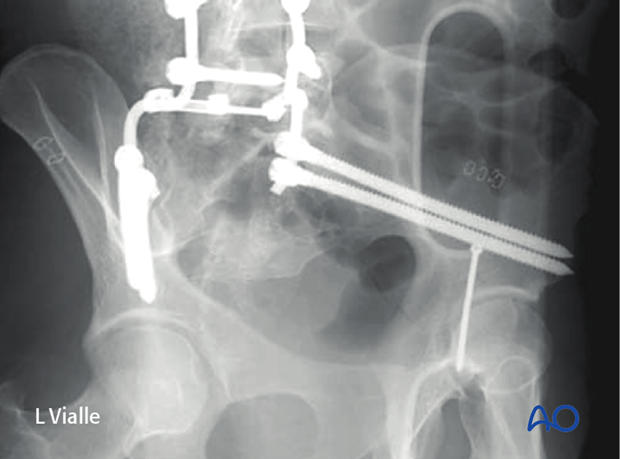
Iliac screw insertion
1. Screw entry points
There are two standard iliac screw entry points within the ilium and one within the sacrum.

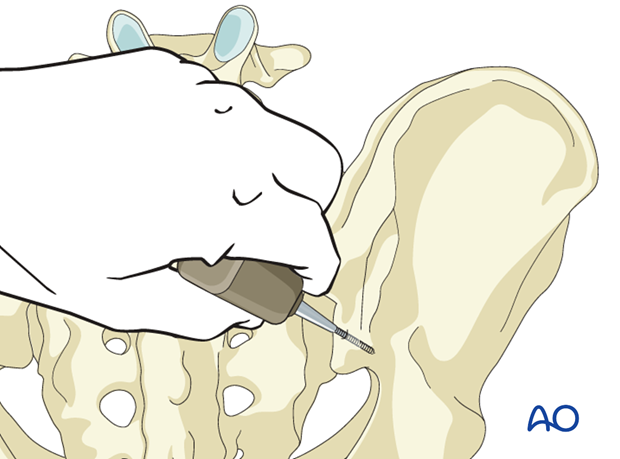
2. Traditional entry point
The traditional entry point is in the posterior iliac crest. It is countersunk to prevent pressure ulcers over the implant.
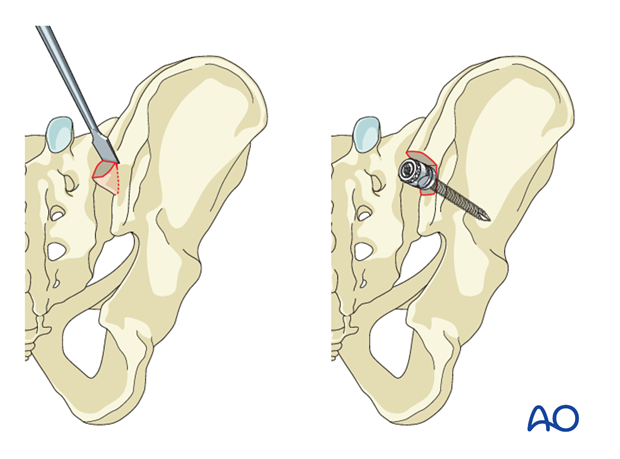
An oscillating drill (3.5 mm) or an awl is used to penetrate between the two cortices in a ventral, caudal direction toward the anterior inferior iliac spine.
When resistance is felt, the length is measured for the insertion of the pedicle screw.
The preferred diameter is 7.0 or 8.0 mm.
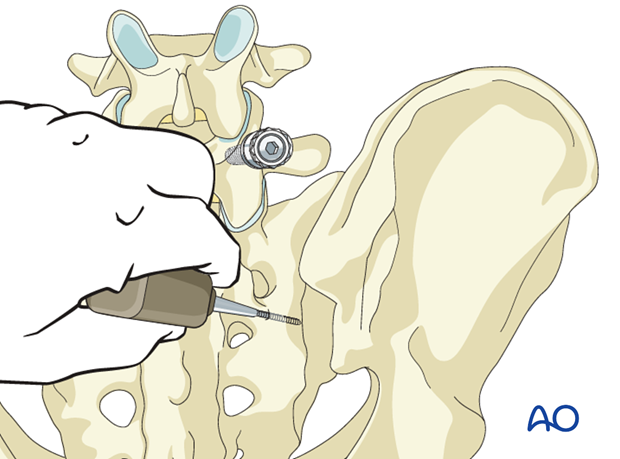
3. Anatomic entry point
The second iliac entry point is referred to as the anatomic entry point. It is more caudal and medial than the traditional entry point and aligns better with the lumbar pedicles.
The more caudal position places this screw in a wider cross-section of bone above the sciatic notch.
An oscillating drill (3.5 mm) or an awl is used to penetrate between the two cortices in a ventral, caudal direction toward the anterior inferior iliac spine.
When resistance is felt, the length is measured for the insertion of the pedicle screw.
The preferred diameter is 7.0 or 8.0 mm.
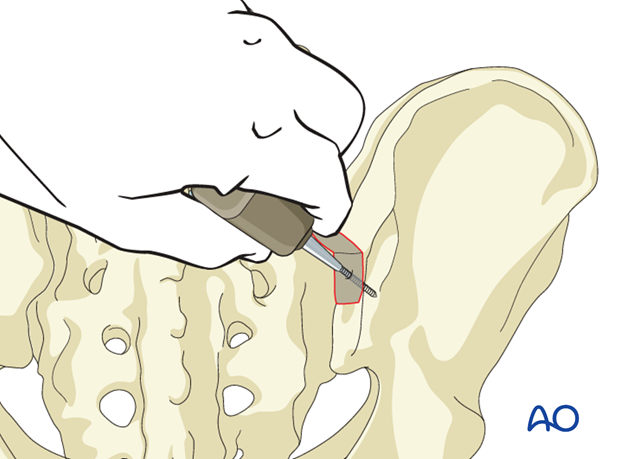
4. Sacral entry point
The third entry point is at the inferolateral aspect of the S1 foramen.
An oscillating drill (3.5 mm) or an awl is used to cross the sacroiliac joint and penetrate between the two cortices of the ilium in a ventral, caudal direction towards the anterior inferior iliac spine.
When resistance is felt, the length is measured for the insertion of the pedicle screw.
The preferred diameter is 7.0 or 8.0 mm.
Because a more lateral trajectory is required, the screws placed using this technique tend to be shorter than those with an iliac entry point.
As the entry point is deeper, there is less concern with screw prominence compared to iliac entry points.
Because the screw crosses the sacroiliac joint, there is potential for long-term consequences such as arthrosis and pain.
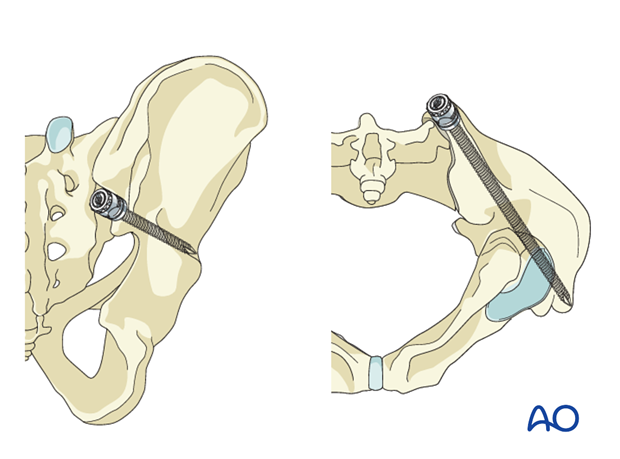
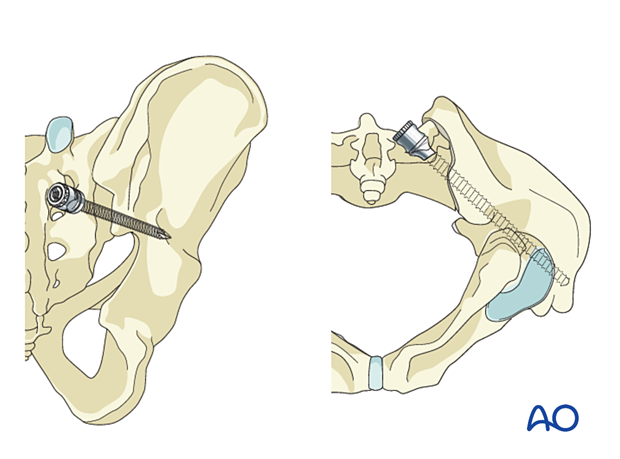
5. Screw trajectory and imaging
The true lateral view (with sciatic notches superimposed) is the primary view for screw insertion.
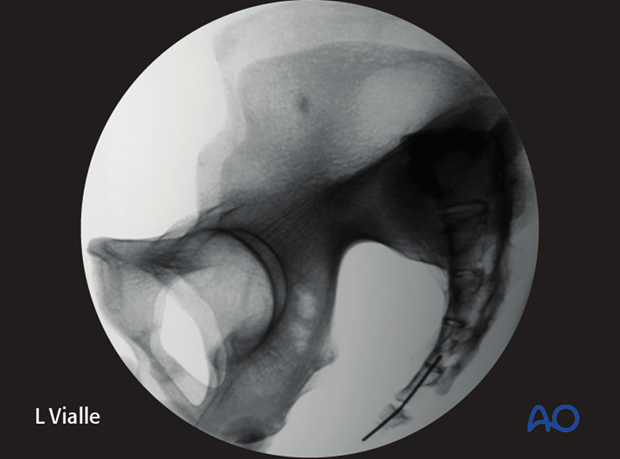
Screw trajectory should extend within 2 cm above the sciatic notch, above the acetabulum, and towards the anterior inferior iliac spine.

The obturator outlet (teardrop) view provides a cross-sectional view of the teardrop-shaped bony channel above the sciatic notch within which the screw should be positioned.
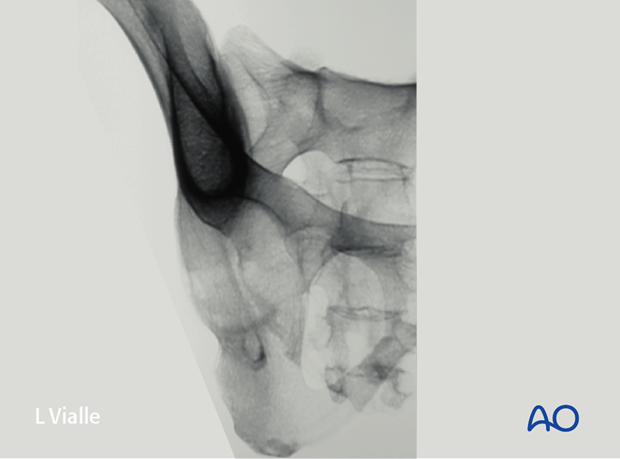
The screw should be confined to the bony margins of the teardrop on the obturator outlet view.

6. Additional views
Obturator inlet view
This view is perpendicular to the screw trajectory. The screw should remain within the inner and outer margins of the ilium.
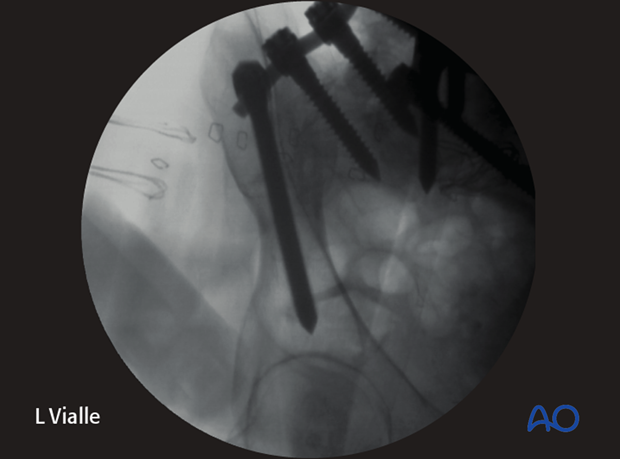
Iliac oblique view
This view is perpendicular to the ilium and can be used to verify screw position above the sciatic notch and acetabula, and acceptable screw length.