Benign tumors C1 to C7
Osteoid osteoma
Osteoid osteomas typically occur in the second decade of age with a male predominance (2–3:1). They represent 12% of all benign skeletal neoplasms, and 10% occur in the spine.
Clinical presentation
- Clinical presentation is nocturnal pain relieved by aspirin or NSAIDs.
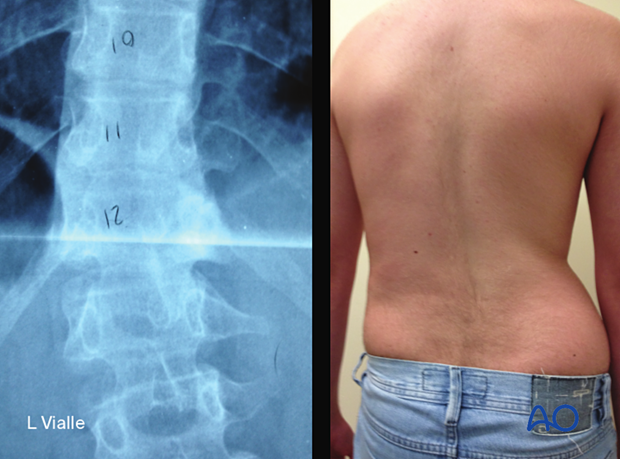
- 70% have scoliosis related to muscle spasm as shown in the x-ray and the picture (T12).
Radiology
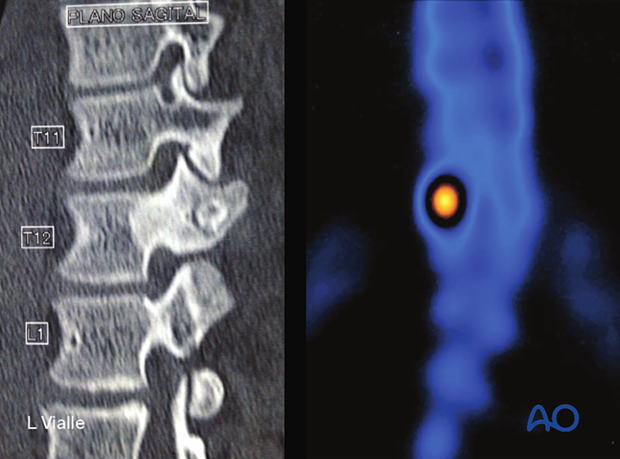
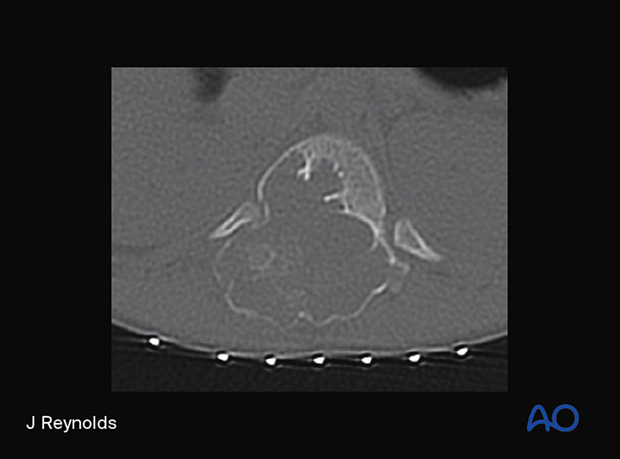
Small radiolucent tumor nidus with surrounding sclerosis typically involving the posterior neural arch (59% lumbar, 27% cervical, 12% thoracic).
CT from the patient shown above, illustrating the most common localization of osteoid osteomas (posterior arch).
Osteoid osteomas are positive on bone scan nuclear imaging as shown in the picture.
Histological characteristics
- Sharply demarcated, round, pink-red mass surrounded by sclerotic bone of osteoblastic origin.
- Osteoid osteomas are < 1.5 cm in size.
Treatment principles
Resection is curative in most cases, with an excellent prognosis. The entire nidus must be removed, or recurrence is possible. Percutaneous treatment with thermoablation is becoming more and more utilized with excellent results.
Observation can be an option for asymptomatic patients in incidental findings.
Osteoblastoma
Osteoblastomas typically occur in the same age group as osteoid osteomas.
Clinical presentation
- The most common clinical presentation of osteoblastomas is pain, which can be mechanical or nocturnal. The pain is usually less intense than pain from osteoid osteomas and is less often associated with scoliosis.
- More often associated with neural element compression.
- 40% of osteoblastomas occur in the spine.
Radiology
Well-circumscribed expansile mass occurring in the posterior elements (40% cervical, 25% lumbar, 20% thoracic, 15–20% sacrum).
Often centered in the pedicle/lamina/transverse process region and may extend into the vertebral body.
Histological characteristics
- Histologically identical to osteoid osteomas. Differentiation depends on size and behavior.
- Osteoblastomas are more than 1.5 cm in size.
Treatment principles
Surgical excision is recommended for osteoblastomas. Preoperative embolization should be considered as these are vascular tumors.
More aggressive en bloc resection should be considered for benign aggressive lesions (Enneking stage 3) to decrease the chance of local recurrence.
Giant cell tumors
Giant cell tumors typically occur in the third and fourth decade of age, with a slight female predominance for lesions involving the spinal column. They represent 5% of all primary bone tumors and typically occur in the thoracolumbar spine and sacrum.
Giant cell tumors are locally aggressive tumors with a recurrence rate of up to 50%. They may undergo sarcomatous degeneration spontaneously or following radiation treatment.

Clinical presentation
The most common clinical presentation is the insidious onset of nocturnal back pain. Pathologic fracture may be seen in upward of 30%.

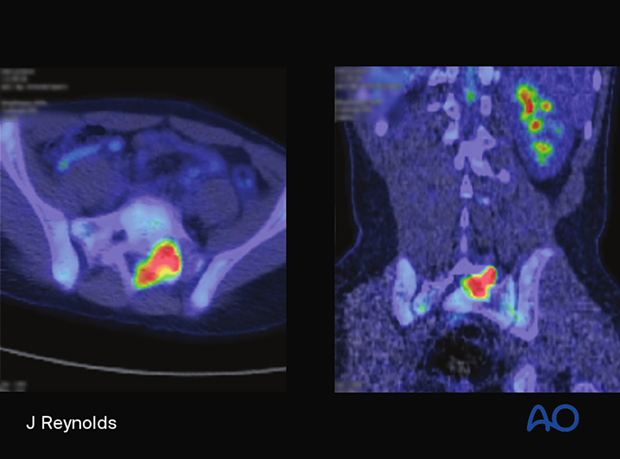
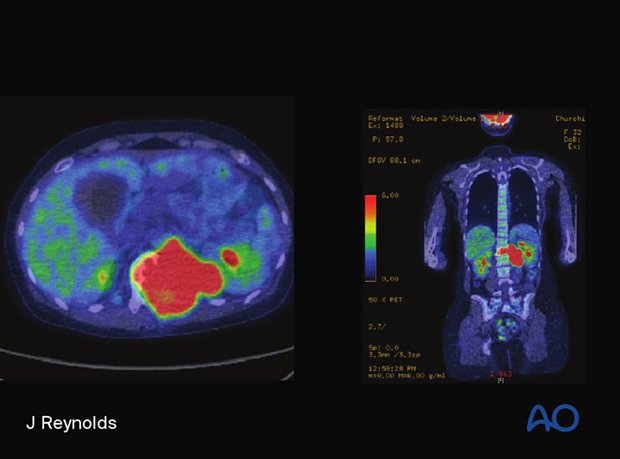
Radiology
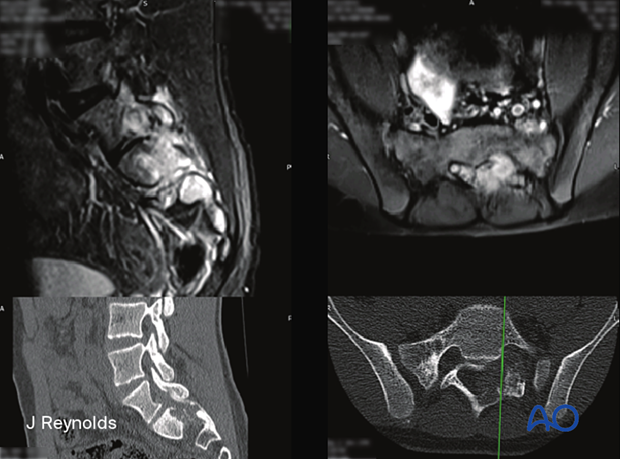
Lytic, expansile lesion of vertebral body or sacrum.
Margins are usually non-sclerotic. The bone matrix is usually absent on CT but may have residual trabeculae.
Histological characteristics
- Grossly, the tumor is tan in color and well demarcated.
- The surrounding bone is expanded with thinning of the cortex.
- Microscopically, multinucleated osteoclastic giant cells are seen among a spindle cell stroma.
Treatment principles
Complete, en bloc surgical resection is the treatment of choice when feasible and when morbidity is acceptable. Curettage or intralesional excision is associated with a high recurrence rate. Tumors may be extremely vascular, so preoperative embolization is often beneficial. Denosumab can also be used against giant cell tumors preoperatively and in nonresectable tumors.
Aneurysmal bone cyst
Aneurysmal bone cysts typically occur in the second and third decade of age with a slight female predominance. 10–30% occur in the spine. They typically arise in the neural arch, with up to 90% extending into the vertebral body.
Long-term behavior is variable, and growth may stabilize. There is a 20–30% recurrence rate and no malignant degeneration.
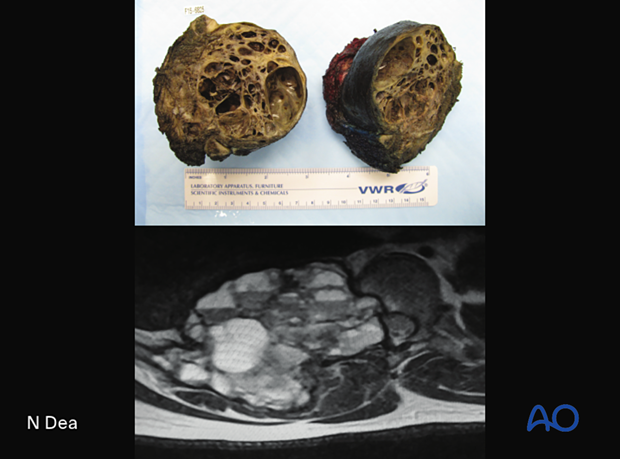
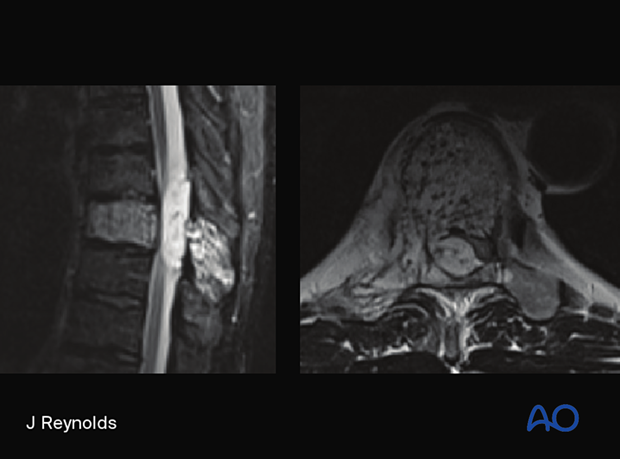
The upper picture shows a macroscopic pathology specimen of a T11 aneurysmal bone cyst depicted in the MRI picture below.
Clinical presentation
The most common symptom is severe nocturnal back pain.
Radiology
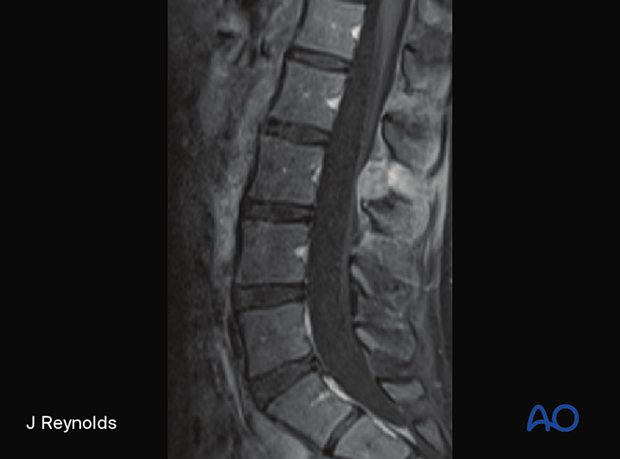
The key imaging feature is multiple fluid-fluid levels in expansile mass as shown in the MRI.
Histological characteristics
- Grossly, the tumor appears as a spongy red mass with multiple blood-filled spaces, as shown in the CT.
- Microscopically, the lesions are primarily cavernous, blood-filled cysts of variable sizes.
- Cysts are linked by fibroblasts, giant cells, histiocytes, and hemosiderin.
Treatment principles
Surgical excision may be curative. Tumors are extremely vascular and may warrant preoperative embolization. Repeated embolization may be curative in some cases.
Hemangioma
Hemangiomas typically occur in the fourth to sixth decade of age with no gender predominance. They occur in 10–20% of the adult population and are evenly distributed throughout the spinal column.
The prognosis for patient recovery is excellent.
Clinical presentation
Hemangiomas are most commonly discovered incidentally. Aggressive lesions may present with localized pain and/or myelopathy/radiculopathy from osseous expansion, epidural expansion, and/or pathological fracture.
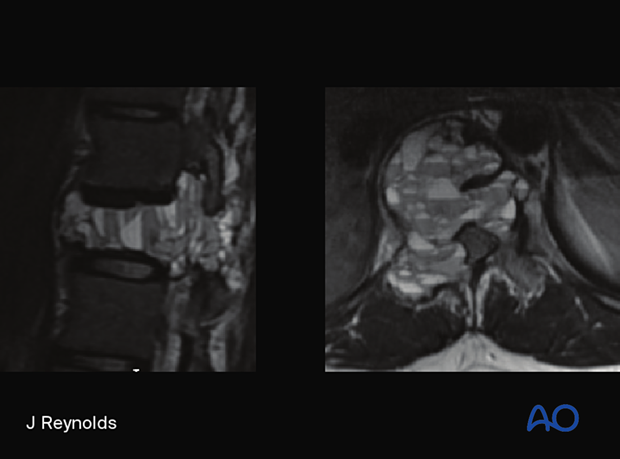
Radiology
A well-circumscribed, hypodense lesion with coarse vertical trabeculae with a white polka dot appearance on axial CT. Hyperintense on both T1 and T2 on MRI.
Histological characteristics
- Typically confined to the vertebral body.
- Microscopically, the lesion shows mature thin-walled, and cavernous sinuses dispersed among sparse, osseous trabeculae and fatty stroma.
Treatment principles
Rarely require treatment. Aggressive lesions may be treated with intralesional ethanol injection, vertebroplasty, low-dose radiation, or surgical excision.













