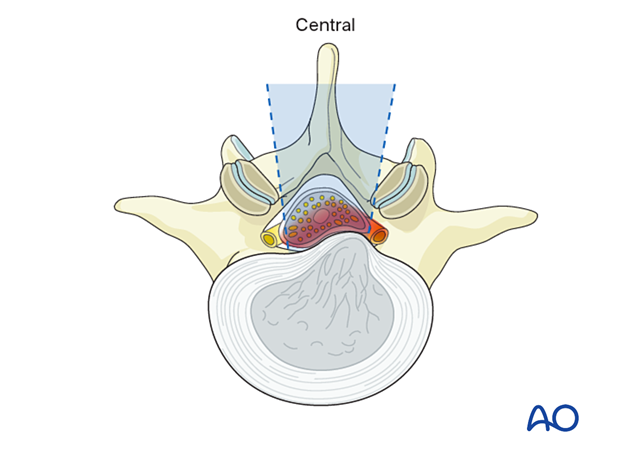
Lumbar disc herniation – central and posterolateral
Central and posterolateral lumbar disc herniations are the most common symptomatic types of disc herniations and typically occur due to the axial biomechanical forces on these discs.
Presentation may include symptoms of cauda equina or nerve root compression. These include radiculopathy, sensorimotor deficits, bowel/bladder issues, neurogenic claudication, and lower back pain.
In large central disc herniation cases, cauda equina syndrome can occur, where the patients present with acute urinary retention/incontinence, saddle anesthesia, and lower extremity weakness. Cauda equina syndrome is a surgical emergency, and decompression should be sought as soon as possible to prevent permanent deficits.
Posterolateral disc herniations are sometimes referred to as paracentral, subarticular, or lateral recess herniations. Depending on the exact location and size of the disc herniation, the traversing nerve root at that level may be compressed.
In cases with a very large posterolateral disc herniation, there may be an extension into the foraminal zone and compression of the exiting nerve root as well.
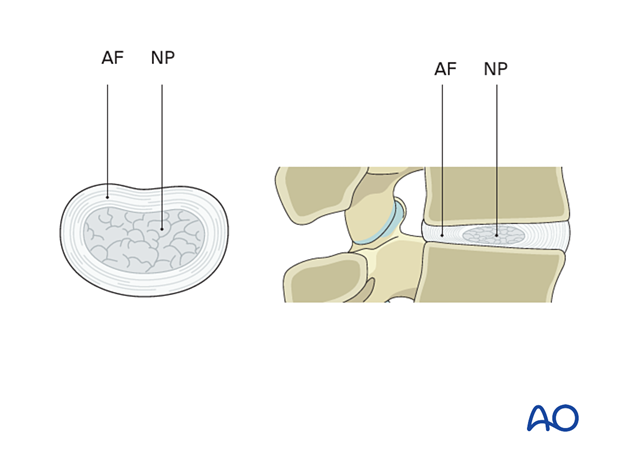
The intervertebral disc is built up of a thick collagen-rich annulus fibrosis (AF) containing a gelatinous proteoglycan-rich nucleus pulposus (NP).
Tears or weakening of the AF can result from degenerative changes or trauma and result in bulging or expulsion of NP material, leading to compression of surrounding neural structures.
The consequences of disc herniation will depend on the neural structures at the location of the disc herniation.
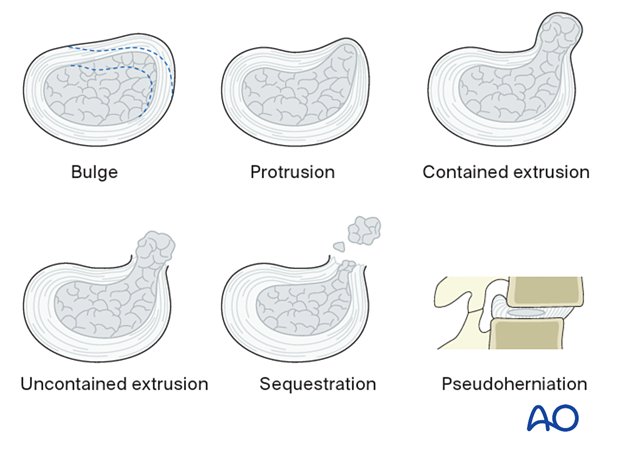
Six different types of disc pathologies can be seen:
- Bulge (without herniation)
- Protrusion (prolapse): the displaced material is less than the base of the displaced material
- Contained extrusion: the displaced material is wider than the base of the displaced material, and annular fibers are intact
- Uncontained/defect extrusion: materials extrude beyond an annular defect
- Sequestration – discontinuous with native disc
- Pseudoherniation – the appearance of a bulging disc due to spondylolisthesis. Note that the disc material does not extend posterior to the posterior spinal line.
Protrusion, extrusion, and sequestration are collectively referred to as disc herniations.