Cervical spine - posterior fixation
1. Introduction
Posterior instrumentation is either combined with open reduction, or is performed after closed reduction has been successfully achieved.
MRI should be obtained preoperatively to rule out the presence of a significant disk herniation before attempting open reduction through a posterior approach.
In certain situations involving the presence of severe neurological compromise after a failed attempt at closed reduction, an open reduction can be performed even without MRI if early reduction is a priority.
Direct decompression of spinal canal caused by a vertebral body fracture intruding into the canal anteriorly cannot be addressed with a posterior approach.
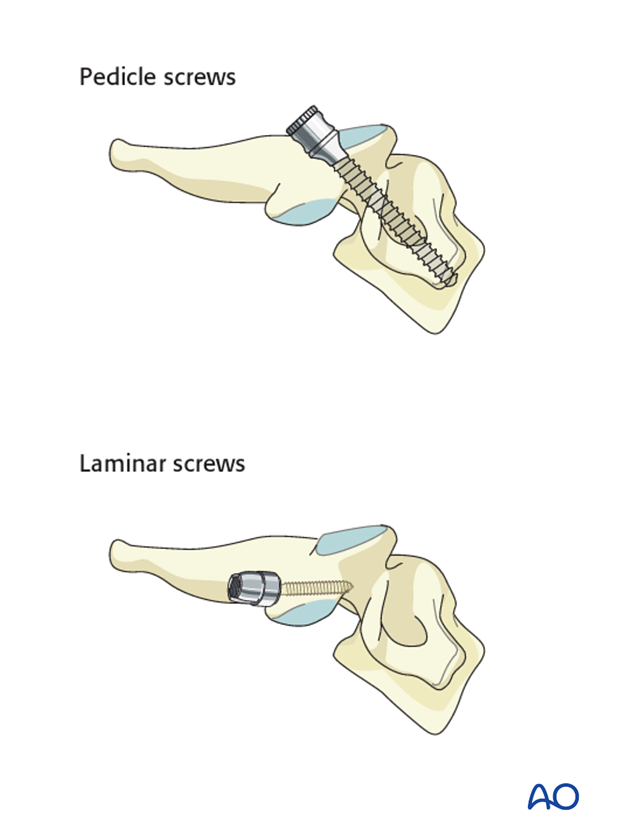
Lateral mass screws vs. pedicle screws
Fixation can be achieved with either lateral mass screws, pedicle screws or combination of the two.
Because lateral mass fixation is generally sufficient, and carries less risk, pedicle screw fixation is limited to rare cases where lateral mass fixation would be insufficient or not possible.
Surgical complications
More details on surgical complications can be found here.
2. Positioning and approach
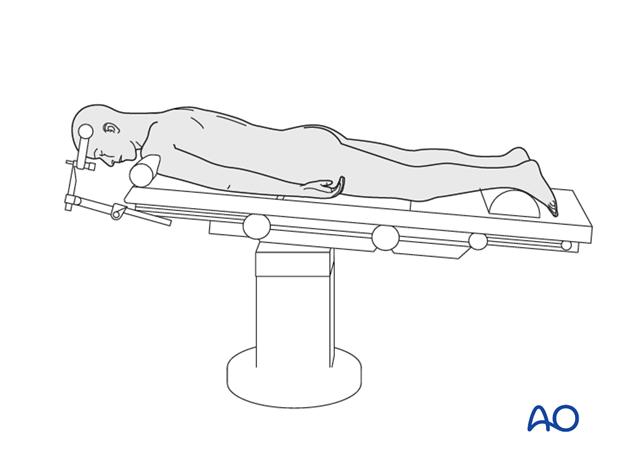
Posterior fixation is achieved with the patient in the prone position, through the posterior approach to the cervical spine.
3. Decompression
A spinal cord anterior compression cannot be addressed by a posterior approach.
On the other hand, nerve root decompression can be achieved directly through the posterior approach by removal of a displaced facet or fragment from the foramen.
4. Reduction
Depending on surgeons preference, reduction can be performed either open or closed.
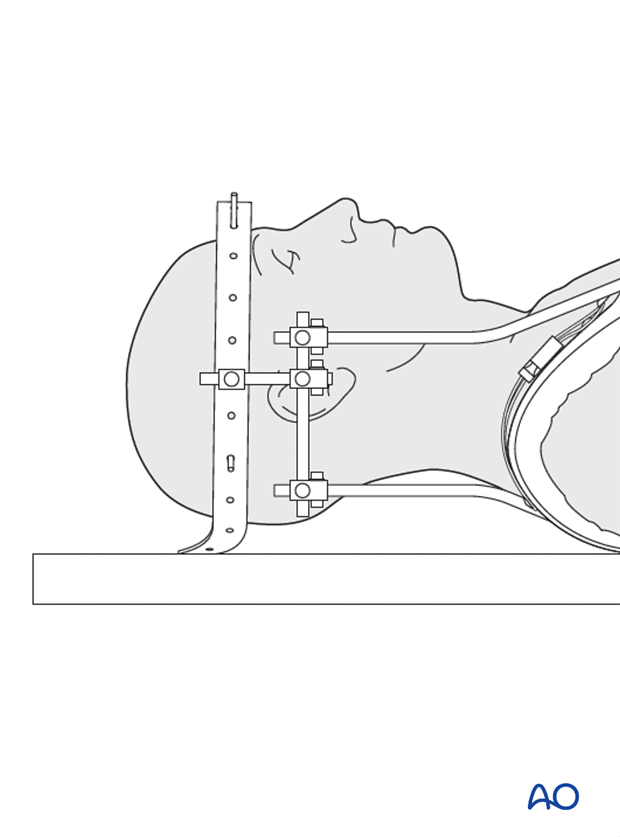
Closed reduction
Closed reduction can be performed preoperatively with:
- halo traction
- halo with manipulation under anaesthesia
If a closed reduction by halo traction is attempted, care should be taken to prevent over-distraction.
Note: A halo device does not only serve for reduction, but is also a temporary immobilization method.
Open reduction
Open reduction can be performed on admission or in case of failed closed reduction.
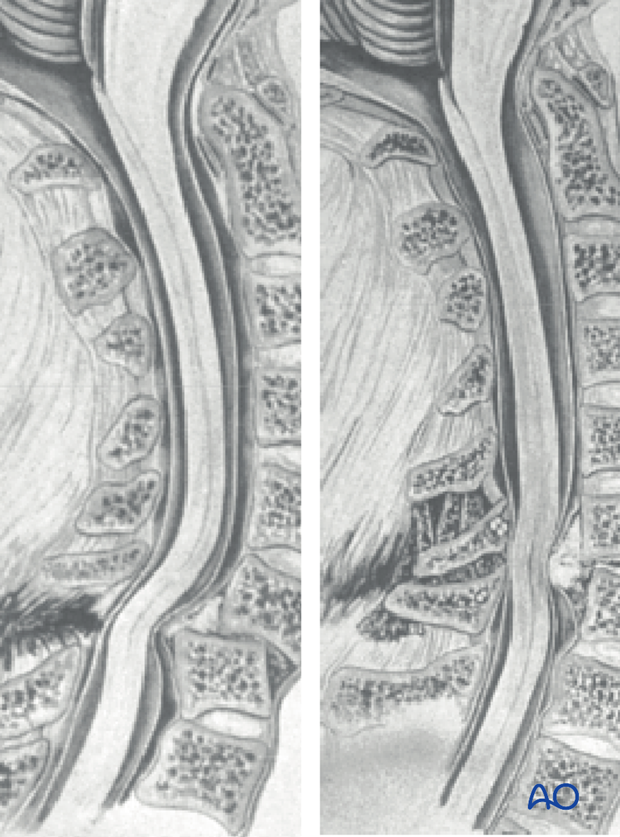
Dislocations can be associated with a significant disk herniation posterior to the anteriorly displaced vertebral body, in which case reduction of the vertebra may drag the herniated disc material into the spinal canal and cause a spinal cord injury.
When MRI rules out disk herniation, the following open reduction maneuver can be performed. In case MRI is not available, then anterior approach with direct disc visualization and removal is the preferred method.
Open reduction of unilateral facet joint dislocation
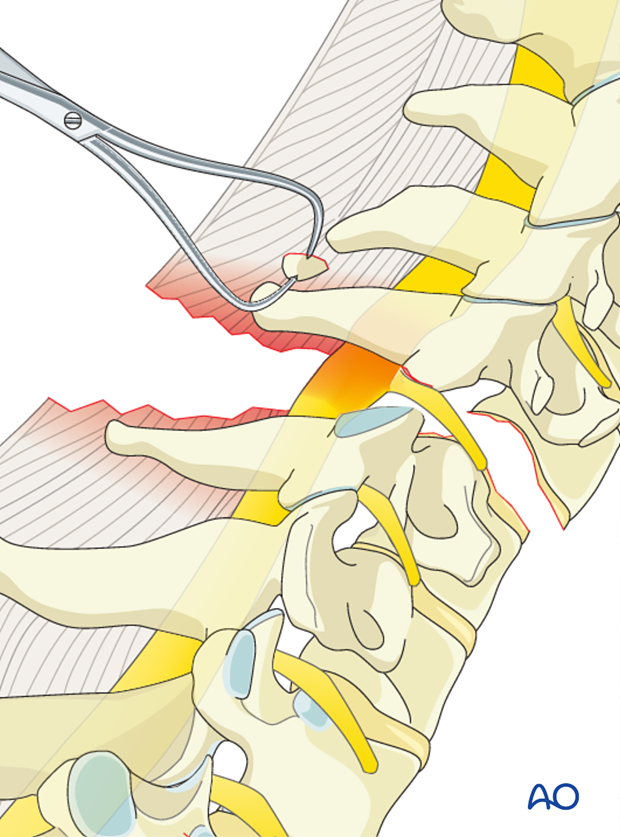
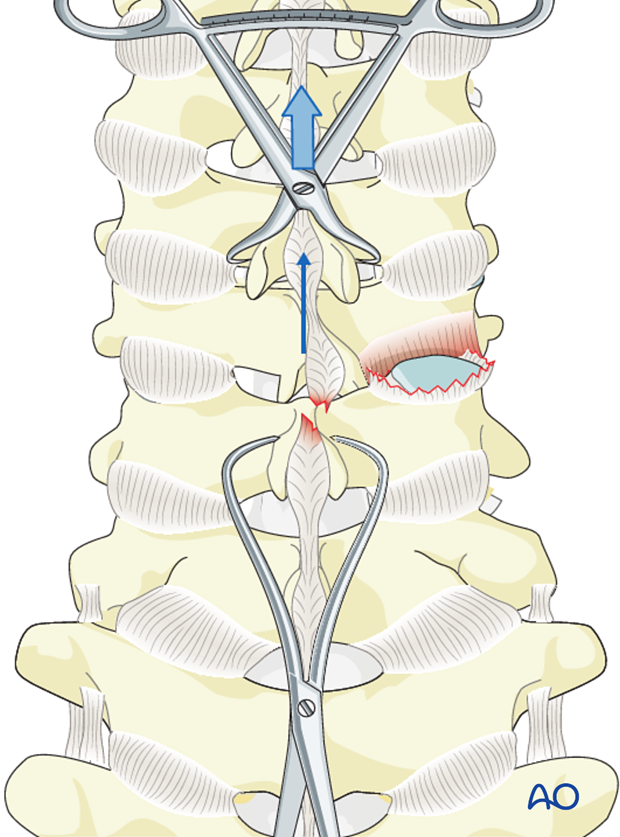
A unilateral facet dislocation can be unlocked with gentle manual distraction applied across clamps placed on the spinous processes above and below the injury.
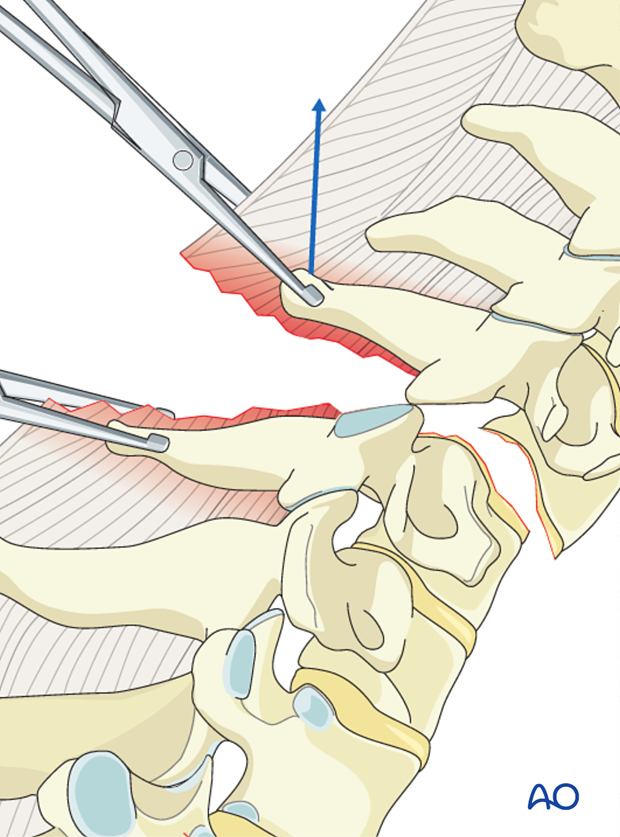
Manual rotation of the spinous process above the level of injury away from the side of the dislocation will reduce the joint and restore the spinal alignment.
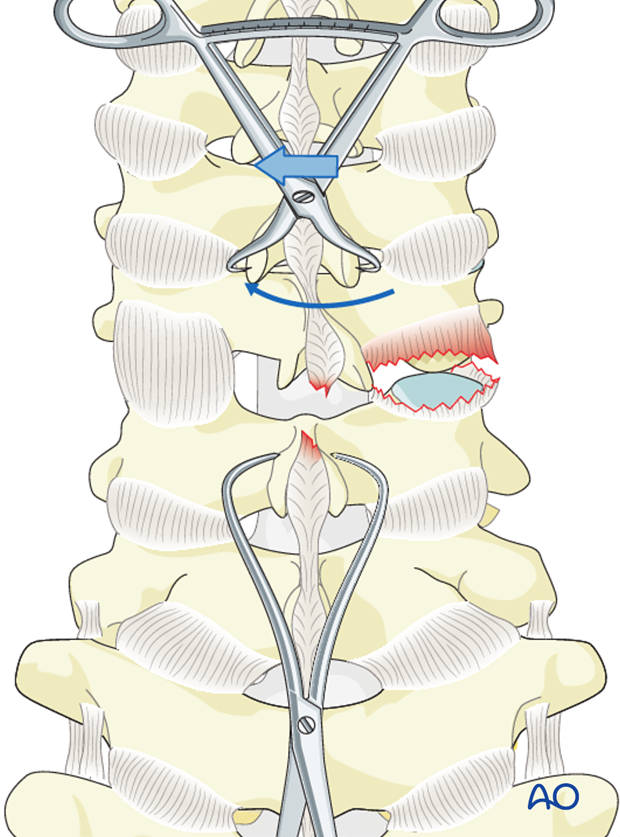
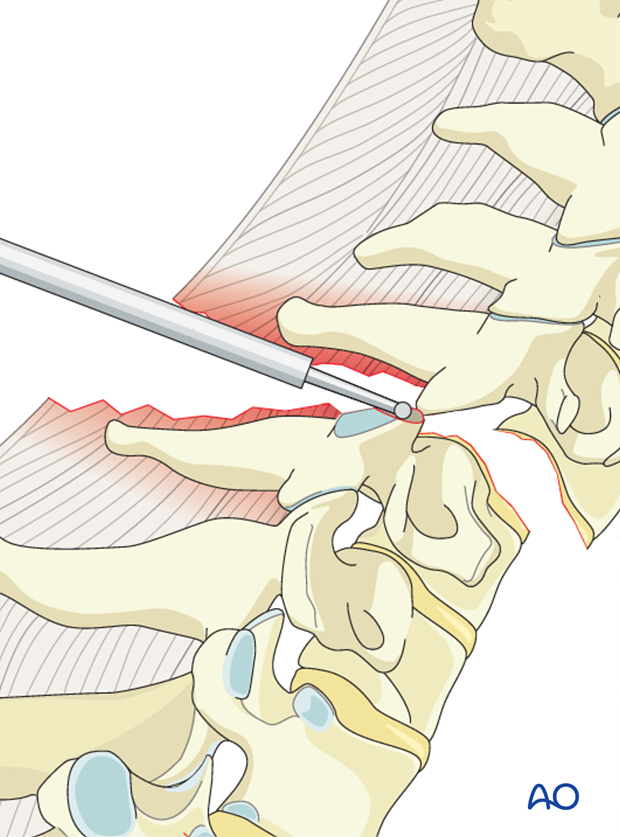
An elevator can be placed between the dislocated facet joints to facilitate reduction
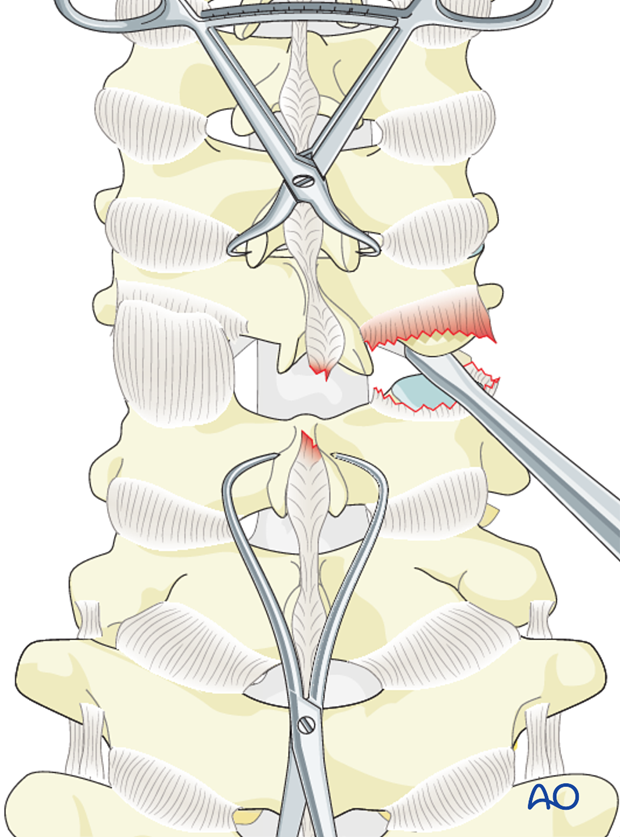
Partial facetectomy in the form of resection of the superior-most projection of the superior facet of the level below the dislocation may facilitate facet reduction.
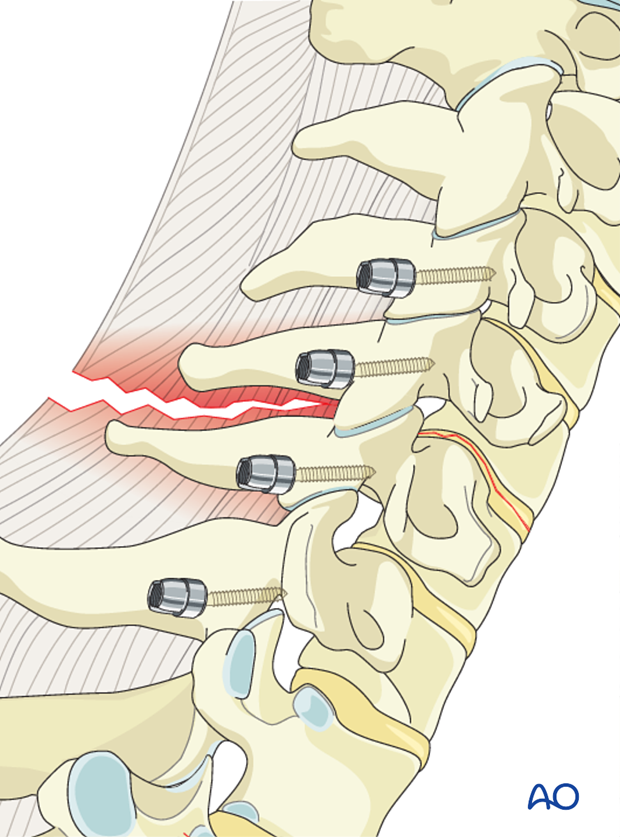
Once reduction has been achieved, posterior instrumentation should be performed.
Bilateral dislocations
A bilateral facet dislocation can be unlocked with gentle manual distraction applied across clamps placed on the spinous processes above and below the injury.
In specific situations, this can be facilitated by prying the facets apart directly with an elevator or partial resection of the superior facet as described above for unilateral facet dislocations
Once reduction has been achieved, posterior instrumentation should be applied.
5. Instrumentation
If the anterior column provides adequate stability for load bearing, and sufficient screw purchase can be achieved in the lateral masses, a C fracture can be treated with only a posterior fixation.
A posterior approach cannot be used as the only fixation technique in the presence of:
- bone intruding in the spinal canal.
- comminution of the anterior column.
- disruption between anterior and posterior column (eg. bilateral pedicle fracture).
When lateral mass fixation is used alone, a lateral mass fracture will require an additional level of fixation.
When an anterior approach is combined with a posterior fixation, posterior instrumentation will include one level above and one level below the disruption or the injured vertebra.
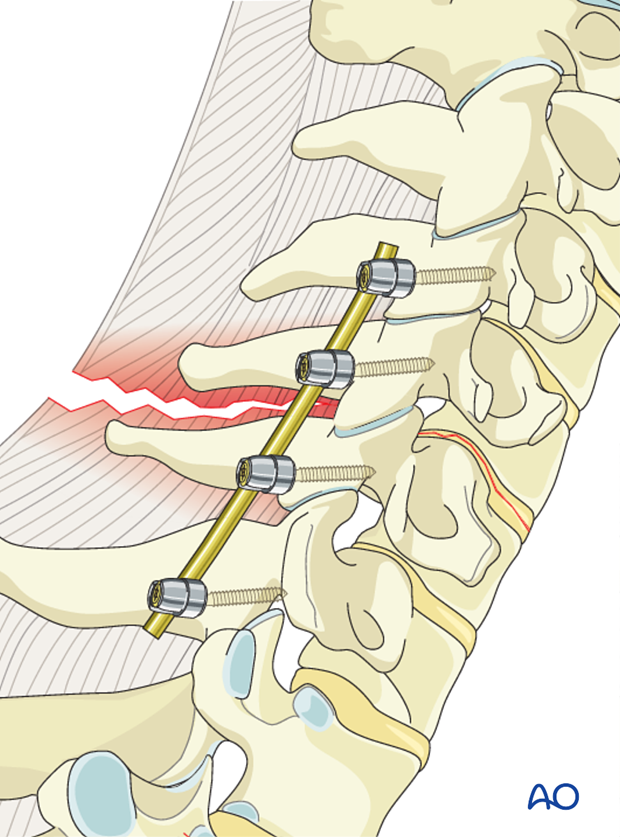
6. Rod insertion
The cervical spine lordosis must be obtained with patient positioning/reduction. The rod should be bent to keep this lordosis.
Incorrect lordosis is one of the main pitfalls of this procedure.
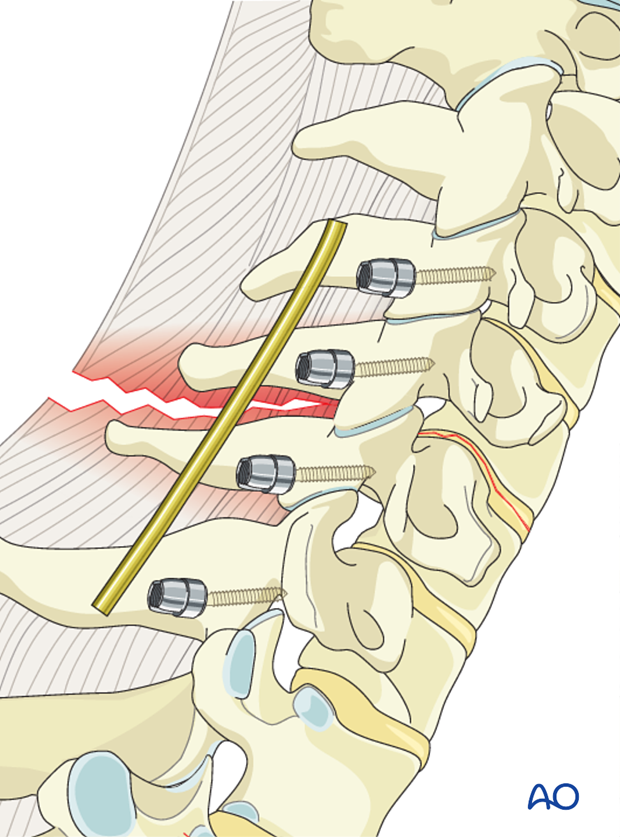
The screws are closed with slight compression to enhance the stability of the construct.
7. Aftercare
Patients are made to sit up in bed on the first day after surgery.
A collar is commonly used following surgical stabilization to moderate patient activity.
The purpose of a collar is to prevent ranges of motion outside of limits deemed unfavorable for fracture healing. Collar is optional.
Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.