Anterior access to the cervical spine (C3–C7)
1. Incision
The exposure for resection of primary tumors may be wider than in a trauma approach.
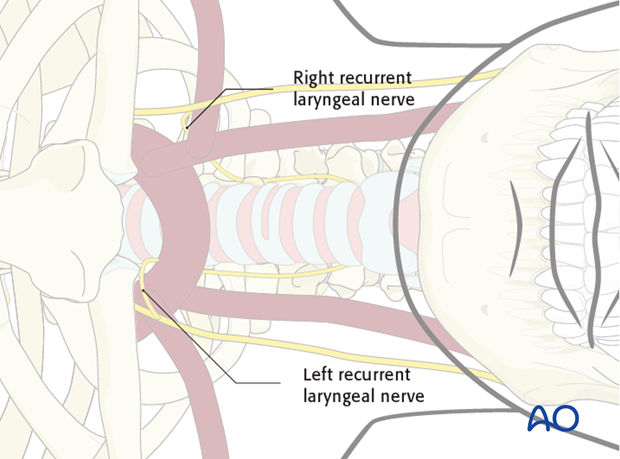
The side of the incision, left or right, mainly depends on the surgeon’s preference.
By using a left-sided approach, the recurrent laryngeal nerve can be avoided.
By using a right-sided approach, the same nerve can be visualized and protected.
For patients undergoing revision surgery and/or with history of radiation, a head and neck surgeon can help reduce the risk of approach-related complications.
Furthermore, the assistance of a head and neck surgeon is necessary if the exposure needs to be extended superiorly (C2).
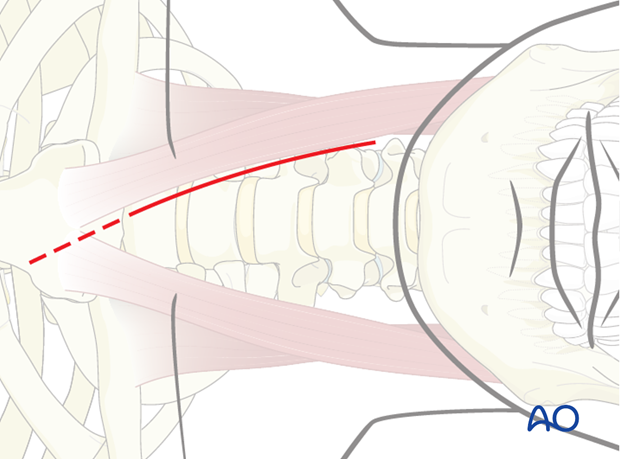
The transverse incision is made at the level required. A transverse incision will give a better cosmetic outcome; however, only limited exposure.
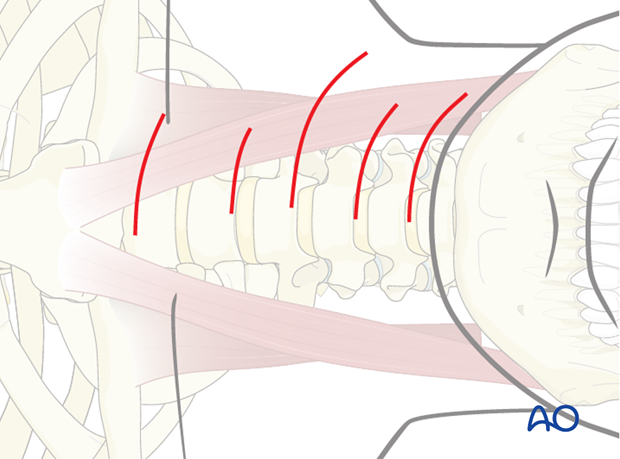
If a multilevel fixation is considered, a more longitudinal incision is required.
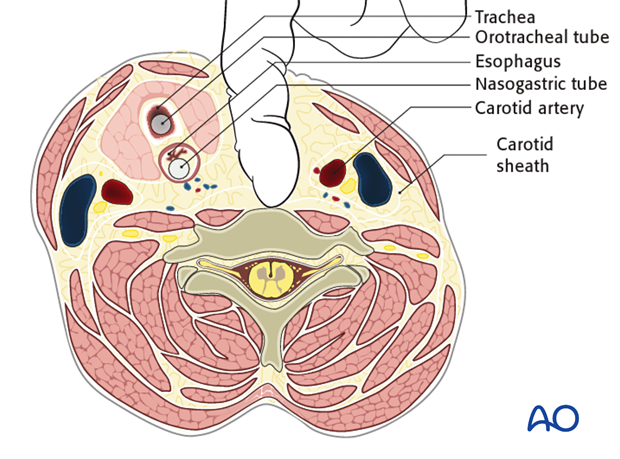
Injuries of the esophagus can occur as a complication of the approach.
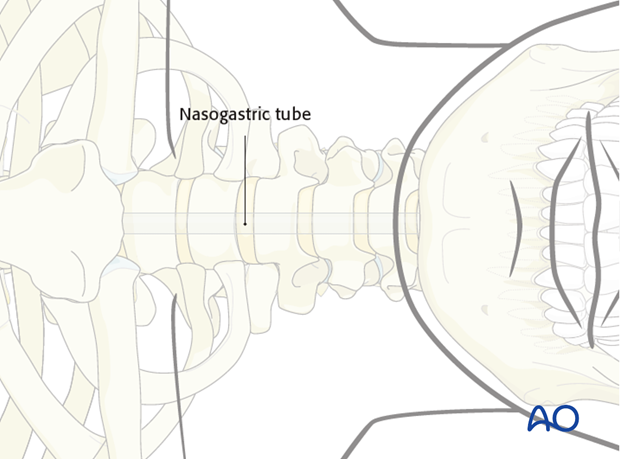
In addition to the tracheotube, a nasogastric tube should be inserted to identify better and thus help prevent accidental injury to the esophagus.
These are serious and potentially lethal complications. Consultation with thoracic or ENT surgeons should be obtained.
2. Dissection
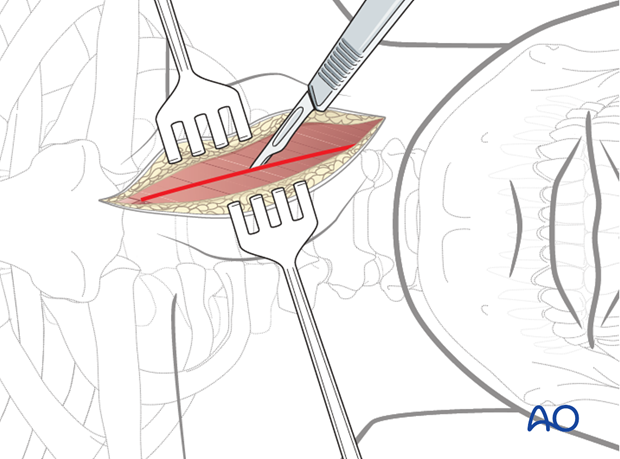
The platysma muscle is transected in line with the skin incision.
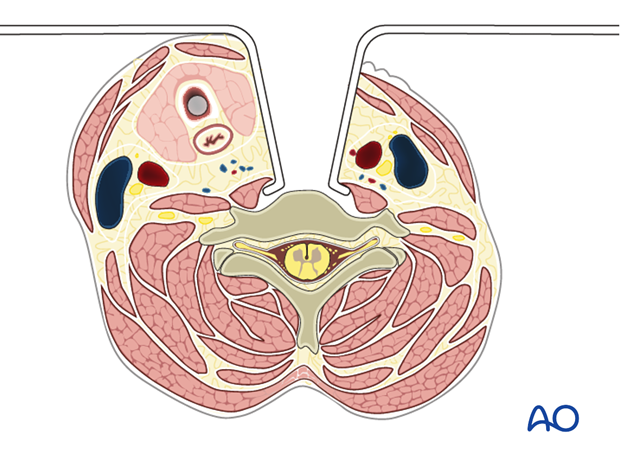
The deep cervical fascia is identified and divided along the anteromedial border of the sternocleidomastoid muscle.
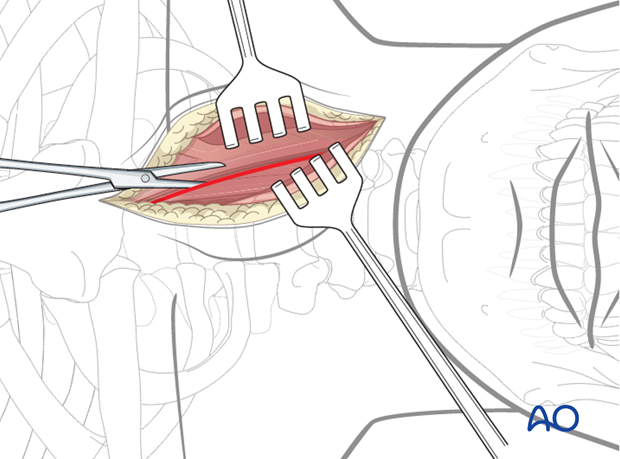
The carotid pulse is palpated, and the dissection is directed medial to the carotid sheath.
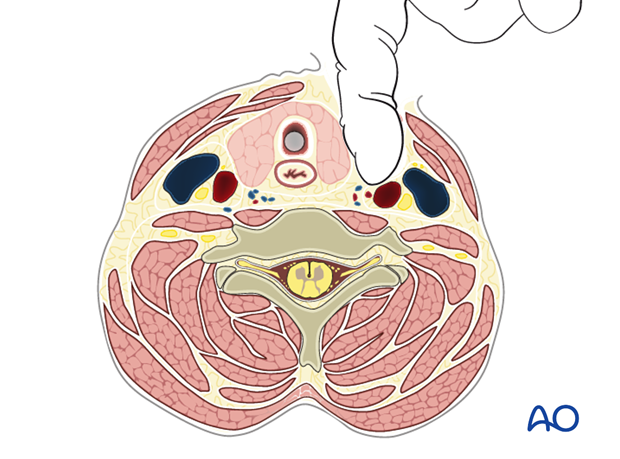
A finger is then used for blunt dissection between the carotid sheath laterally and the trachea and esophagus medially, down to the prevertebral fascia.
The recurrent laryngeal nerve is identified and protected.
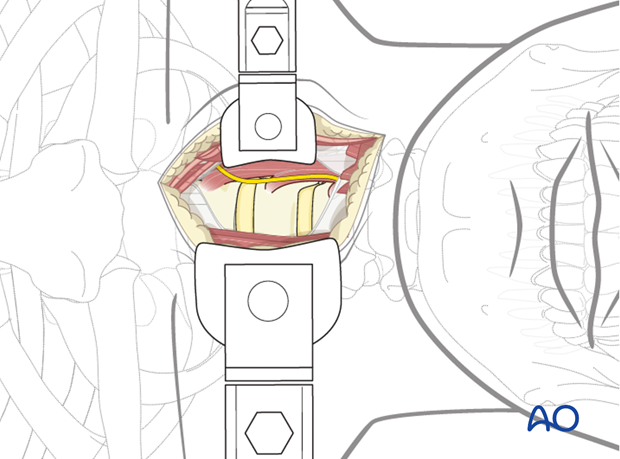
The prevertebral fascia is cut longitudinally, allowing direct visualization of the vertebra and the longus colli muscle.
The level is verified with fluoroscopy. The longus colli muscle is mobilized, and retractors are placed.
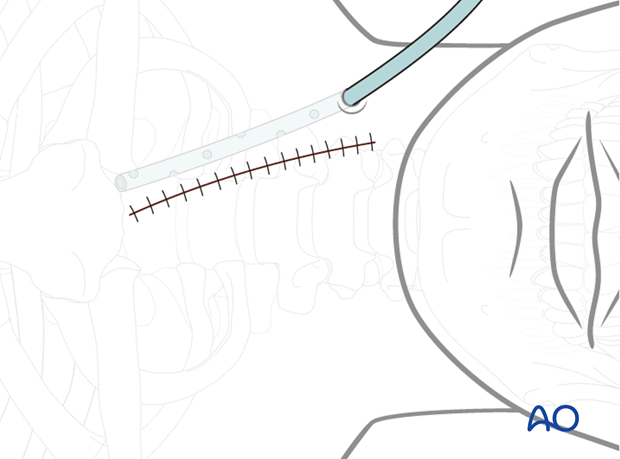
3. Closure
The platysma muscle is sutured, followed by subcutaneous and skin closure.
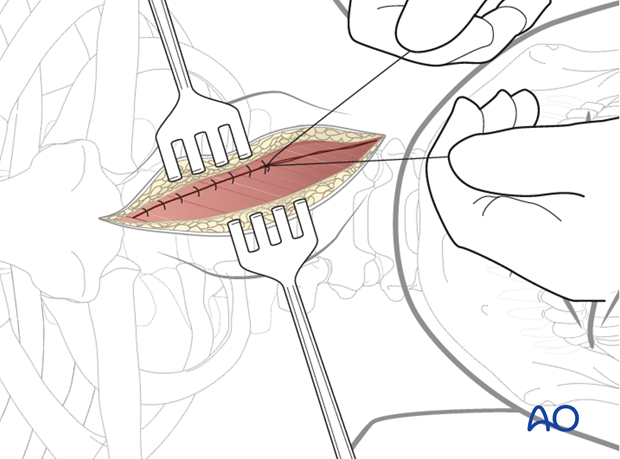
A wound drain is inserted through a separate stab incision.