Nonoperative
1. Introduction
The decision for operative or nonoperative treatment of pelvic ring injuries is based on:
- Fracture stability, displacement, and pattern
- Patient factors
- Surgical skill and availability of equipment
Pelvic ring stability is assessed by the type and location of fractures and joint injuries involving the pelvic ring.
2. Treatment
Fractures that disrupt the continuity of the pelvic ring or the spinopelvic junction are often unstable. In these injuries the preferred method of treatment is operative reduction and fixation. Nonoperative treatment of unstable pelvic ring injuries is reserved for cases in which the patient cannot undergo surgery.
Reduction
Reduction of pelvic ring displacement can be attempted using nonoperative means such as traction or manual compression.
Although rotational injuries may be reduced and controlled with manual compression, maintenance of this reduction is difficult if not impossible without surgical techniques.
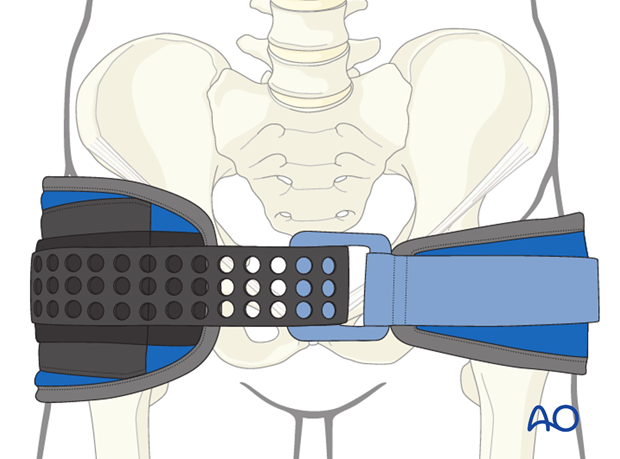
This reduction may be maintained temporarily by nonoperative means, such as a circumferential sheet or binder. However, these techniques of external compression cannot be maintained for more than 24-48 hours due to skin breakdown.
Traction
Cranially displaced injuries may be reduced with manual traction and held in position with skeletal traction and weights. Reduction of the vertical displacement is verified with X-ray. The weight may be adjusted to fine tune the reduction.
Although traction can reduce cranial displacement, it requires up to 3 months for healing in unstable displaced injuries. This results in significant morbidity for the patient due to prolonged bed rest and immobilization. In this case, appropriate nursing is essential to prevent pressure wounds and good respiratory and musculo-skeletal physiotherapy to avoid pulmonary complications
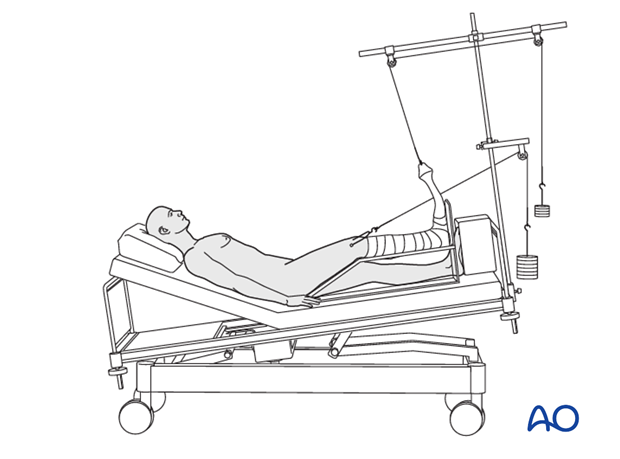
X-ray monitoring during traction
X-rays should be obtained every 1-2 weeks initially to ensure maintenance of reduction. Repeat reduction may be necessary. By 6 weeks, alignment is less likely to change and less frequent X-rays are used to monitor healing. Traction is maintained until there is X-ray evidence of healing (typically up to 3 months).
If radiographic alignment becomes unacceptable, the patient's condition should be reassessed. Delayed correction of pelvic deformity is difficult, and becomes more so with further delay. If the patient's condition has improved enough, surgery or referral should be considered.
After nonoperative treatment is completed, patients should be mobilized with physical therapy and followed for one year to assess outcome and maintenance of reduction.

Patient mobilization
Mobilization after the period of traction should be individualized. Even in a bed bound patient, exercises to avoid stiffness and promote muscle function are advisable.
As soon as the patient is mobile enough, and comfortable enough, discharge from hospital should be possible and encouraged (depending upon other injuries).

Weight bearing
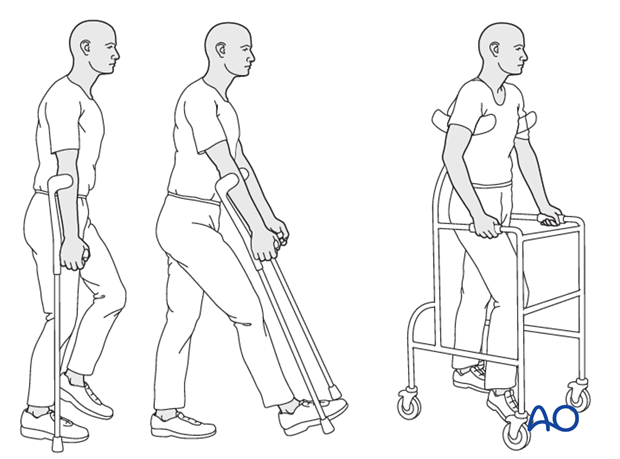
Weight bearing is permitted using crutches or a walker. This can be gradually decreased as comfort and healing permit.
Physiotherapy
Outpatient rehabilitation should be maintained and increase mobility and muscle strength. Contractures should be avoided.
Follow up
Patients should be seen at 6 weeks and 3 months after discharge from the hospital. Follow up X-rays are obtained at these visits to assess fracture healing. In cases of persistent pain (especially low back pain), X-rays should be scrutinized to exclude undiagnosed unstable fracture patterns or nonunions. CT scans may also be helpful in these cases.













