Laminectomy
1. Introduction
Fracture displacement and comminution can result in spinal canal compromise and nerve root compression causing neurological deficits.
Decompression can be achieved:
- Indirectly
- Directly
Indirect decompression results from realignment of the fracture which can restore the patency of the spinal canal and neuroforamina.
Direct decompression requires access to the spinal canal via laminectomy or foraminotomy to remove compressive lesions caused by fracture fragments.
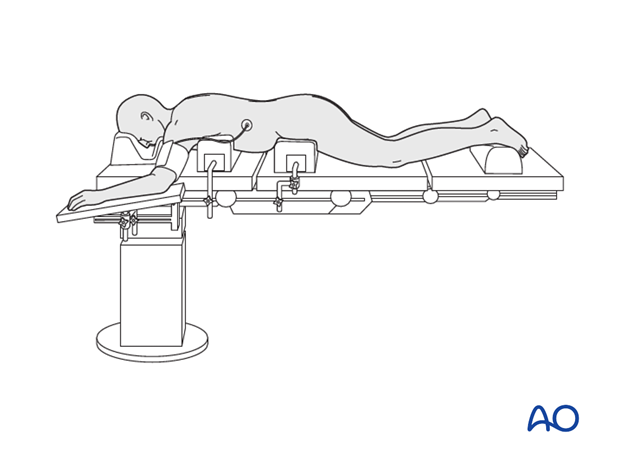
2. Positioning and approach
This procedure is performed with the patient placed prone through a midline or paramidline approach.
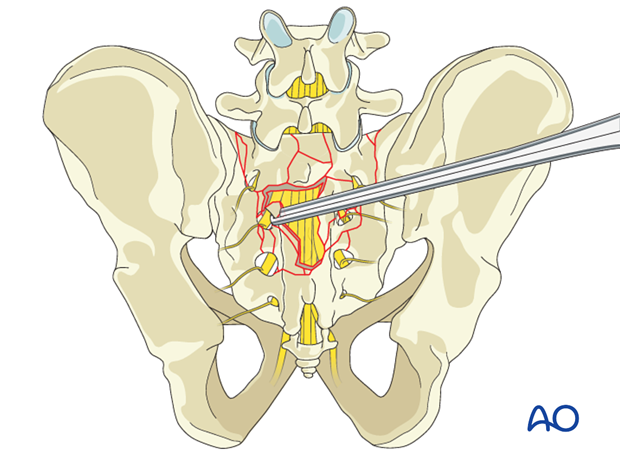
3. Laminectomy of comminuted sacral lamina
In the case of comminuted fractures of the posterior element of the sacrum, much of the laminectomy is performed by merely mobilizing and removing these free fracture fragments.
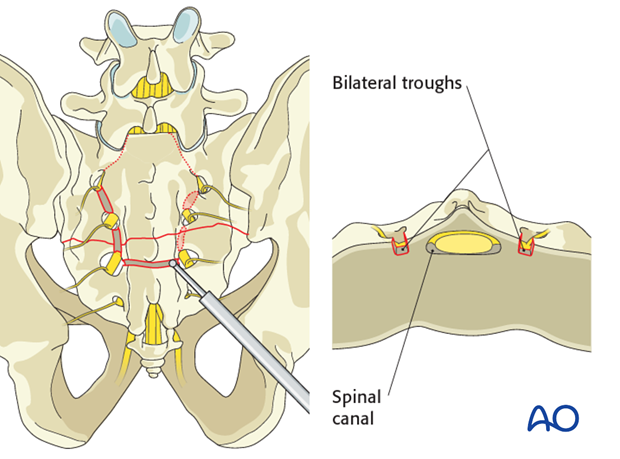
4. Laminectomy of intact sacral lamina
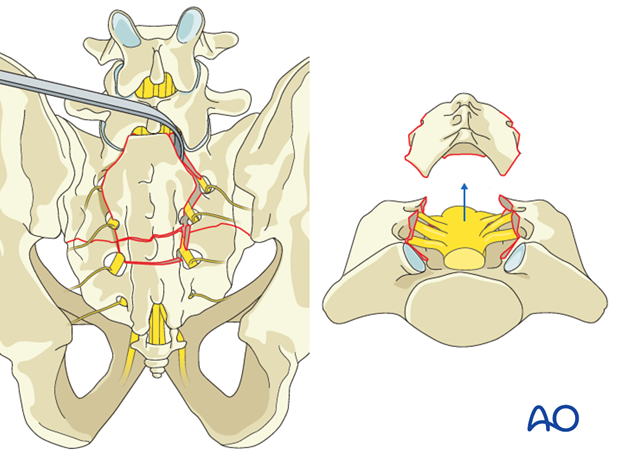
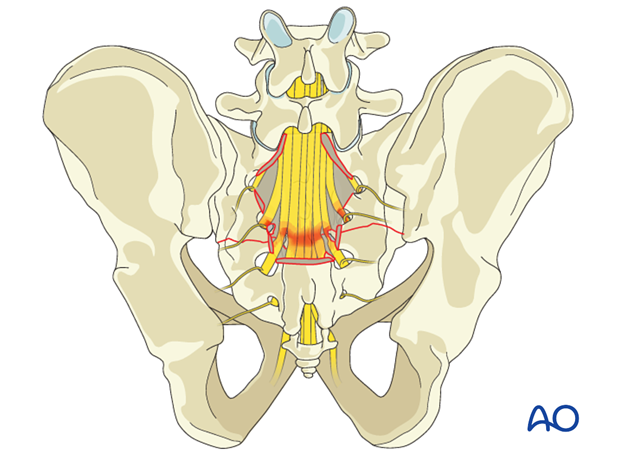
Intact sacral lamina can be removed with a high speed burr using a bilateral through technique.
Vertical troughs are placed bilaterally just medial to the pedicles of the sacral levels being decompressed and are connected at the caudal extent of the laminectomy by a horizontal through.
The troughs are carefully extended through the ventral cortex of the lamina
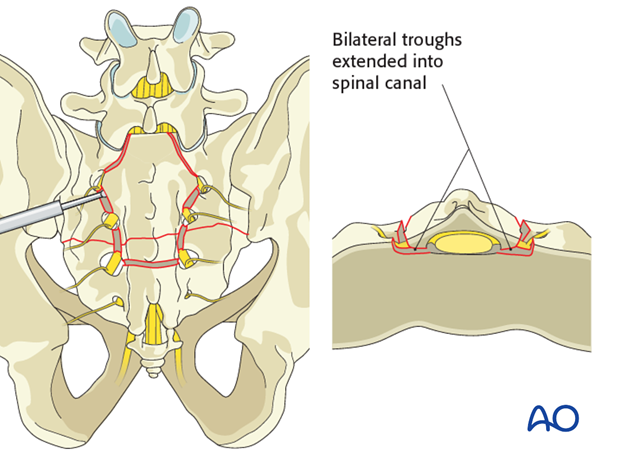
The lamina is then lifted of the underlying nerve roots with an up-angled curette.
5. Decompression
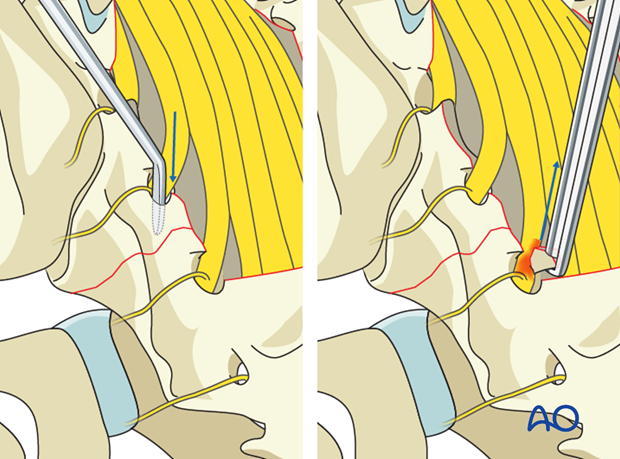
The canal is then explored to identify nerve root injury, dural tear, and remaining compression due to malalignment of the anterior spinal canal. Compressive bone fragments such as comminuted bone fragments and bone at the apex of kyphotic fracture malalignment should be removed.
Decompression of the foramina should be ascertained by unimpeded passage of a curved instrument along the nerve roots throughout the entire course of each foramen. Any residual foraminal compression should be addressed with a Kerrison rongeur.
Water tight suture repair of CSF leaks is performed if possible. With unrepairable tears alternative options can be used such as fibrin glue, allograft, and patches.
In the case of nerve root transection there is no evidence to support nerve root repair.













