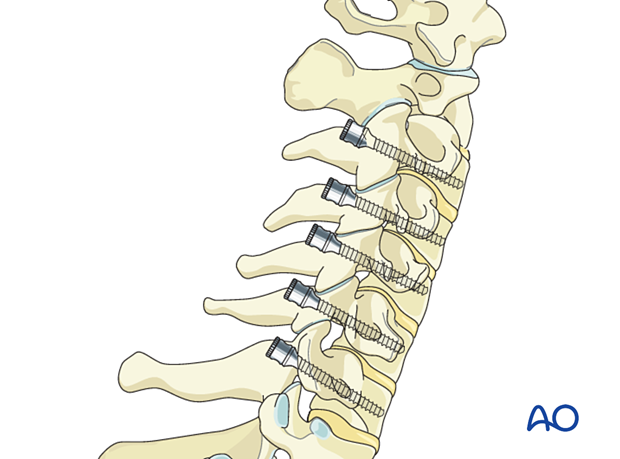
Pedicle screw insertion in the cervical spine
1. General considerations
Once the spine is exposed, the appropriate levels of fixation are confirmed with the image intensifier.
The lower cervical spine is difficult to visualize in lateral fluoroscopy. It is therefore important that good-quality AP views are available during the procedure.
Except for C7, which in 95 % of cases does not contain the vertebral artery, subaxial cervical pedicle screws are considerably riskier than lateral mass screws, and should be reserved for salvage situations in which lateral mass fixation is insufficient or unavailable.
Navigation may be used for more accurate screw insertion.
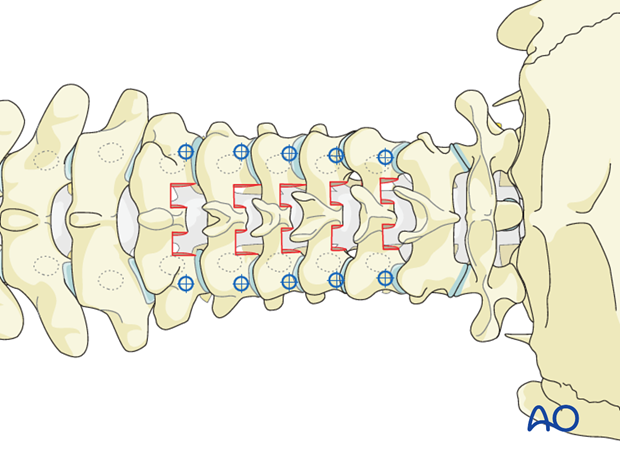
Cervical pedicle screws can be combined with lateral mass screws and thoracic pedicle screws.

2. Pitfall
Between C3 and C6, the vertebral artery lies within its foramen immediately lateral to the pedicle, and the cervical nerve root lies within the spinal canal immediately medial to the pedicle. Even minor screw malposition can therefore result in severe neurovascular injury. These concerns are compounded by the typically very narrow width of the subaxial cervical pedicles.
The average pedicle width increases from approximately 5 to 6 mm from C3 through C6.
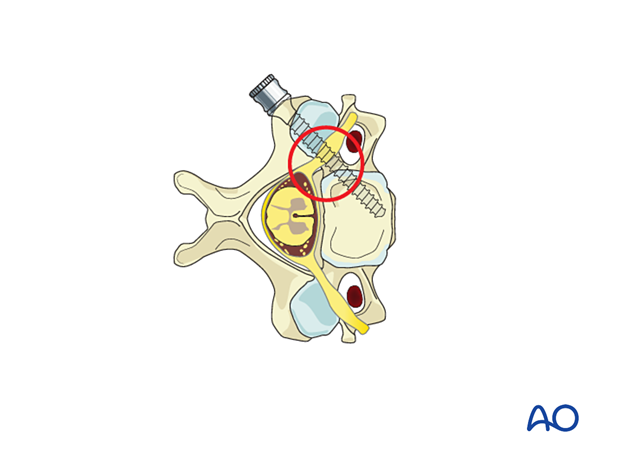
Subaxial cervical pedicles between C3 and C6 are also typically narrow in height. Screw malposition in the sagittal plane risks injury to the nerve roots within the foramina above or below the pedicle.
The average height is approximately 6 mm.
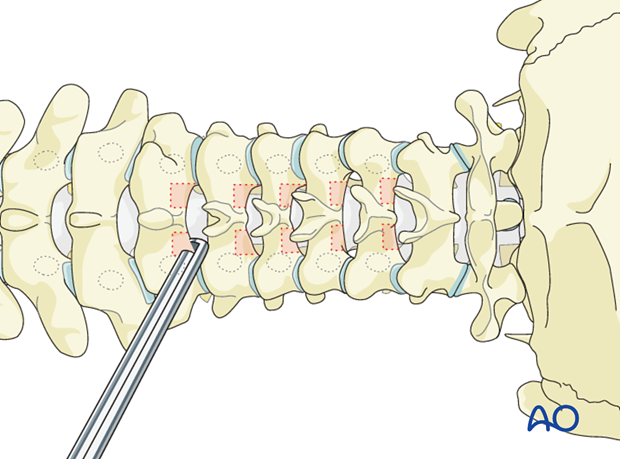
3. Laminotomy (optional)
Because of the low margin for error, we recommend that laminotomies be performed to help guide pedicle screw insertion, by allowing palpation and even direct visualization of the medial superior and inferior margins of the pedicle.
4. Entry points
The starting point is just below the facet joint at the halfway point between the medial and lateral margins of the lateral mass.
The precise location of the starting point in both the coronal and the sagittal planes can be fine-tuned by verifying the exact location of the pedicle through the laminotomy site.
5. Opening of the cortex
Open the superficial cortex of the entry point with a burr.

6. Medio-lateral inclination
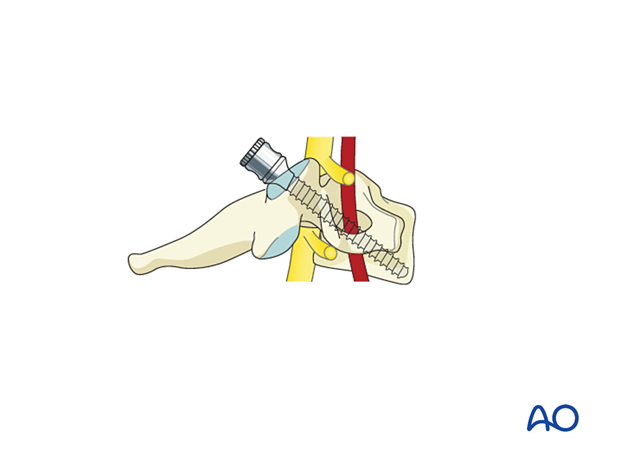
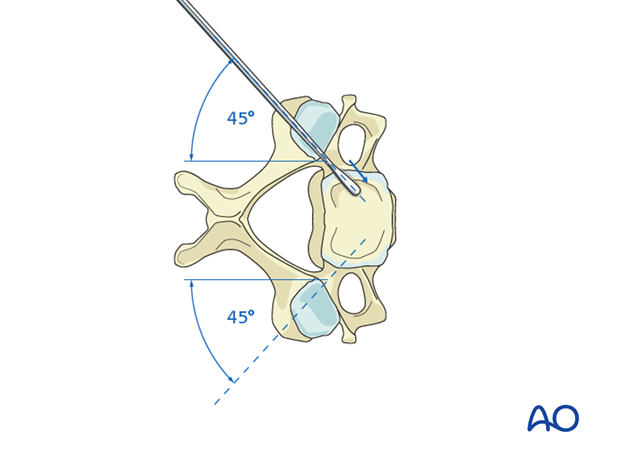
Depending on the exact location of the starting point, the angle is around 45°. Angulation decreases somewhat as you progress cranial to caudally, approaching 50° at C3 and 40° at C6. The angulation can be fine-tuned by palpation of the medial aspect of the pedicle through the laminotomy site.
7. Cranial-caudal angulation
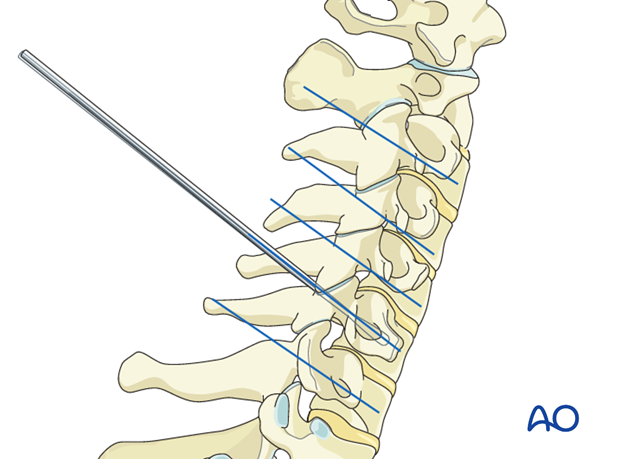
Lateral fluoroscopic guidance is recommended because of the low margin of error that results from the narrow height of C3–C6 pedicles and the close proximity of the nerve roots within the foramina above and below.
A trajectory roughly perpendicular to the axis of the posterior elements is required. This trajectory can be fine-tuned by palpating the inferior and superior margins of the pedicle through the laminotomy.
8. Screw insertion
Pedicle preparation may be performed using the small 2 mm pedicle probe or a smooth drill. Tactile feedback should be of uniform resistance from cancellous bone within the pedicle. The feeling of a premature solid endpoint may indicate excessive medial or lateral angulation and the risk of penetration through the cortex of the pedicle.
However, because the C3 to C6 pedicles are often sclerotic, tactile feedback can be unreliable, which further highlights the usefulness of guiding screw insertion through a laminotomy.

Screw diameter is determined based on preoperative CT measurements of the height and width of the pedicles. Screws of 3.5 or 4.0 mm in diameter are typically used.
Screw length can be determined by preoperative CT measurement and by intraoperative measurement of the length of the screw tract.
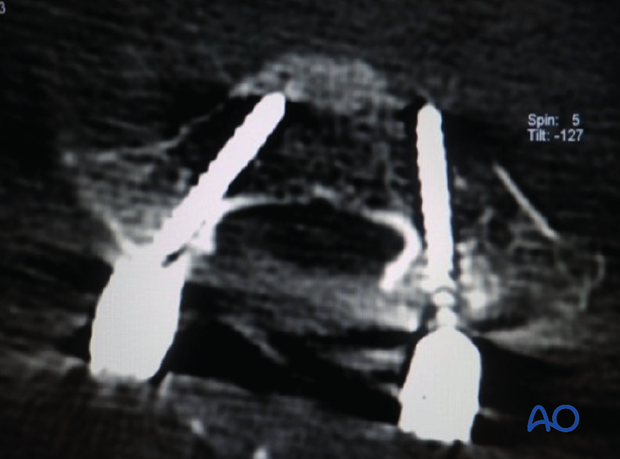
The screw is inserted through the created trajectory.