Nonoperative treatment/ bracing
1. Preliminary remarks
A fracture that is deemed to be stable may be treated with brace immobilization or no brace immobilization.
Early mobilization is instituted once a patient is upright.
The purpose of a brace is to prevent ranges of motion outside of limits deemed unfavorable for fracture healing.
A brace is also commonly used following surgical stabilization to temper patient activity.
Bracing is often unsuccessful for ligamentous disruption in the adult patient.
AP lateral plain x-rays are obtained to make sure there is no significant fracture displacement requiring surgery.
2. Bracing
Bracing is often performed immediately after the injury up to 10 to 12 weeks. At the present time there is controversy regarding the effectiveness of bracing for spinal injuries in providing better outcomes at follow-up.
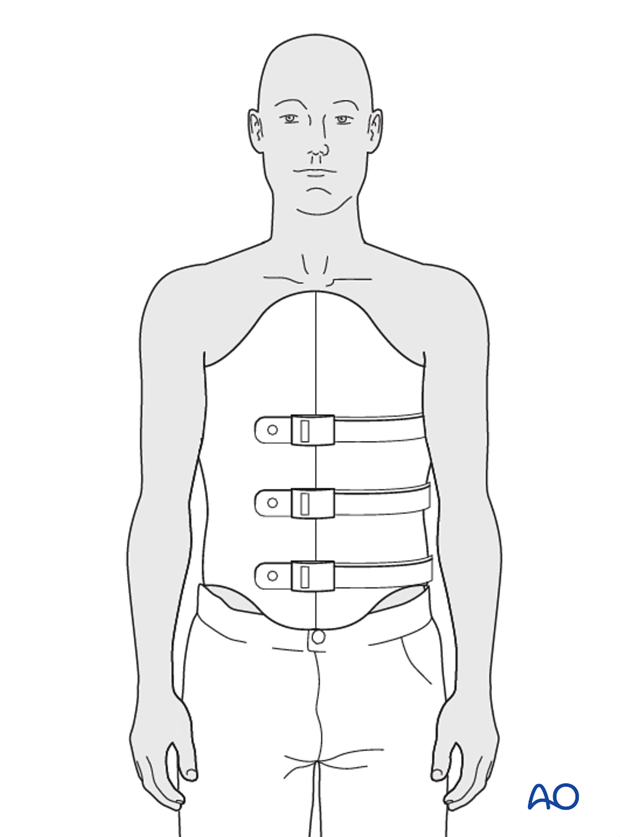
Thoracolumbar sacral orthosis (TLSO)
Traditional thoracolumbar sacral bracing is used for fractures between T8 and L4.
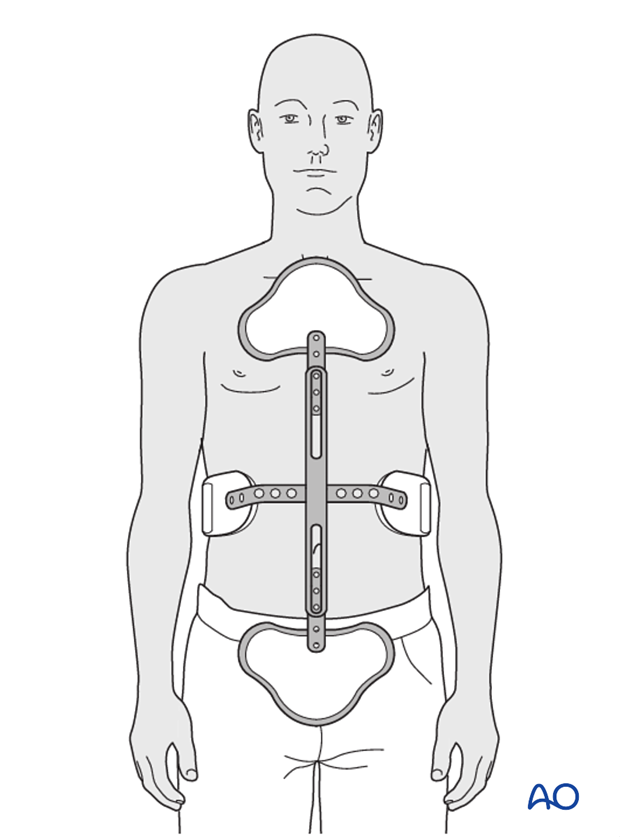
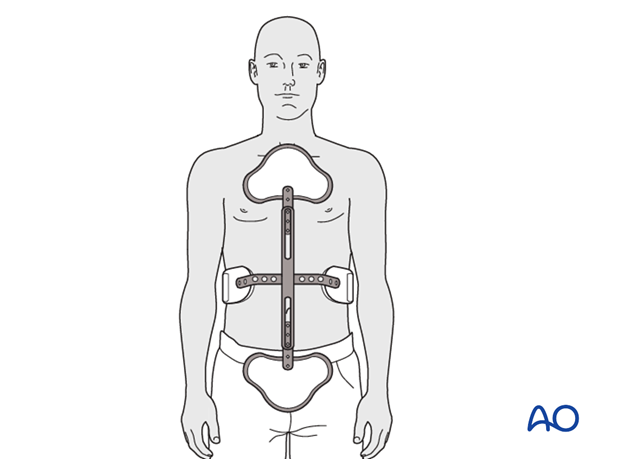
TLSO hyperextension brace (Jewett)
Many feel a hyperextension brace or a 3 point loading orthosis is biomechanically optimal to prevent fracture collapse or increasing kyphosis. (Thoracolumbar junction T10-L2)
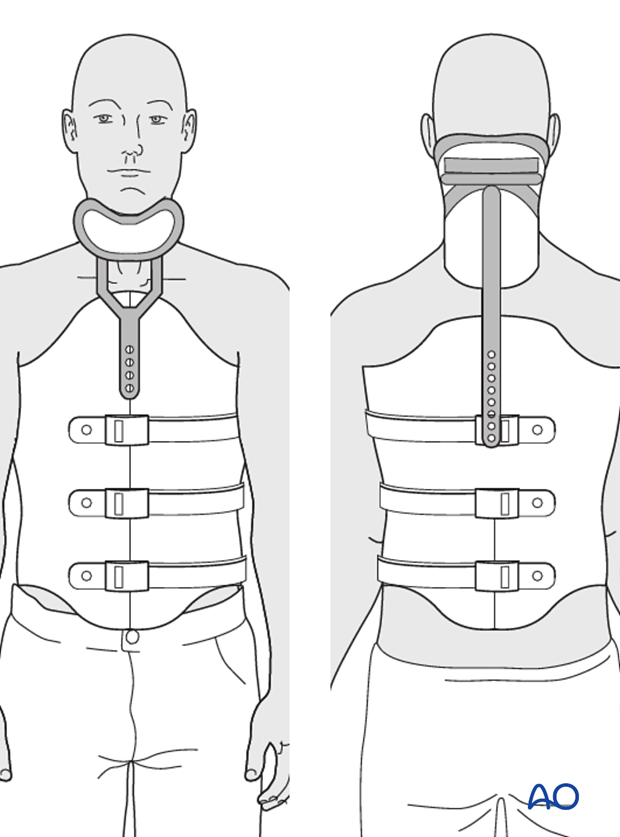
TLSO with cervical extension
Fractures of the thoracic spine from T1 and T7 require a cervical extension to the brace.
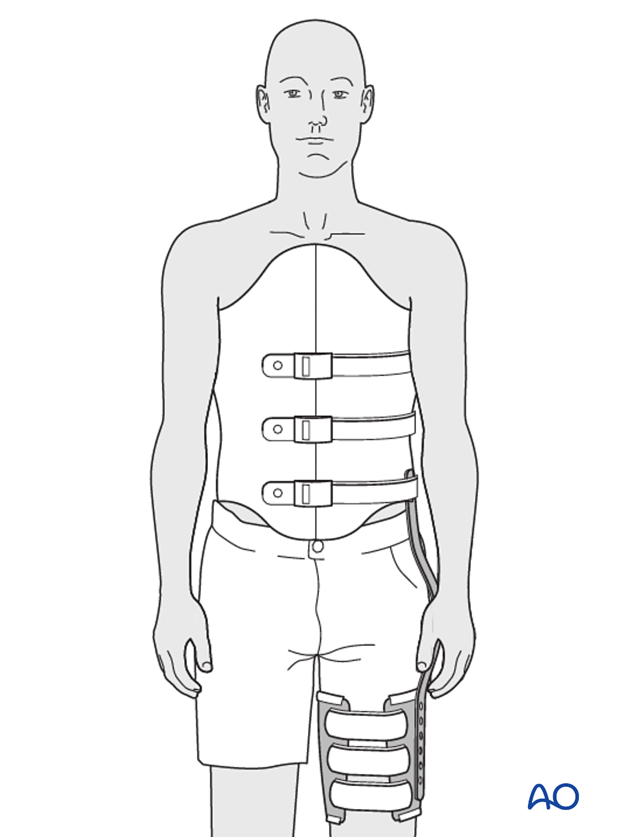
TLSO with leg extension
Fractures involving L5 and the first sacral vertebral body often require a leg extension to the brace.
3. Aftercare for nonoperative procedures
Bracewear is considered an inconvenience for patients. In a strict sense, it should be worn 24 h a day to provide adequate immobilization.
For personal hygiene, the patient can stand with the help of a carer/assistant, who helps remove the brace without any bodily movement. The patient can then shower and dry themselves, with the carer then assisting with the reapplication of the brace.
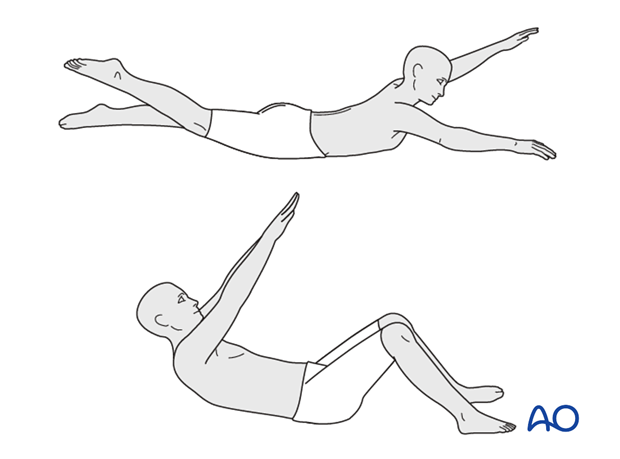
An intensive physical rehabilitation program needs to be established after removing the brace, especially for strengthening the abdominal muscles and the posterior vertebral muscles.