Posterior access to the cervical spine (C3–C7)
1. General considerations
The exposure for resection of primary tumors may be wider than in a trauma approach. Moreover, more lateral extension may be required. In the case of previous intralesional surgery, wound excision is advised to remove the scar as it may have been contaminated by the tumor during the first surgery. Lastly, some patients will need preoperative radiation therapy as part of their treatment plan, which could render the approach more difficult and more prone to postoperative complications. Meticulous surgical technique in the exposure and closure is warranted.
2. Skin incision
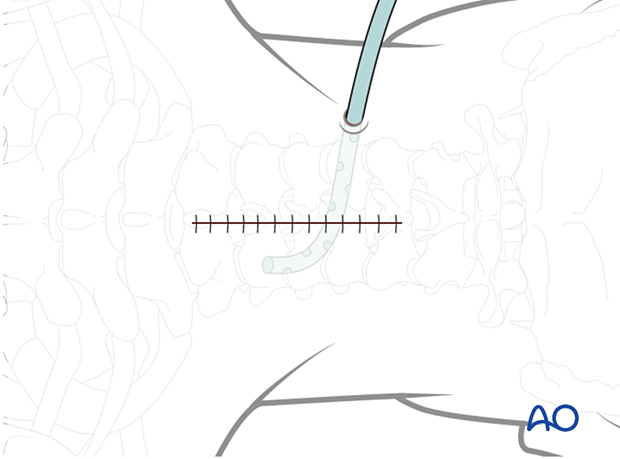
The skin and subcutaneous tissue may be infiltrated with a 1:500,000 epinephrine solution to achieve hemostasis.
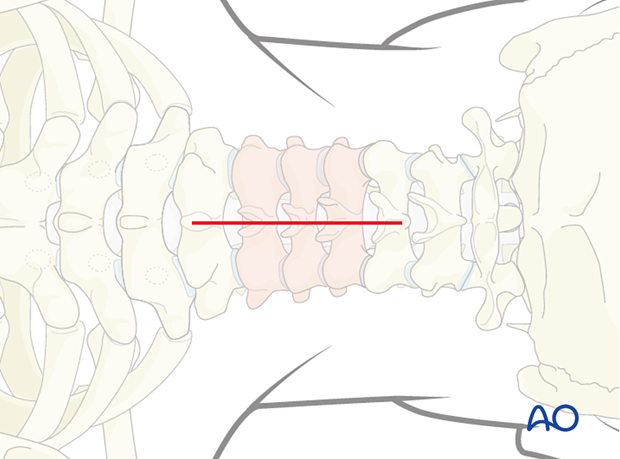
The exact location of the incision is identified using a C-arm and marked.
A midline skin incision is made centered over the involved segment.
3. Dissection
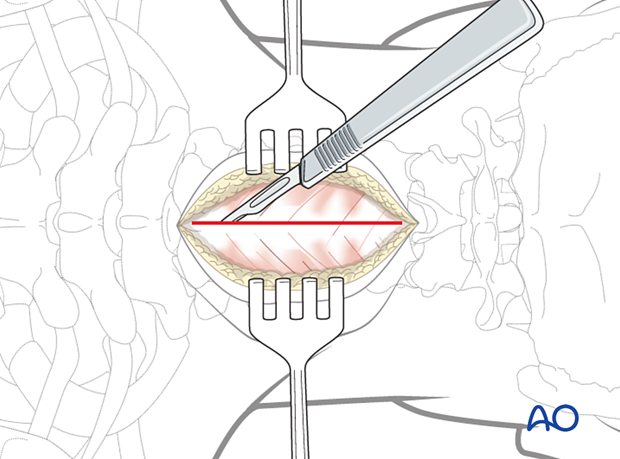
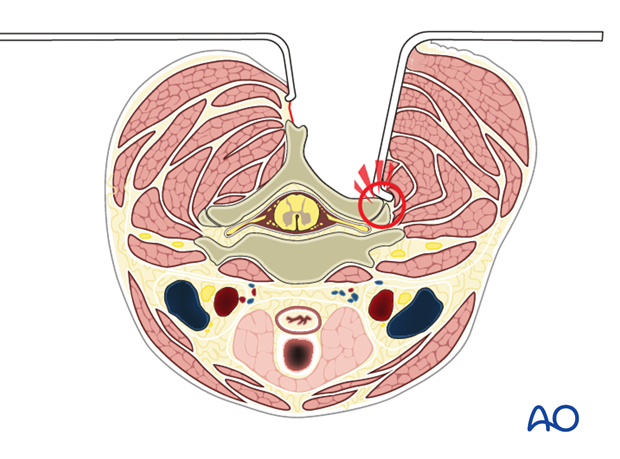
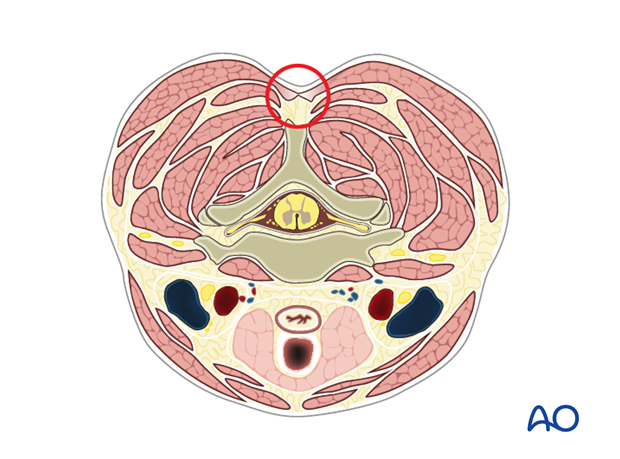
The dissection is carried down in the midline through the subcutaneous tissue and the fascia to the tips of the spinous processes.
The dissection should be carried down through the midline to decrease bleeding.
It is necessary to confirm the vertebral level with fluoroscopy as soon as bony structures are visible. This is done prior to any further dissection.
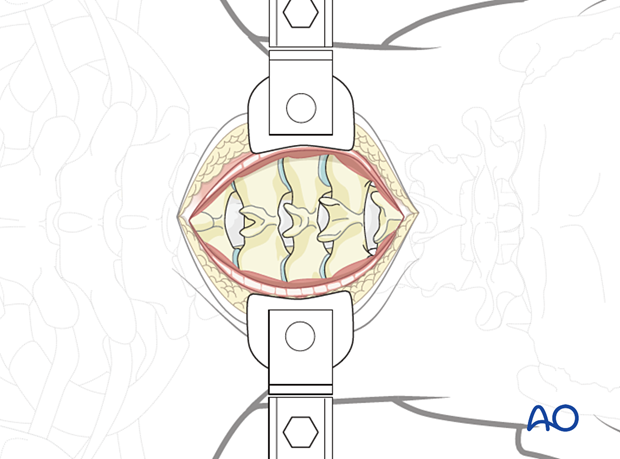
Self-retaining retractors are used to maintain tension on soft tissues during exposure.
The paraspinal muscles are elevated subperiosteally from the underlying laminae, using a Cobb elevator. Dissection is performed along the spinous processes, lamina, and lateral mass (bilaterally).
Review preoperative images to verify whether the tumor invades the lamina. In such cases, exposure of the posterior elements should be performed with great care, and the use of Cobb elevators should be avoided.
When operating on a primary tumor that involves the posterior element, great care should be taken not to enter the tumor during exposure.
The use of a subperiosteal dissection minimizes bleeding and muscle damage.
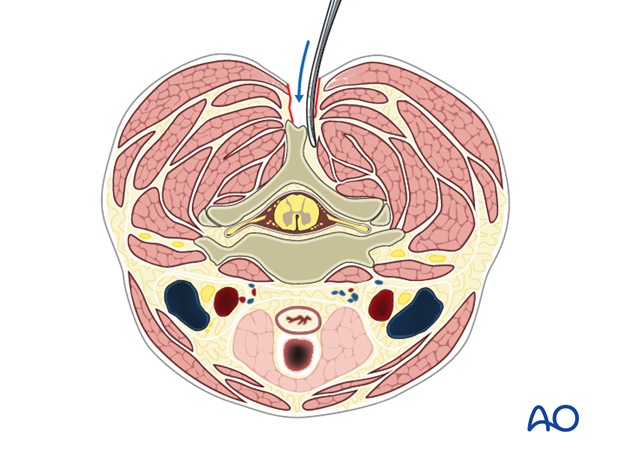
During exposure, care is taken not to injure the facet joint capsule the proximal or distal joints, as this might lead to unintended joint fusion or degeneration.
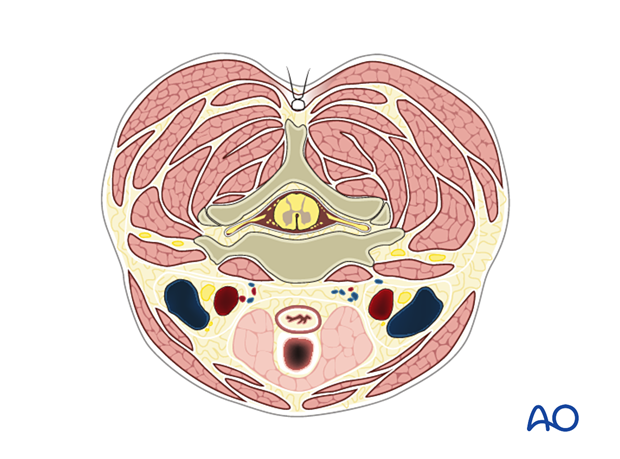
Final exposure of the posterior cervical spine from C3 to C7
4. Closure
For patients undergoing tumor surgery and/or with history of radiation, plastic surgery should perform the soft tissue reconstruction to decrease the risk of wound complications.
Drains are usually inserted via a separate stab incision.
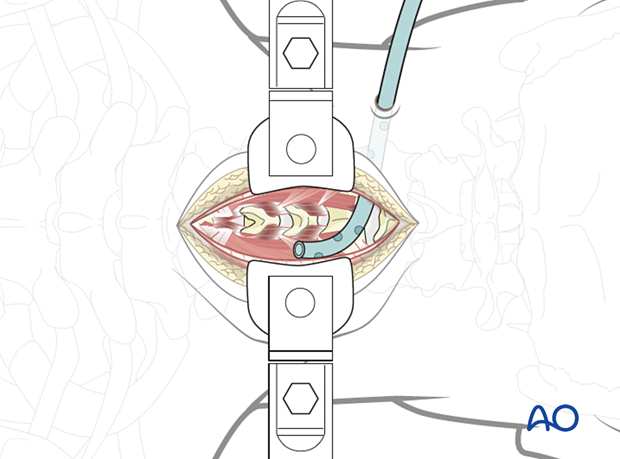
Once the surgical fixation and decompression have been performed, the muscles are approximated using interrupted sutures.
The fascial layer is then closed with continuous or interrupted sutures.
Intrawound vancomycin can be applied to decrease the risk of postoperative wound complications.
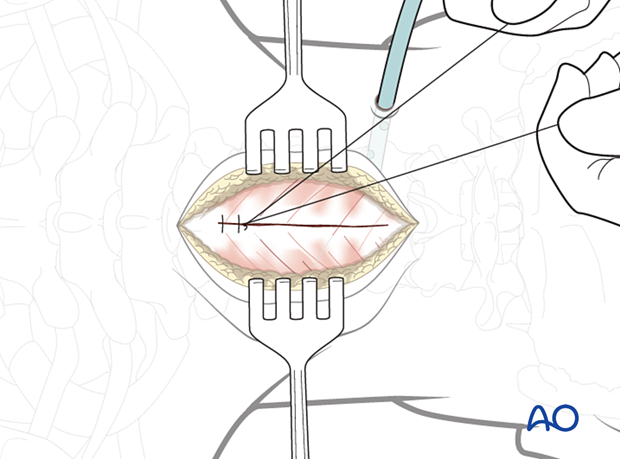
The subcutaneous layers and skin are sutured.