Surgical complications associated with cervical trauma surgery
1. Vertebral artery
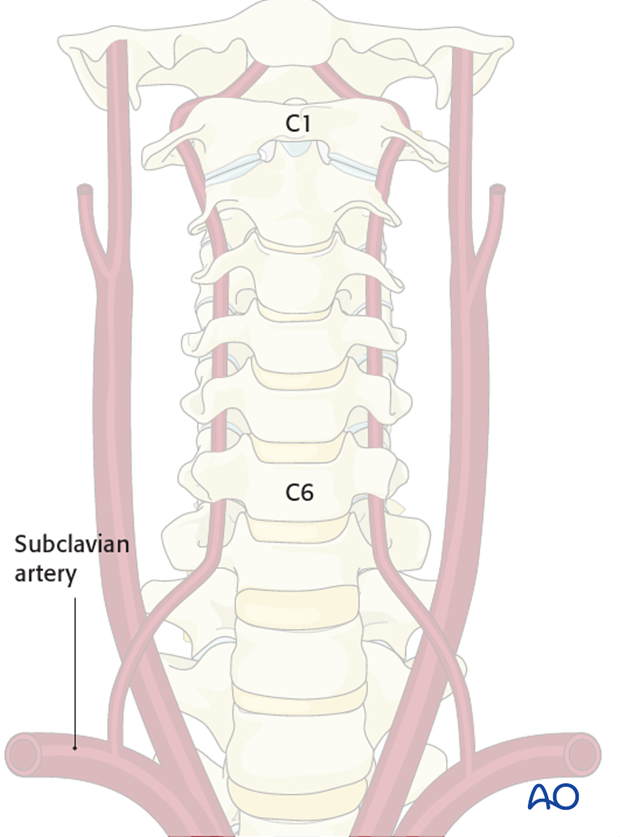
Normal anatomy
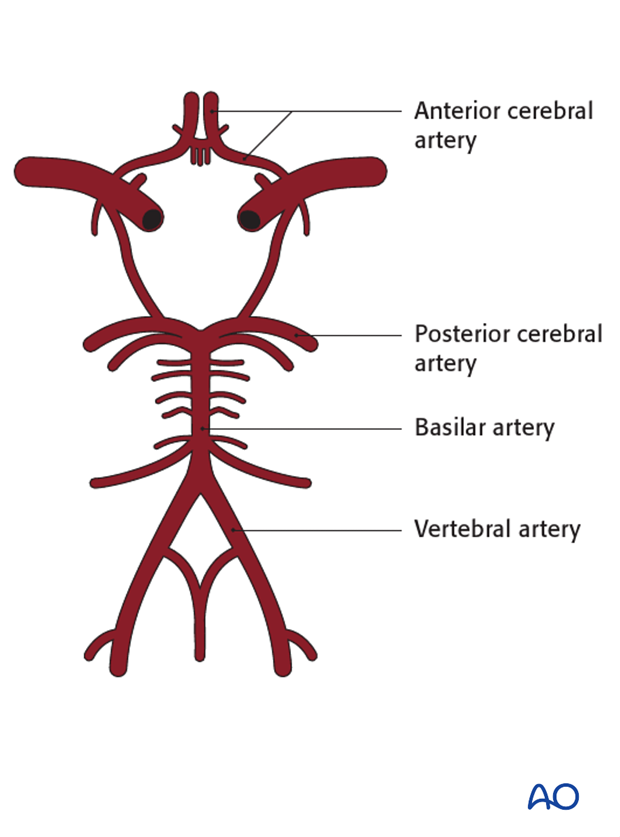
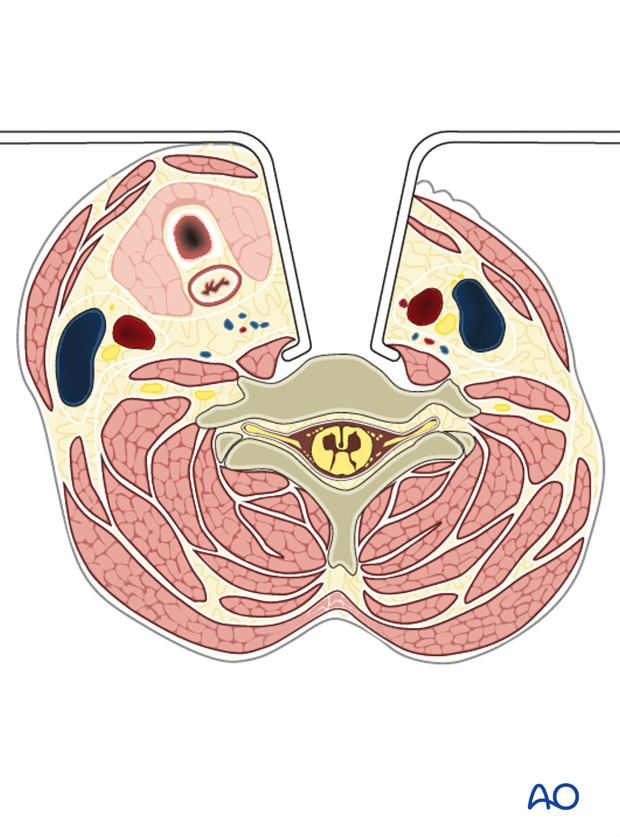
Vertebral arteries branch from the subclavian arteries from both sides, and enter the cervical spine at the level of C6 (in 7.5% of the cases at C7). They course through the transverse foramen in each cervical vertebra, and after they pass through C1, they travel across the posterior arch and enter the foramen magnum.
Inside the skull they join to form the basilar artery. This artery is the main blood supplier to the brain stem and connects to the circle of Willis.
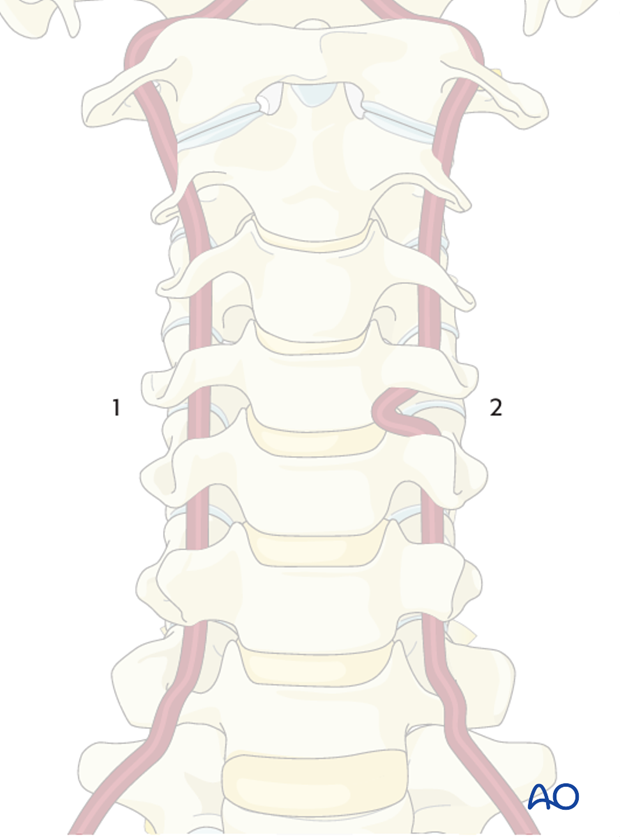
Anatomical variations
The following two variations are associated with an increased risk of intraoperative injury:
- Medial migration of the vertebral artery, especially due to its tortuosity
- Atypical entry of the vertebral artery into the transverse foramen leaving the artery exposed along a major segment in an anterolateral position of the vertebral body
Note: Prior to any surgical procedure, the vertebral artery trajectory must be evaluated.
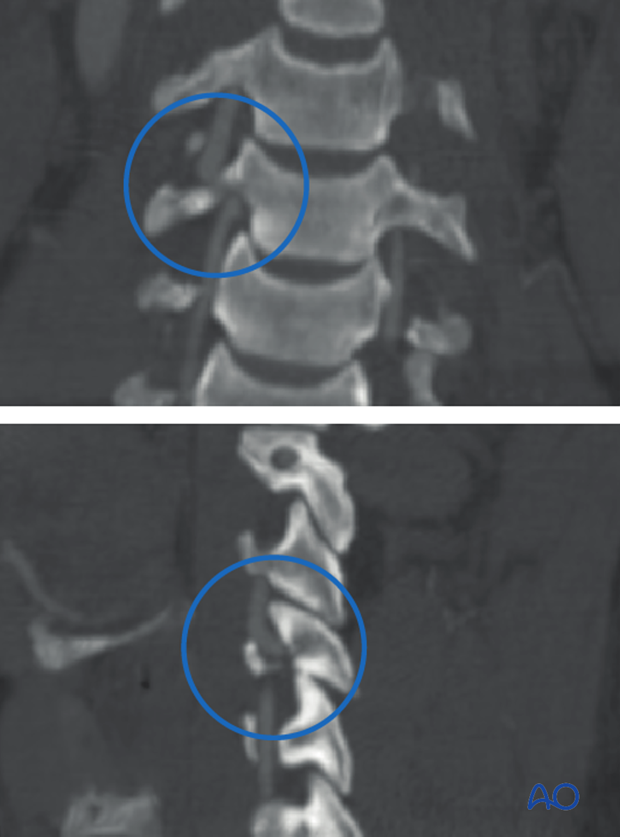
Complications associated with trauma
The incidence of vertebral artery injury associated with spinal fractures ranges from 24-46%. The majority of them are asymptomatic.
Younger patients are usually at lower risk for neurological deficit. Older patients are at increased risk because of possible stenosis or occlusion of the contralateral artery.
CT angiography is the preferred imaging modality. If there are signs of dissection, anti-platelet therapy (aspirin) should be started.
Complications associated with surgery
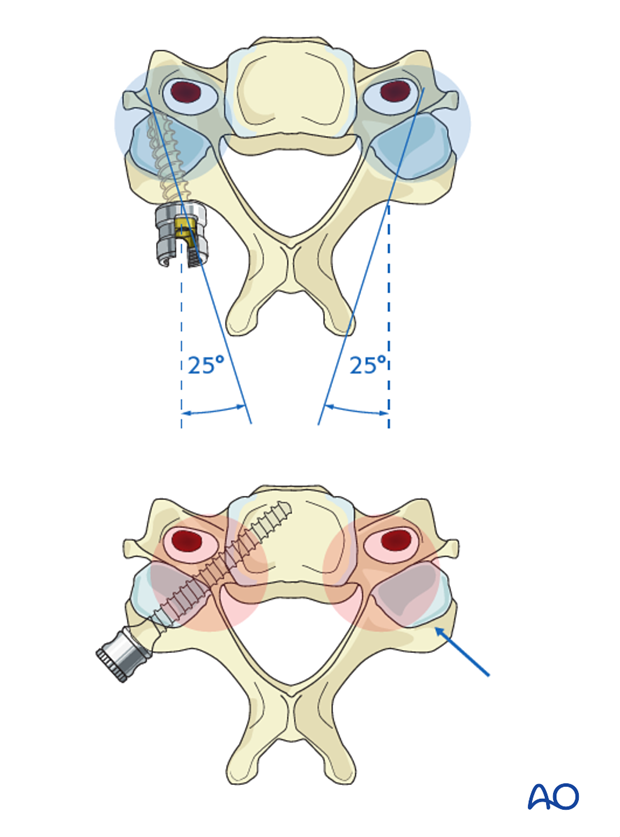
In the subaxial cervical spine, the lateral mass screws are safe, with regard to the vertebral artery, if the drill trajectory respects the 25° angulation.
Placement of pedicle screws in the cervical spine is more prone to cause iatrogenic vertebral artery injury.
In case of an iatrogenic injury to the vertebral artery:
- Insert screw to stop bleeding.
- If bleeding continues, an angiogram is recommended to evaluate the extent of the damage as well as the dominant side; consider stenting or embolization.
- Evaluation by a vascular surgeon may be necessary at this point.
- If the contralateral artery is intact, this injury may remain asymptomatic. If the contralateral side is not instrumented as yet, a safer fixation method (eg. lateral mass crews or a pedicle crew at a different level) should be chosen to prevent the risk of bilateral vertebral artery injury, which may be fatal.
- After surgery, obtain angiogram and consider antithrombic therapy (aspirin)
2. Esophagus perforation
Complications associated with trauma
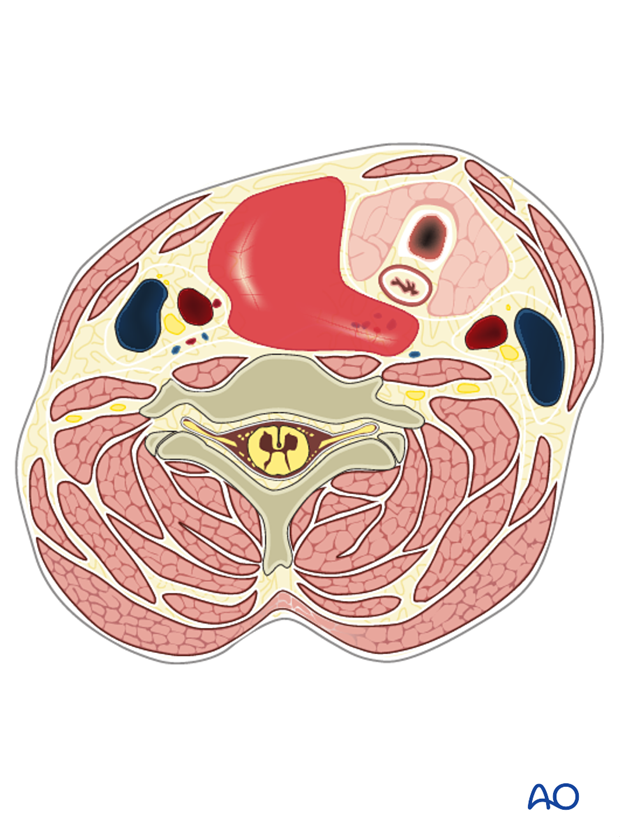
The esophagus is in close contact to the anterior spine at the level of C3 and T4. Damage to the esophagus can be caused by distraction injuries (B3).
In B3 injuries at the level, injury to the esophagus should always be suspected. Free air in the anterior part of the spine is a strong sign of an esophagus or trachea rupture.
Complications associated with surgery
Esophagus injuries occur during the anterior approach with an incidence of 0.2-0.4%. They may cause surgical site infection, cutaneous fistula, or mediastinitis, which is a serious and potentially lethal complication.
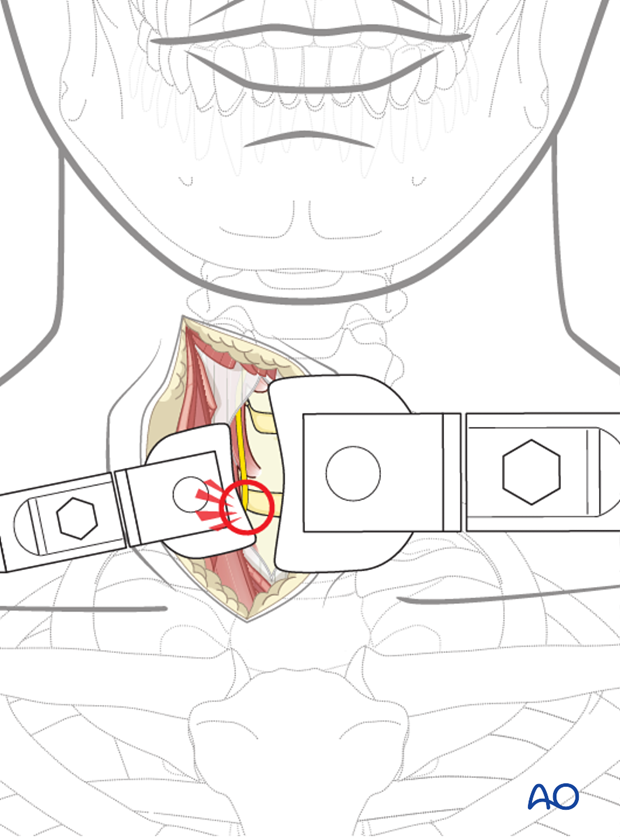
The esophagus is at the greatest risk of injury when the anterior dissection reaches the vertebra as the esophagus lies adjacent to the spine.
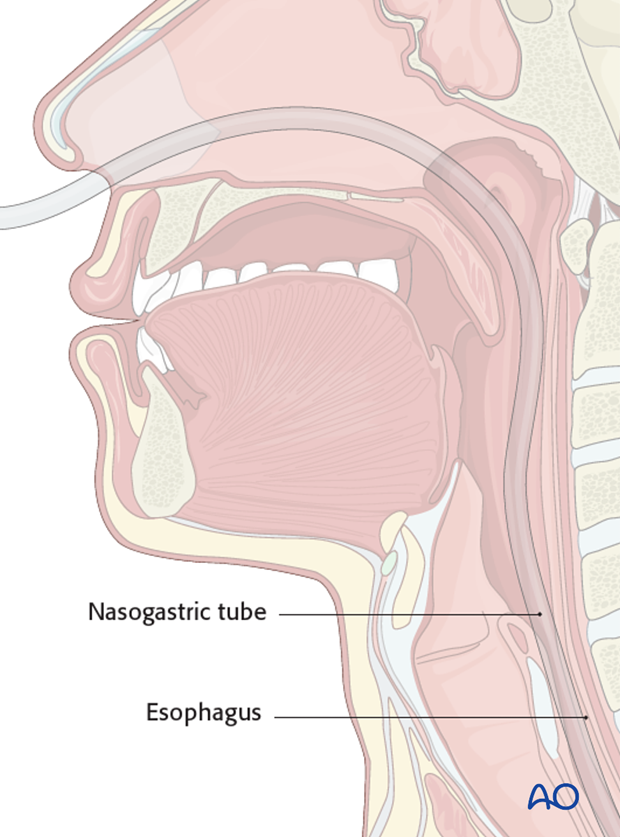
Inserting a tube into the esophagus before surgery may help the surgeon to identify and avoid compromising the esophagus.
Early diagnosis is crucial to prevent infection.
Immediate repair is absolutely necessary.
If there is any doubt regarding injury to the esophagus during surgery, this needs to be clarified using contrast radiograms prior to closure of the wound. An ENT surgeon should be contacted if necessary.
In case of infection after an anterior approach, injury to the esophagus should be suspected. Lateral contrast radiogram with swallowing is used to diagnose any rupture.
3. Post-operative hematoma
After an anterior approach, a hematoma may develop within the first hours and can present as progressive dysphasia or difficulty in breathing. Urgent removal of the hematoma is necessary.
After a posterior approach, epidural hematoma formation may cause neurological deterioration and should be removed immediately.
Postoperative hematoma is best prevented with hemostasis prior to wound closure. Insertion of a drain is recommended.
4. Dysphagia
This is a swallowing difficulty and is one of the most common complaints following anterior cervical surgery (incidence up to 6-9% in some series).
Symptoms are pain during swallowing, coughing, or a feeling of blocked throat. Most symptoms disappear within a couple of weeks.
In case of persistent symptoms, complications of anterior implants should be ruled out (screw pullout, instability of the cage, etc.).
This is a common complication of the anterior approaches.
- Avoid excessive and prolonged retraction (normal retraction shown in illustration)
- Ensure that implants do not protrude.
5. Dysphonia
Prevalence is 1.5-4% after anterior surgery. The recurrent nerve is particularly at risk at the lower cervical segments. To prevent nerve compromise, try to identify the nerve and to protect it during the surgery.
Symptoms are new onset wet voice or hoarseness.
It is usually caused by a recurrent nerve injury:
- Direct damage
- Retraction pressure
- Cuff pressure
Unilateral injury is usually well tolerated. For revision cases, a contralateral approach can only be performed if a preparatory laryngoscope examination shows normal vocal folds to prevent bilateral injury.
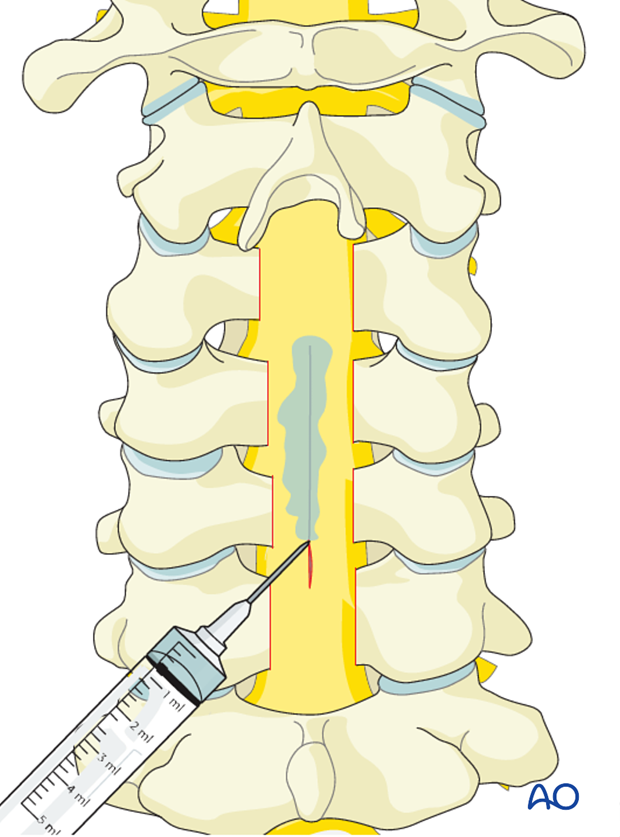
6. Dural tear
A traumatic injury at times can disrupt the dural tube. Disruption can also occur during the surgical intervention.
To prevent dural tears, a surgeon must carefully protect the neural elements during the surgery.
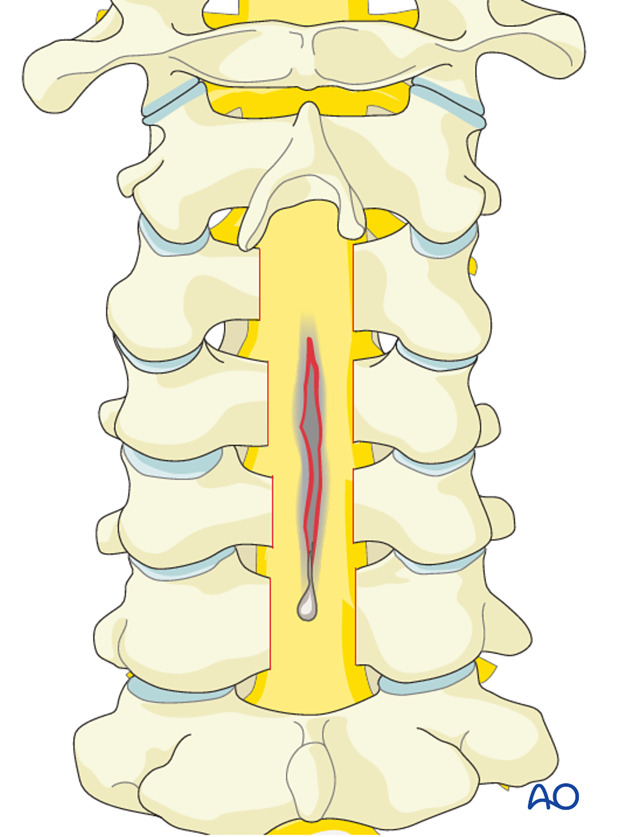
If a dural tear nevertheless occurs, it can be repaired by a standard dural closure technique eg, using standard stitches.
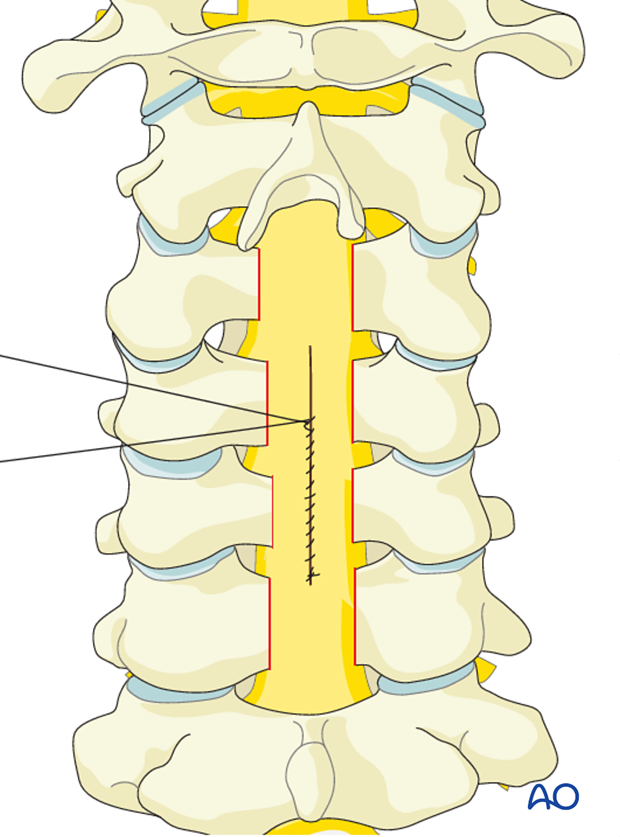
After dural closure, patching or sealing the dura can be performed.