Cervical spine - posterior fixation
1. Introduction
Posterior instrumentation is either combined with open reduction, or is performed after closed reduction has been successfully achieved.
MRI should be obtained preoperatively to rule out the presence of a significant disk herniation before attempting open reduction through a posterior approach.
In certain situations involving the presence of severe neurological compromise after a failed attempt at closed reduction, an open reduction can be performed even without MRI if early reduction is a priority.
Direct decompression of spinal canal caused by a vertebral body fracture intruding into the canal anteriorly cannot be addressed with a posterior approach.
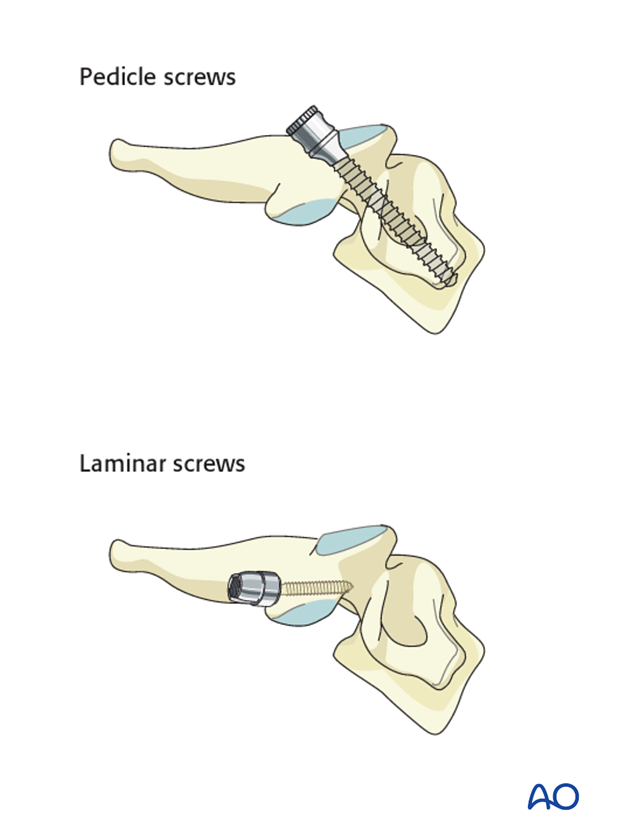
Lateral mass screws vs. pedicle screws
Fixation can be achieved with either lateral mass screws, pedicle screws or combination of the two.
Because lateral mass fixation is generally sufficient, and carries less risk, pedicle screw fixation is limited to rare cases where lateral mass fixation would be insufficient or not possible.
Surgical complications
More details on surgical complications can be found here.
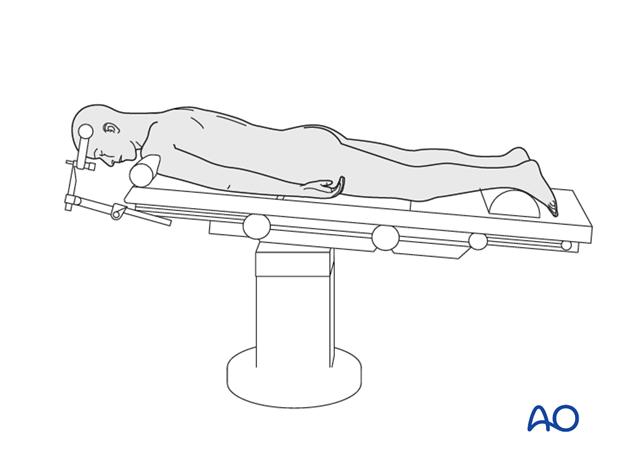
2. Positioning and approach
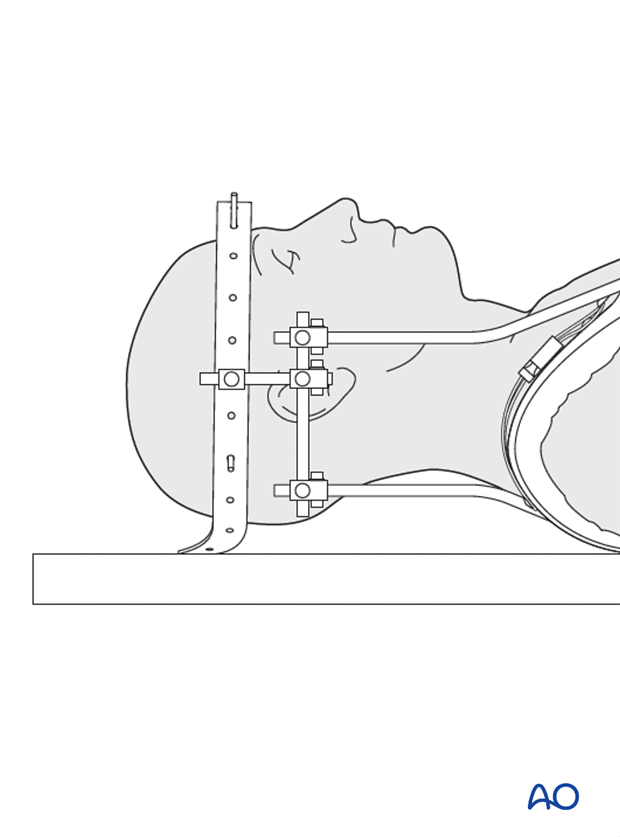
Posterior fixation is achieved with the patient in the prone position, through the posterior approach to the cervical spine.
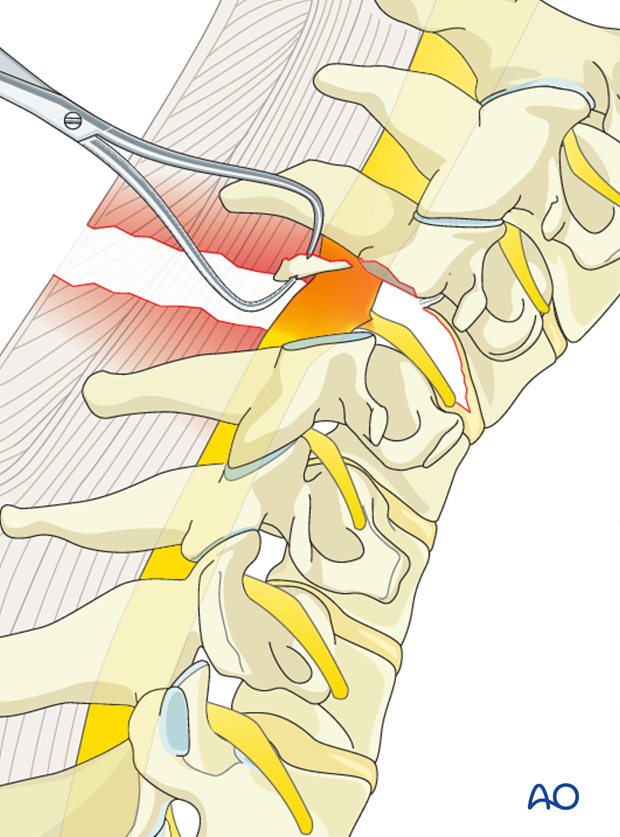
3. Decompression
A spinal cord anterior compression cannot be addressed by a posterior approach.
On the other hand, nerve root decompression can be achieved directly through the posterior approach by removal of a displaced facet or fragment from the foramen.
4. Reduction
Depending on surgeons preference, reduction can be performed either open or closed.
Closed reduction can be performed preoperatively with:
- halo traction
- halo with manipulation under anaesthesia
Open reduction can be performed on admission or in case of failed closed reduction.
When realigning B fractures under traction, care should be taken to prevent over-distraction.
Note: A halo device does not only serve for reduction, but is also an immobilization method.
5. Instrumentation
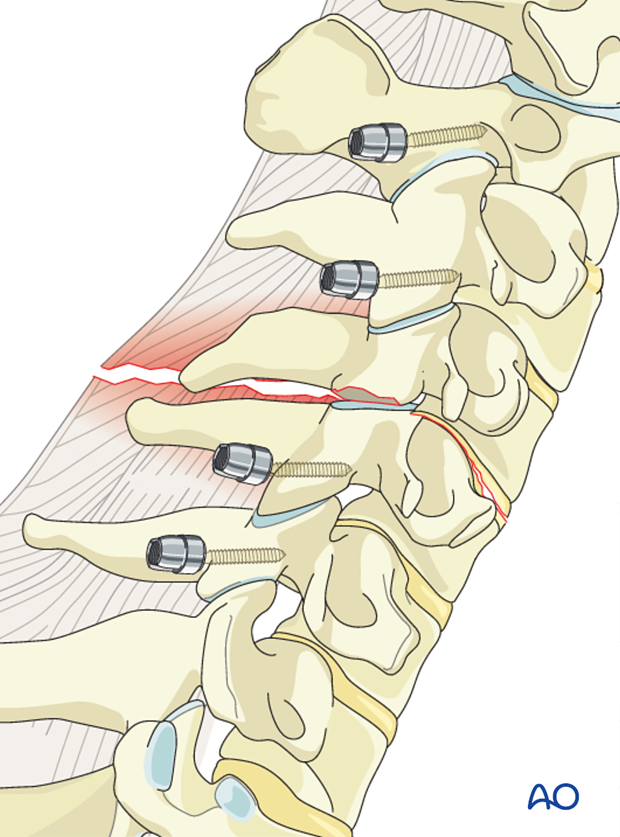
Posterior instrumentation should include one level above and one level below the injured vertebra.
Because dislocation is often associated with fracture of the facet joint, posterior lateral mass stabilization often requires a two-level instrumentation in order to obtain fixation into the first intact lateral mass above and below.
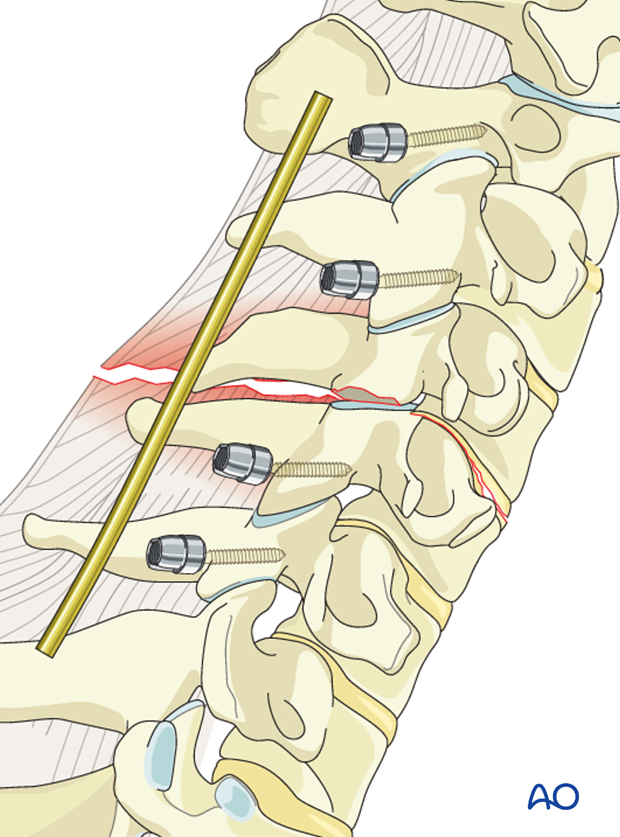
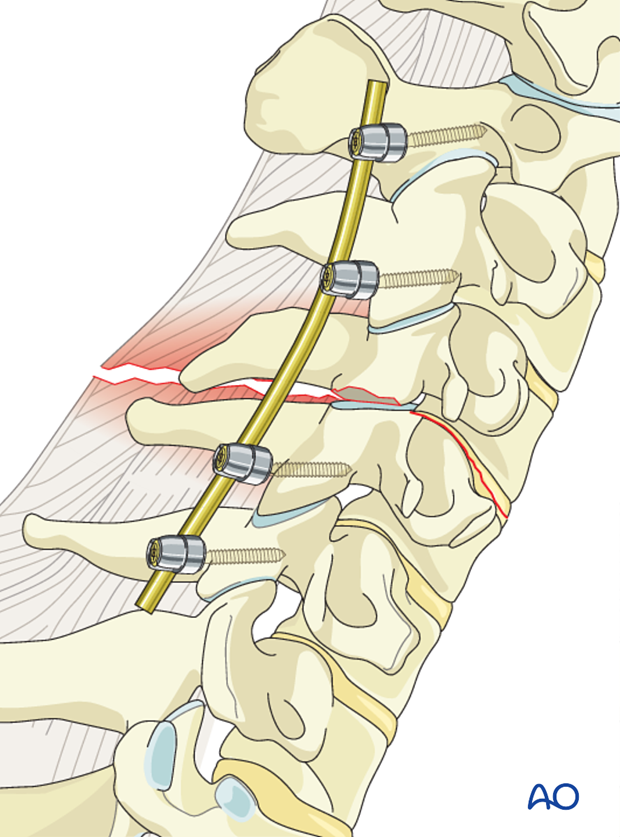
6. Rod insertion
The cervical spine lordosis must be obtained with patient positioning/reduction. The rod should be bent to keep this lordosis.
Incorrect lordosis is one of the main pitfalls of this procedure.
The screws are closed with slight compression to enhance the stability of the construct.
7. Aftercare
Patients are made to sit up in bed on the first day after surgery.
A collar is commonly used following surgical stabilization to moderate patient activity.
The purpose of a collar is to prevent ranges of motion outside of limits deemed unfavorable for fracture healing. Collar is optional.
Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.