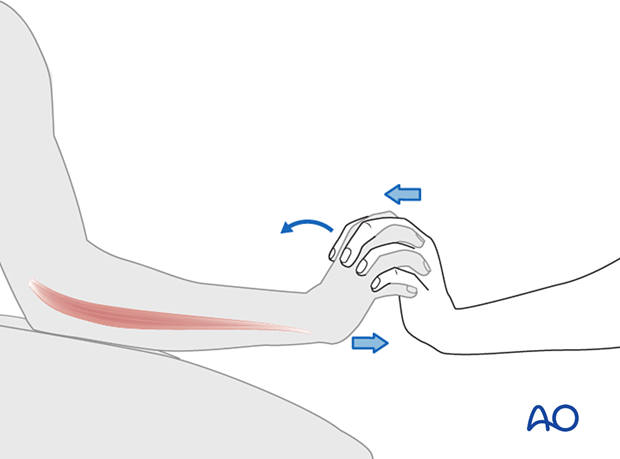
Wrist extensors (C6)
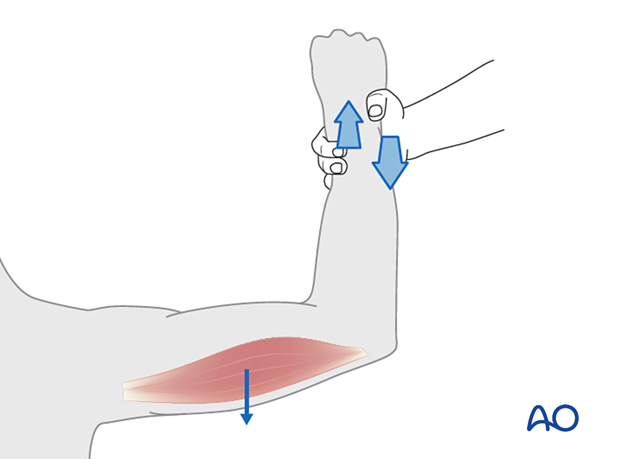
Elbow extensors (C7)
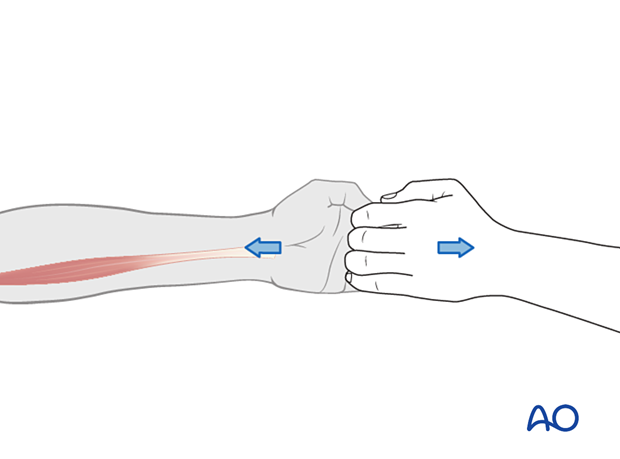
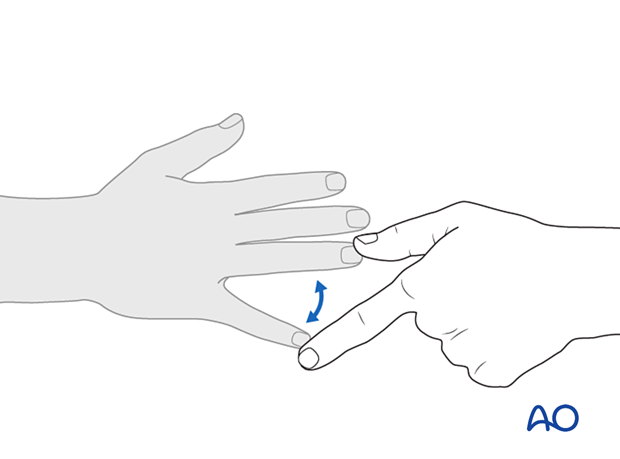
Finger flexors (C8)
Finger abductors (T1)
Examine the strength of key muscle groups in the lower limb.
Hip flexors (L2)
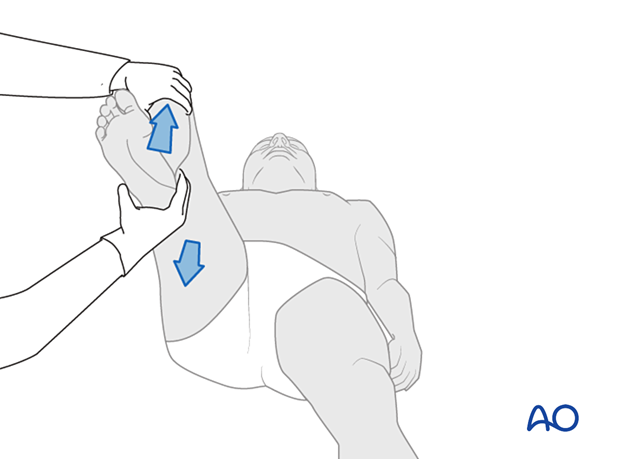
Knee extensors (L3)
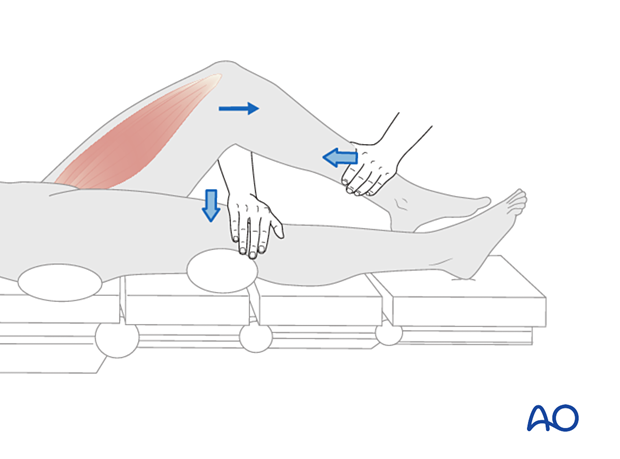
Ankle dorsiflexors (L4)
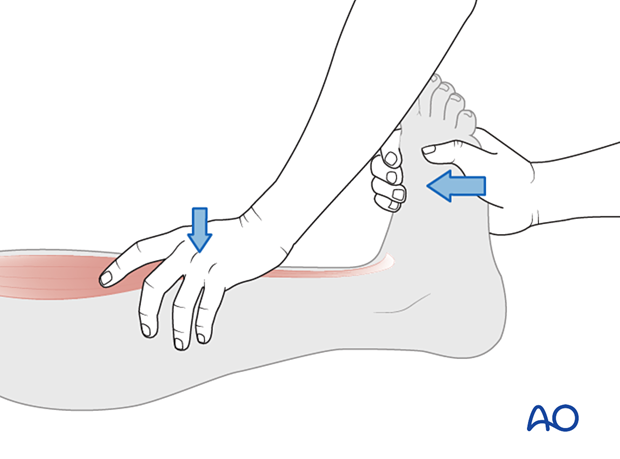
Great toe extensors (L5)
Ankle plantar flexors (S1)
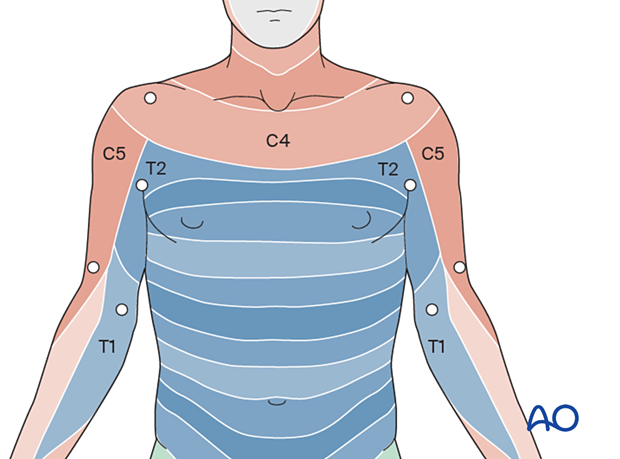
4. Sensory function
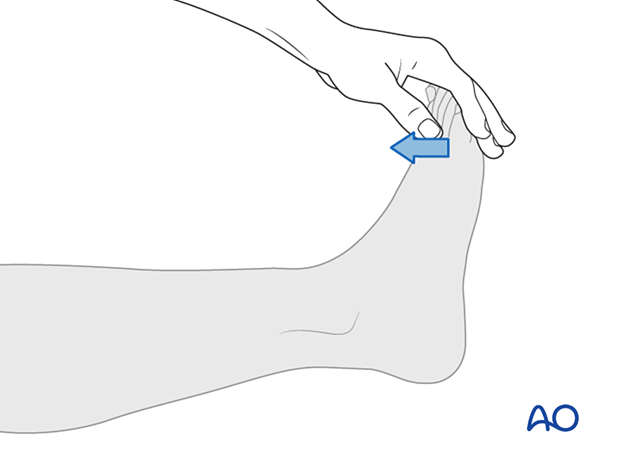
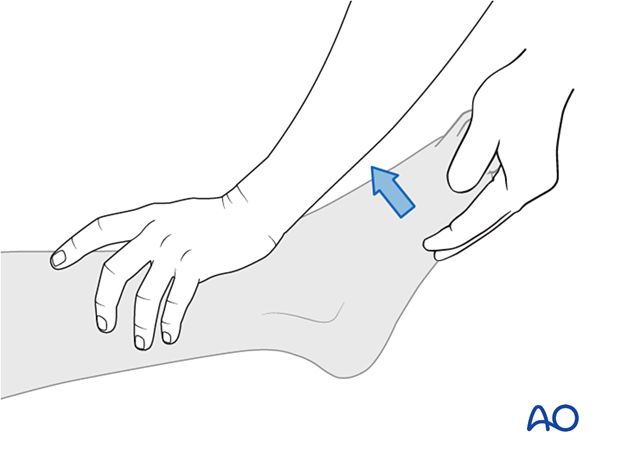
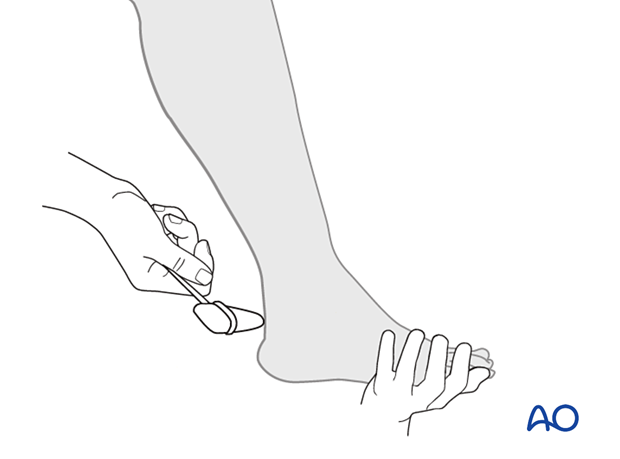
Pinprick sensation is assessed with a needle. Light touch sensation is assessed with a piece of tissue paper.
Sensation is scored as absent (0), abnormal (1), or normal (2).
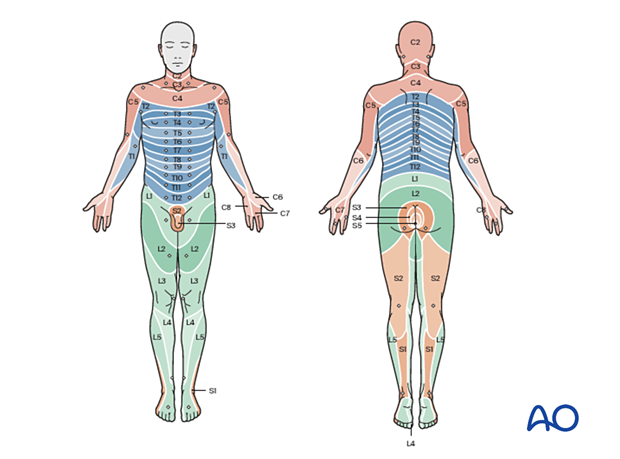
- Because the C4 sensory level extends below the clavicle just above the T2 dermatome, a mid-cervical neurological injury level is often misinterpreted as being at the thoracic level. C5 through T1 are in the arms. The T2 dermatome includes the medial forearm, the axilla, and the upper chest.
- The left and the right need to be examined separately and are not always the same.
5. Reflex examination
The upper and lower extremities should be examined for asymmetry in deep tendon reflexes.
In the setting of an acute spinal cord injury, deep tendon reflexes are absent below the level of injury.
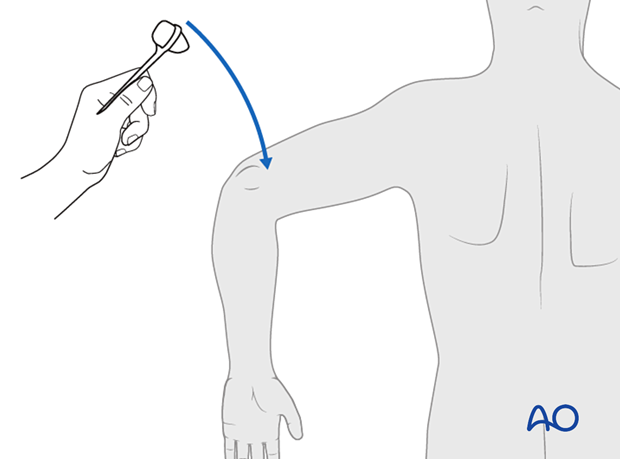
The upper extremity reflexes are listed below, with the corresponding neurological level in parentheses.
Biceps reflex (C5)
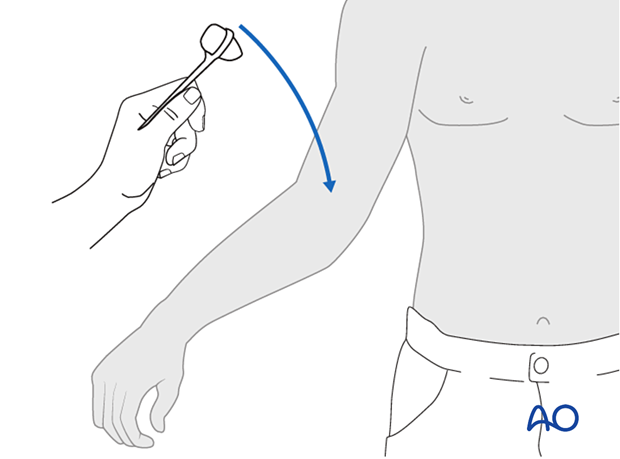
Brachioradialis reflex (C6)
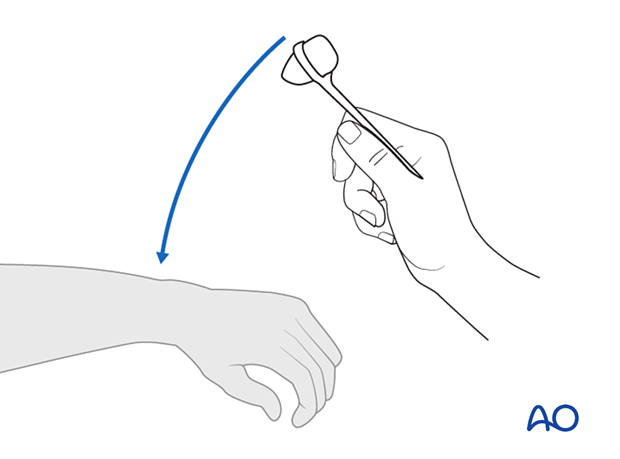
Triceps tendon reflex (C7)
Knee tendon (L4)
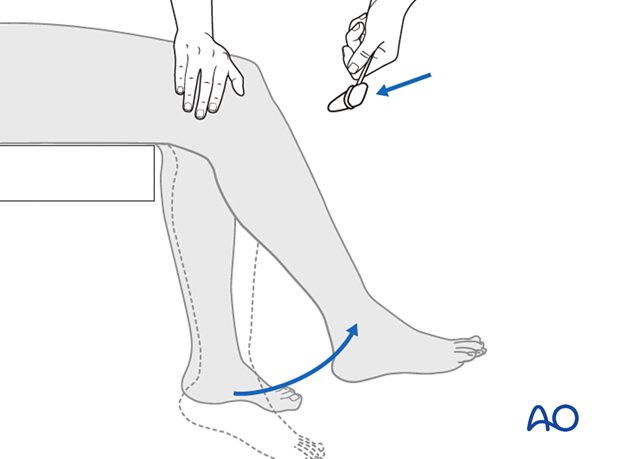
Achilles tendon (S1)
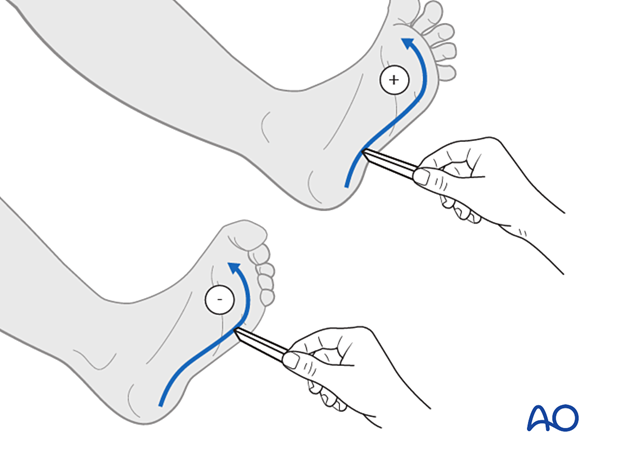
Pathological reflexes:
Clonus and Babinski reflexes should be assessed. If positive, this may be an indication of spinal cord dysfunction.
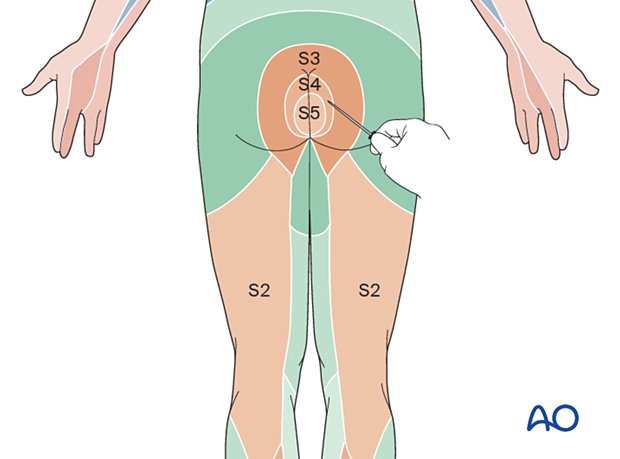
6. Sacral sparing tests
Because the sacral roots are most caudal, the presence of any sacral root function indicates the absence of complete spinal cord injury, which impacts both treatment and prognosis.
A rectal examination should be performed to assess for anal sphincter tone as well as proprioception and perianal sensation. Anal sphincter tone should be scored as absent, flaccid, reduced, or normal.
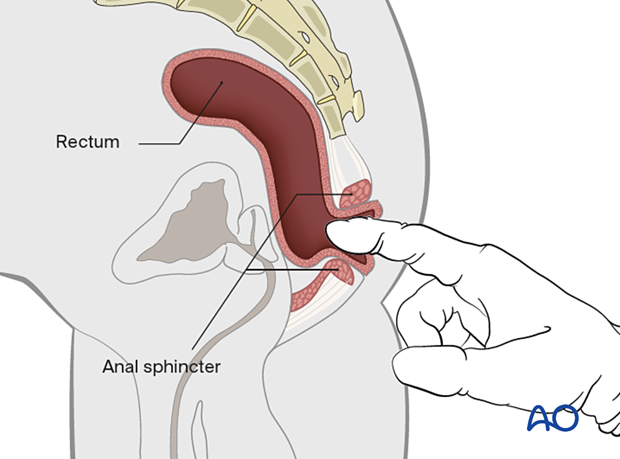
The anal sphincter allows for the most caudal assessment of motor innervation.
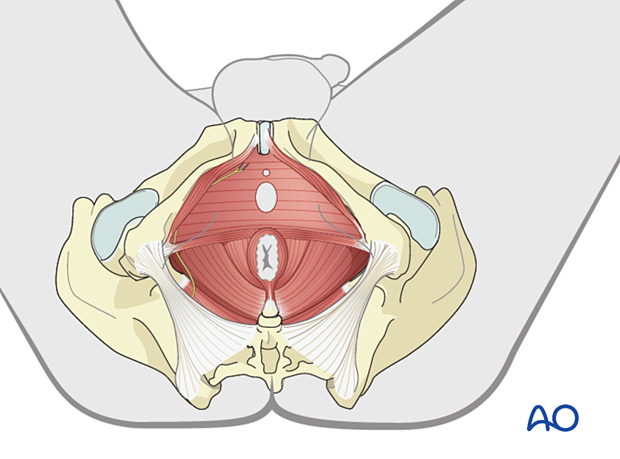
The S2–5 dermatomes should be assessed for pinprick and light touch sensation.
7. Clinical Syndromes in SCI
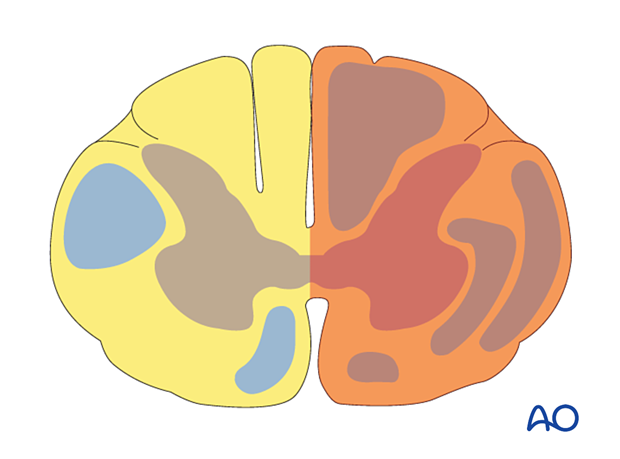
Brown-Sequard syndrome is caused by a hemi section of the spinal cord.
Clinical presentation:
- Unilateral lateral column damage results in ipsilateral muscle paralysis
- Injury to the dorsal column results in an ipsilateral loss of joint position sense, vibratory sense, and tactile discrimination
- Damage to the lateral spinothalamic tracts results in loss of pain and temperature sensation on the contralateral side of the body
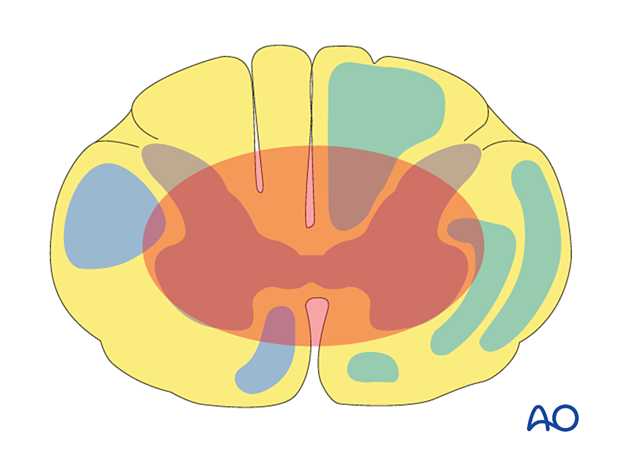
Central cord syndrome is caused by hyperextension injuries and is the most common SCI.
This syndrome is most common in elderly patients and patients with cervical stenosis.
Clinical presentation:
- There is typically more motor impairment of the upper than the lower extremities
- Bladder dysfunction
Anterior cord syndrome results from damage to the anterior 2/3 of the spinal cord. This may be caused by compromised blood supply from the anterior spinal artery or flexion compression forces on the cervical spine.
Clinical presentation:
- Patients will have minimal distal motor function because of damage to the lateral corticospinal tracts
This syndrome has the poorest prognosis for functional recovery.
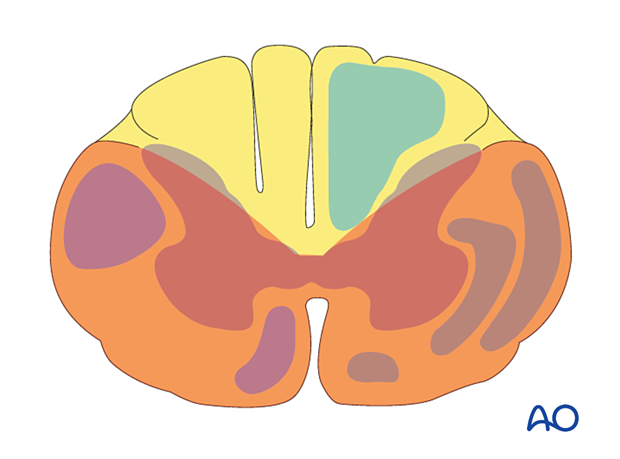
Posterior cord syndrome is a very rare injury, sparing the anterior 2/3 of the spinal cord.
Clinical presentation:
- Patients lose their ability to discern deep pressure and vibration and joint position
- Ambulation is only possible with visual feedback
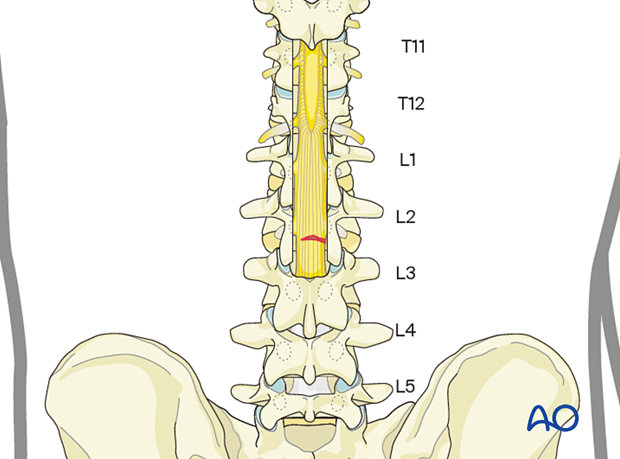
In the Conus Medullaris syndrome, there is an injury to the conus medullaris or the lumbar nerve roots. This typically occurs after fractures at the T12–L1 level.
Clinical presentation:
- Isolated bowel and bladder dysfunction
- Deficits reflecting both cord and root components
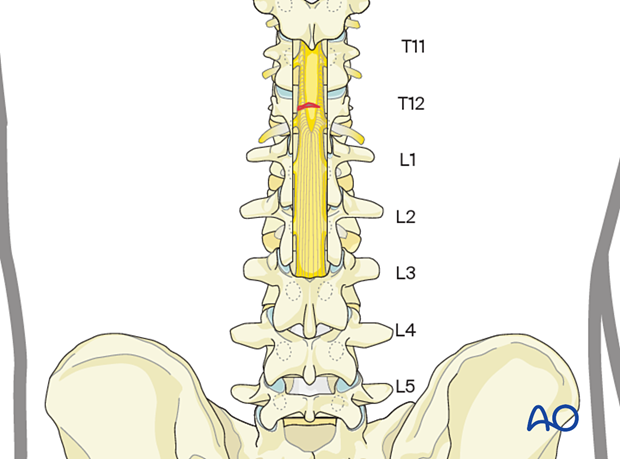
In the Cauda Equina syndrome, there is an injury to the spinal rootlets below the level of the spinal cord (typically below the L1–L2 level.
Clinical presentation:
- Bowel and bladder dysfunction
- Motor deficits
- Radicular symptoms from lower motor neuron damage