ORIF - Sacral alar plating
1. Introduction
Transverse lower sacral fractures with displacement may injure sacral nerve roots. If perineal sensation or sphincter tone is abnormal, surgical decompression may be indicated. This could involve laminectomy, and if deformity is significant, reduction and fixation of the sacral fracture.
Otherwise, ORIF is indicated for correction of severe deformity or as part of management for open fractures.
Plate fixation of transverse sacral fractures must be performed posteriorly and typically involves the use of two small plates.
The exposure is obtained through a posterior midline sacral approach.
2. Positioning and approach
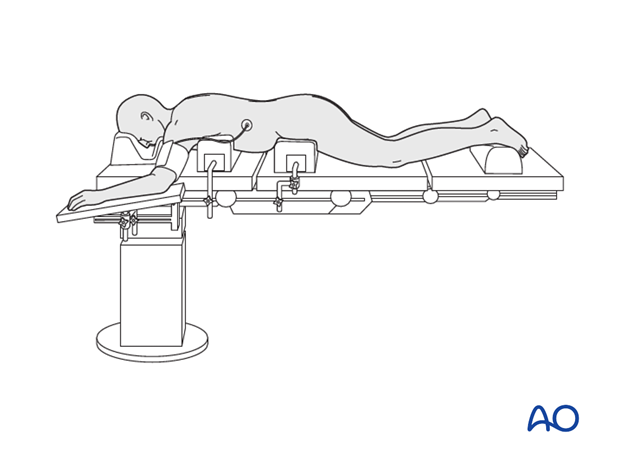
This procedure is performed with the patient placed prone through a midline or paramidline approach.
3. Preparation of the fracture site
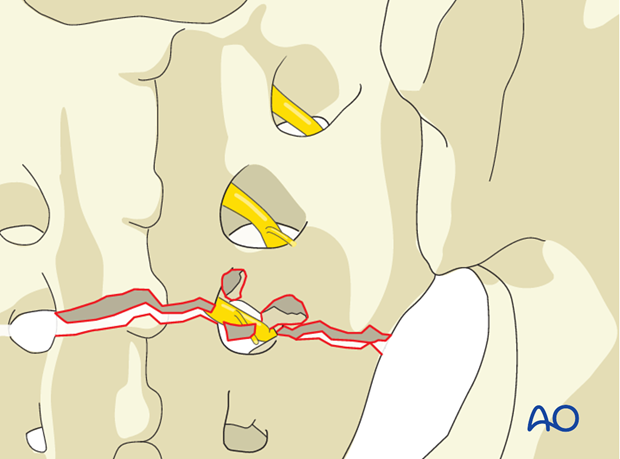
Expose the entire fracture line. Identify and remove small bony fragments from the fracture zone. They may be located in the transforaminal region and hinder fracture reduction.
Sacral nerve root decompression
The complete fracture line has to be cleaned out and inspected.
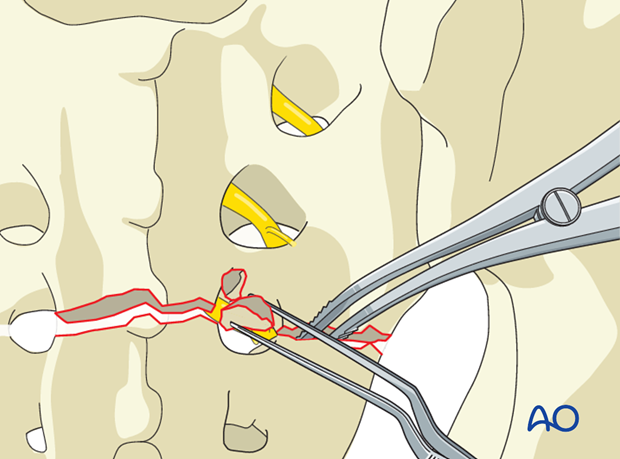
Enhance the exposure by using a lamina (bone) spreader, and carefully placed bone hooks.
Extract bone fragments that may compromise the sacral nerve roots. Fracture reduction may be required to realign the sacral vertebral canal and restore anterior clearance for the neural elements.
4. Reduction
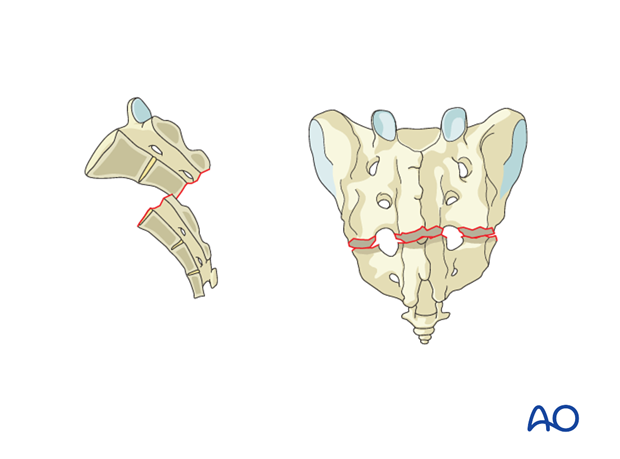
The typical displacement is flexion with possible anterior translation of the distal fragment.
Preliminary fixation
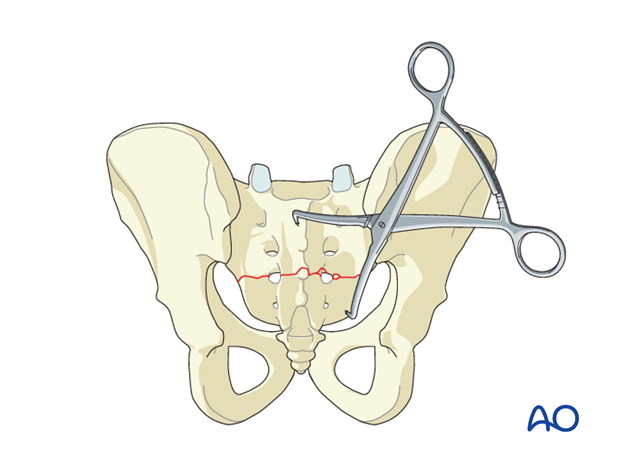
The primary reduction maneuver typically involves the use of two pointed reduction forceps (Weber clamps).
The caudal fragment is grasped and pulled caudally to disimpact and permit reduction. Small elevators can be used to assist disimpaction.
Once reduced, the caudal fragment is clamped to the cranial fragment with pointed reduction forceps.
5. Planning of the internal fixation
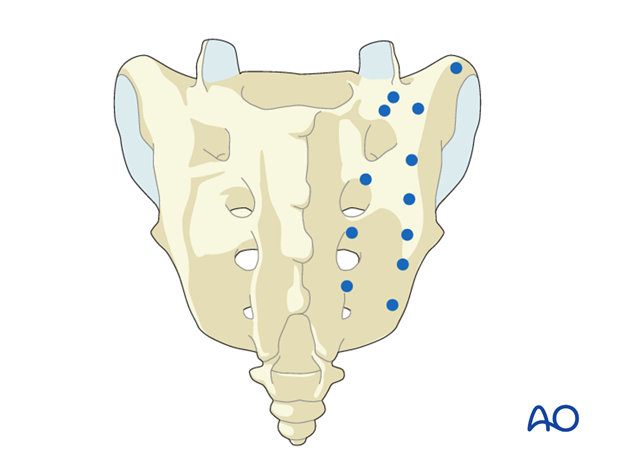
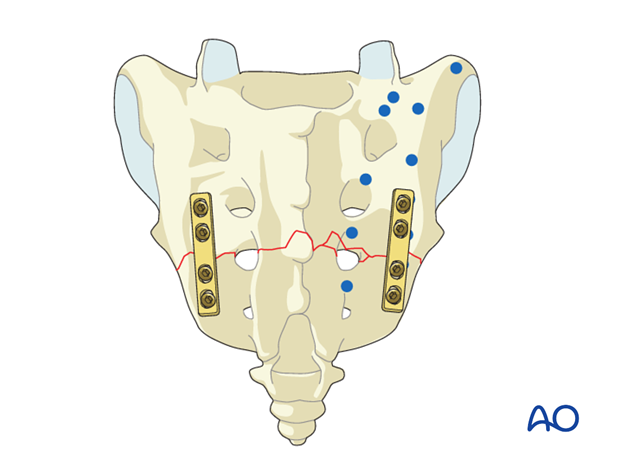
Safe placement of screws avoids the spinal canal and sacral foramina by using the illustrated lateral entry points proximal and distal to the fracture bilaterally. These are lateral to the sacral foramina and nerve roots, or between and in line with the sacral foramina.
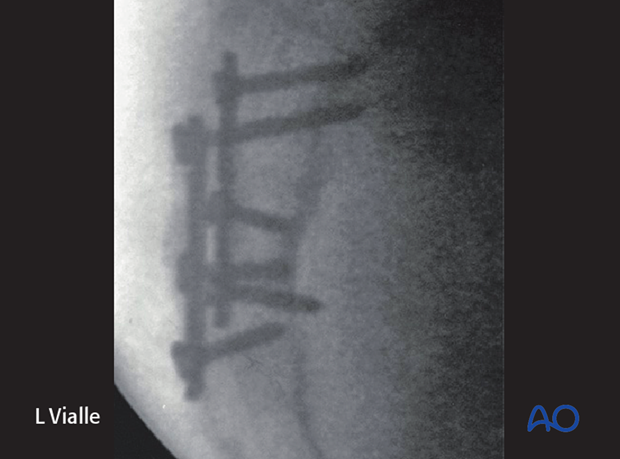
6. Plate application
Fixation is performed with two (bilateral) small fragment plates (4-6 holes). Locking plates may provide enhanced stability.
7. X-ray control
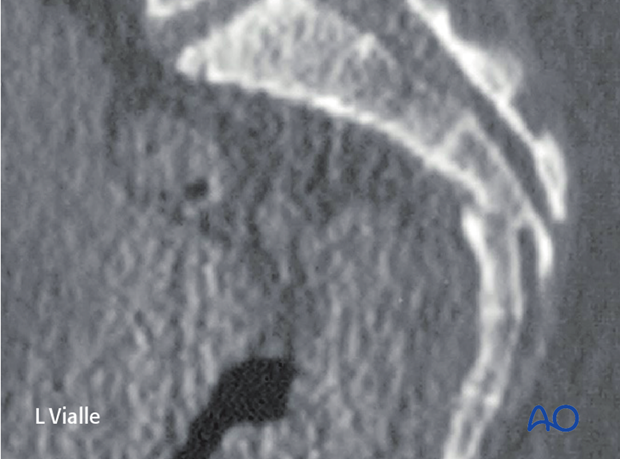
Preoperative lateral CT-view.
Postoperative lateral X-ray view.
Confirm satisfactory reduction and hardware placement on AP & lateral views.
8. Aftercare following open reduction and fixation
Postoperative blood test
After sacral surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Drains, if used, are usually removed after 48 hours.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
- It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
- For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary. - Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises. - Patients who are treated with spino pelvic fixation constructs are typically allowed to bear weight as tolerated unless precluded by other injuries.
The following applies to patients treated without spinopelvic fixation:
- For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
- In unstable unilateral sacral injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
- Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 weeks but use of crutches may need to be continued for three months.
- Fracture healing and sacral alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable sacral fractures and spinopelvic dissociation
Extra precautions are necessary for patients with bilateral unstable sacral fractures and spinopelvic dissociation. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair.
Patients with bilateral unstable sacral fractures and spinopelvic dissociation who are treated with spino pelvic fixation constructs are typically allowed to bear weight as tolerated unless precluded by other injuries.
The following applies to patients treated without spinopelvic fixation:
- For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
- After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













