Retroperitoneal approach for Anterior lumbar interbody fusion (ALIF)
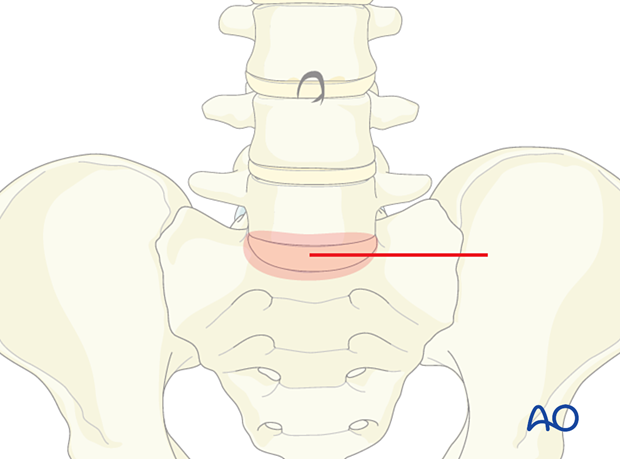
1. Skin incision
The skin incision should be strictly correlated to the level to approach, usually to the left of the midline. The ‘ideal’ incision should be minimal, horizontal, usually 6–7 cm long, and oriented slightly to the left, similar to the Pfannenstiel incision. Other incisions should be considered according to the patient’s size or other technical issues.
The incision needs to take the sacral slope into account.
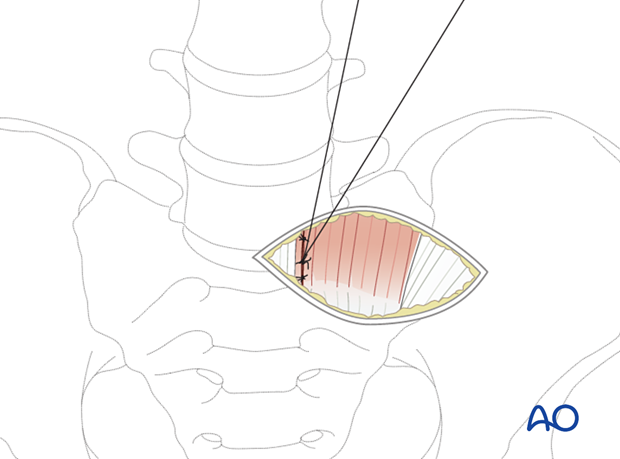
2. Blunt finger dissection
Blunt finger dissection is used to mobilize the skin and soft tissues of the left anterior rectus sheath. The anterior rectus sheath is then opened longitudinally near the midline using electrocautery.
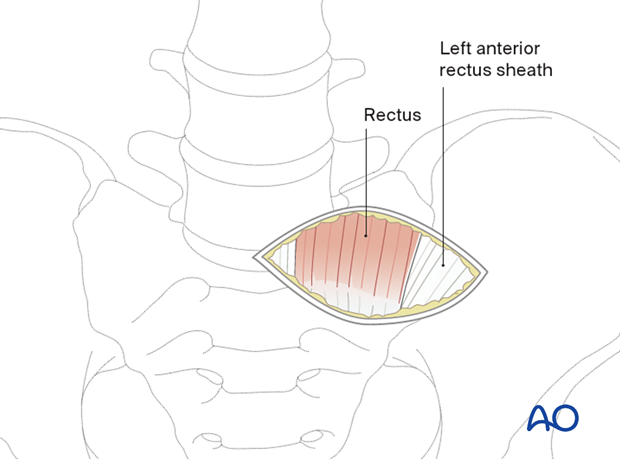
The medial border of the intrafascial rectus muscle is mobilized over a cranial to caudal distance of approximately 10 cm.
The muscle is then mobilized laterally to expose the underlying arcuate line.
This step is fundamental: the arcuate ligament marks the caudal aspect of the incomplete posterior rectus sheath.
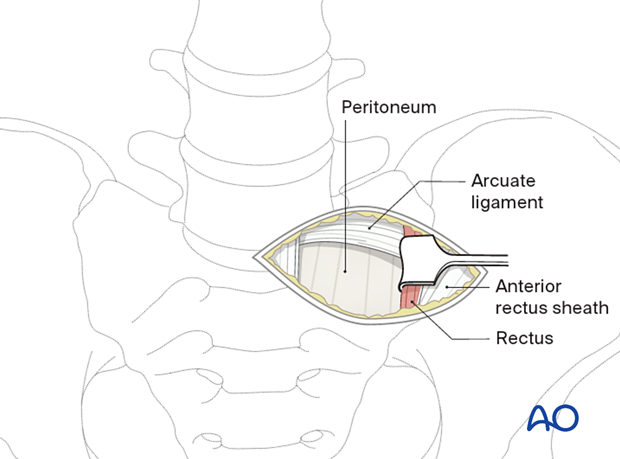
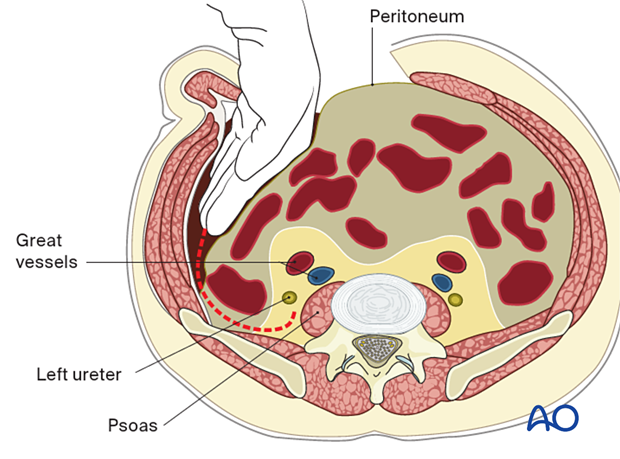
Inserting the fingers and then the entire hand into the retroperitoneal space allows the surgeon to sweep the intraperitoneal contents superiorly, inferiorly, and medially to reveal the spinal column in the midline.
Because this maneuver relies mostly on palpation and not visualization, relevant anatomy must be familiar to the surgeon. The identification of the psoas muscles makes it possible to locate and palpate the left great vessels.
This helps to avoid vascular injuries. In addition, care must be taken to avoid tears in the peritoneal lining.
The ureter must be identified to prevent inadvertent injuries.
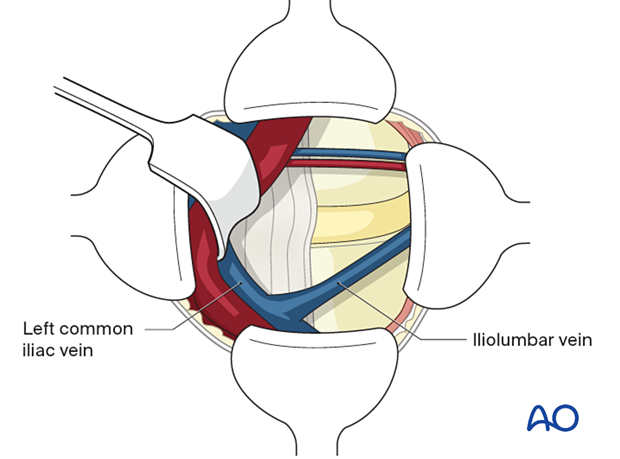
3. Exposure
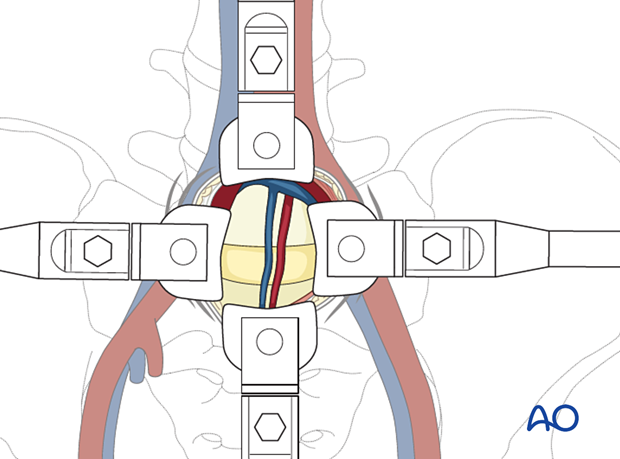
Deep, self-retaining abdominal retractors can now be placed to maintain a sufficient corridor to the disc space.
An alternative method is to use Steinmann pins to circumscribe the working area. The retractors should be securely locked, to avoid unexpected mobilization that can injure the surrounding structures.
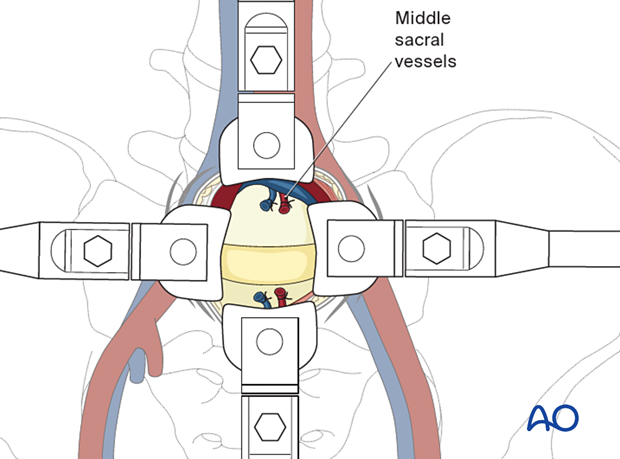
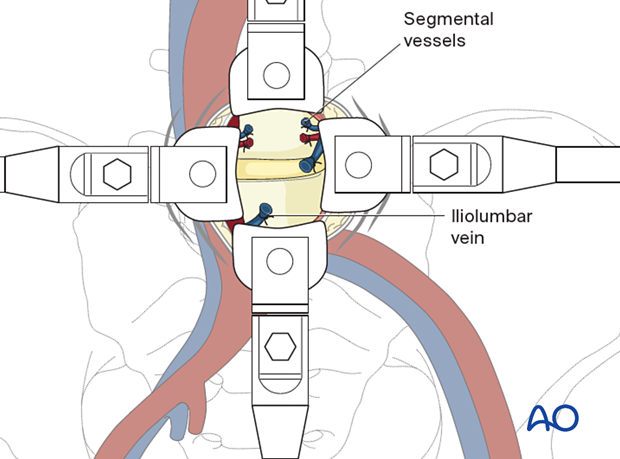
At the level of L4–L5 or L3–L4 the aorta and vena cava must be retracted to the right using blunt dissection with a sponge stick.
Segmental arteries and veins must be ligated.
The regional vascular anatomy must be carefully studied preoperatively with an angiogram or CT scan because of the different patterns of vascularization.
4. Closure
The fascia can be closed after careful visualization of all the anatomical structures that have been passed through during the approach. The remainder of the wound should be sutured in a standard fashion, usually without drainage.