Fractures in the ankylosed cervical spine
1. Introduction
Fractures in ankylosed spines occur primarily in patients with:
- Ankylosis spondylitis
- Seronegative spondyloarthropathy
- Diffuse idiopathic spinal hyperostosis (DISH)
- Previous surgical fusion
Because the spine is rigid, fractures do not follow the usual patterns of injury in non-ankylosed spines. Instead they tend to mimic long bone fractures of the extremities and treatment philosophy should be adjusted accordingly.
The fractures have several characteristics that are important to recognize:
- Highly unstable three column injuries regardless of the degree of displacement
- Frequently caused by low energy injuries
- Difficult to diagnose
- Compromised bone quality
- Patients with many comorbidities
- 10 % association with epidural hematoma
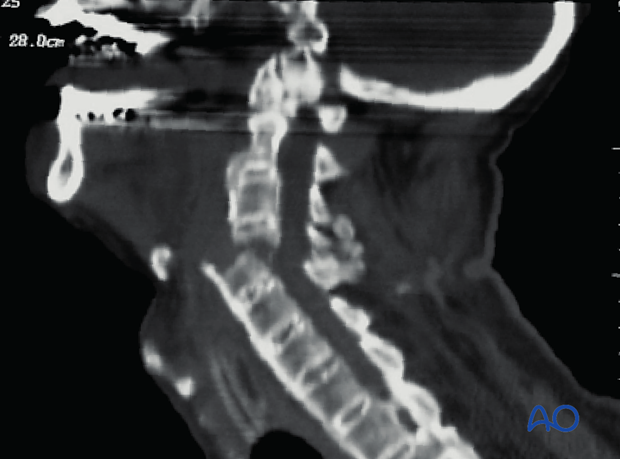
Diagnosis
Because of the combination of poor bone quality, often trivial causative injuries and the fact that even minimally displaced injuries can be very unstable, timely diagnosis of these injuries can be challenging.
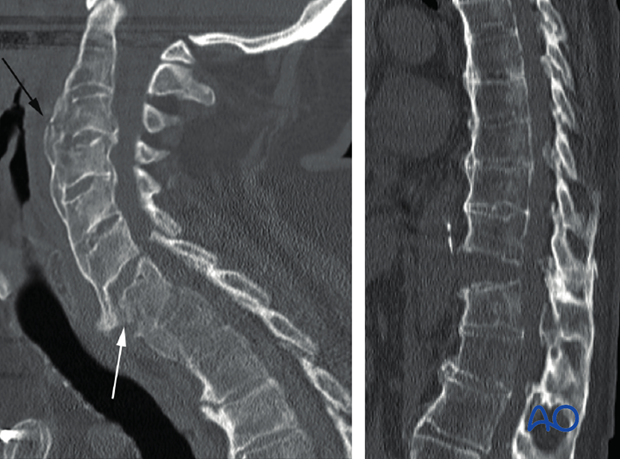
Multiple noncontiguous injuries occur in 10 % of patients.
Patients with ankylosing spine conditions who have new onset of neck pain require CT imaging to evaluate for fracture. If a fracture is identified, the remainder of the spine should also be imaged with CT or MRI to identify noncontiguous injuries.
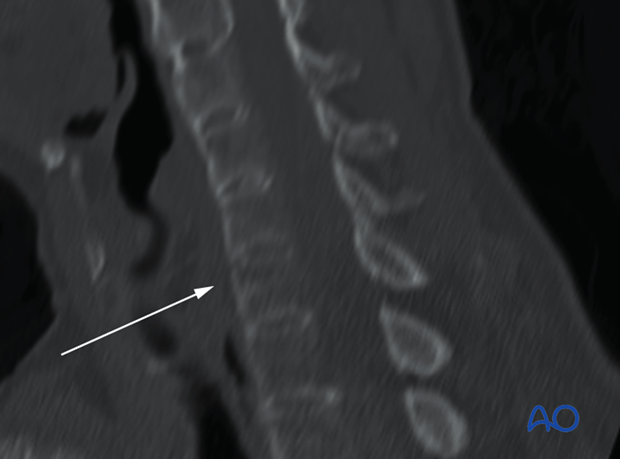
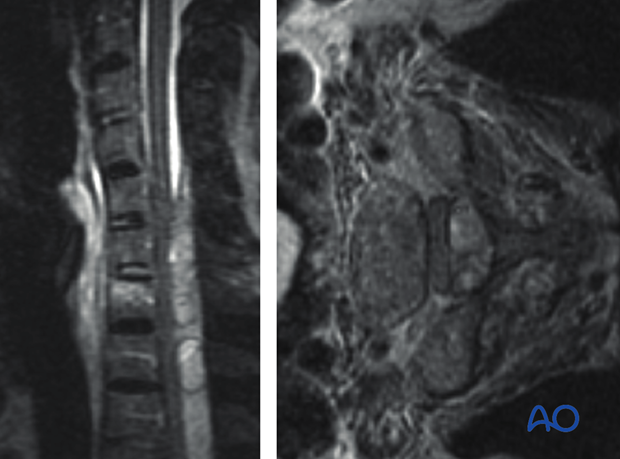
Patients who have neurological deficits without obvious radiographic reasons should be evaluated emergently with MRI to look for epidural hematoma which occurs in approximately 10 % of patients.
MRI can also be useful to detect non-displaced fractures when CT findings are equivocal.
MRI scanning may not be feasible in patients with severe kyphotic deformities.
Treatment
Because the spine is ankylosed the number of levels instrumented has no implications on spinal motion segments and refers only to the number of fixation points. This is analogous to the fixation of long bone fractures, the principles of which mandate multilevel posterior fixation for fractures in the ankylosed spine.
In general three fixation points above and below the fracture are recommended though a minimum of two may suffice (as shown).
For this reason short segment fixation should be avoided as it is biomechanically unfavorable and provides no benefit in terms of preserving spine motion.
For similar reasons and because the osteoporosis frequently seen in these patients preferentially affects the anterior column, anterior fixation should be avoided as a definitive form of stabilization.

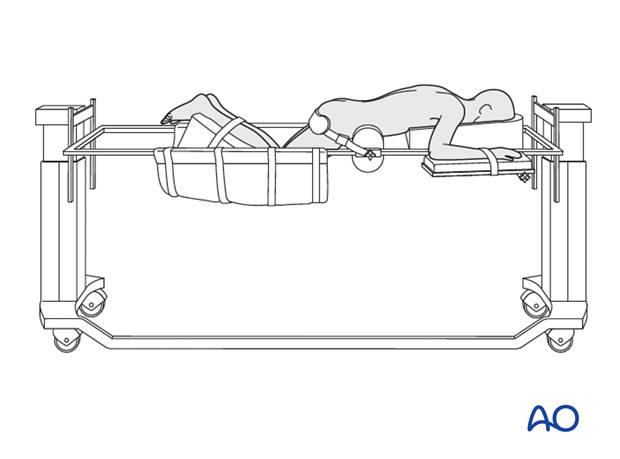
Positioning
Due to the highly unstable nature of these injuries, patients are at risk for neurological deterioration when being intubated and positioned prone.
Awake fiberoptic intubation should be performed.
This risks associated with positioning can be minimized as follows:
- Awake positioning
- Wake up test
- Electrodiagnostic monitoring pre- and post-positioning
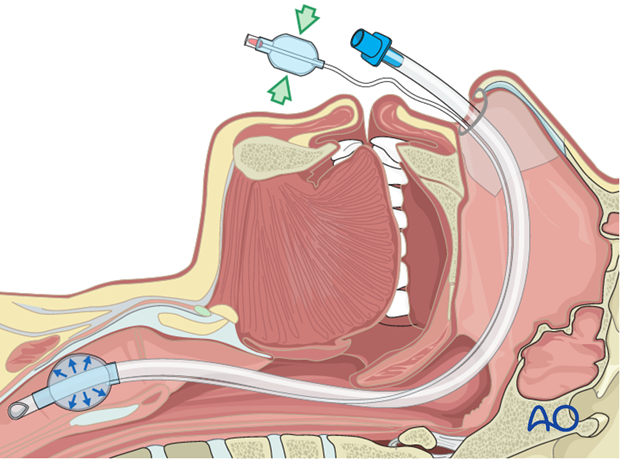
Measures should be taken to avoid hyperextension of the injury during positioning.
Rigid fixation of the skull with Mayfield clamps or a comparable device is required.
Because these patients frequently have severe cervicothoracic kyphosis, positioning can be a challenge. If using Jackson frame, the chest pad frequently needs to be bolstered to elevate the neck above the rails of the frame.
Radiographic visualization of the cervicothoracic junction can be challenging or impossible due to osteoporosis, deformity, and body habitus.