Anterior fusion of L5-S1
1. Introduction
Managing spondylolisthesis requires good knowledge of lumbosacral anatomy.
The goals of the surgical management is to alleviate pain by achieving:
- Solid fusion across the deformity
- Neural decompression
The goal of the surgery is to
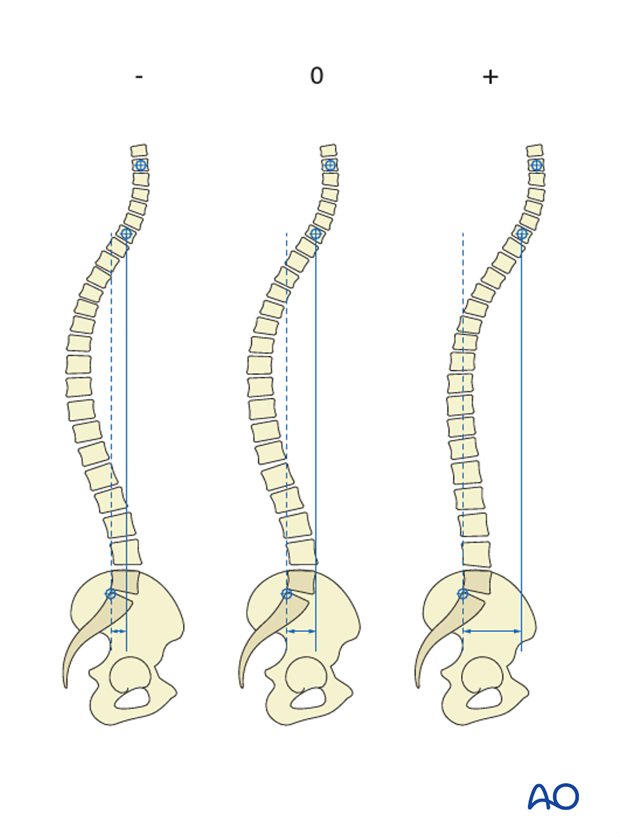
- Ensure sagittal balance
- Prevent further slippage
- Reduce pain
- Maintain neurological integrity
2. Preparation and approach
This procedure is performed through the retroperitoneal approach with the patient placed supine.
3. Discectomy
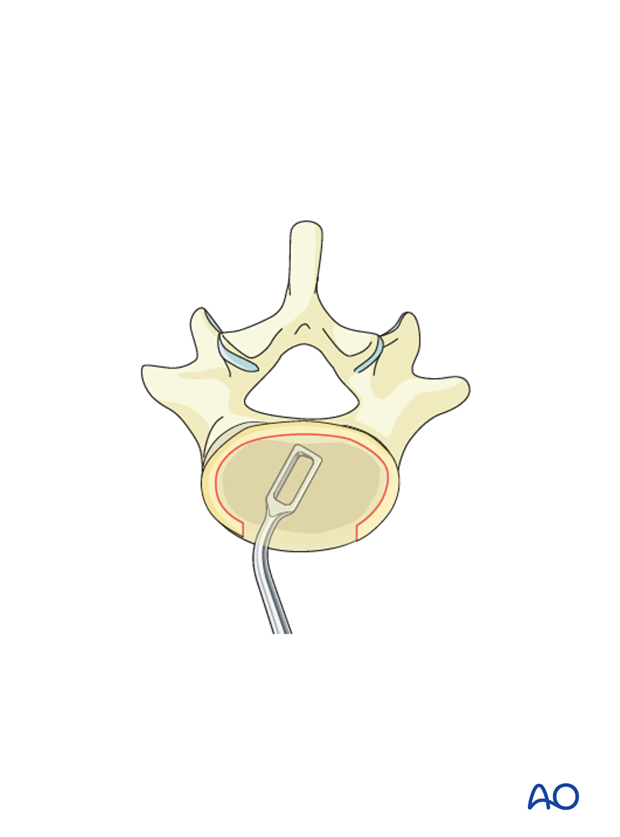
Identify the lateral borders of the L5-S1 disk.
Incise midline in a vertical fashion the anterior annulus and develop a flap on either side.
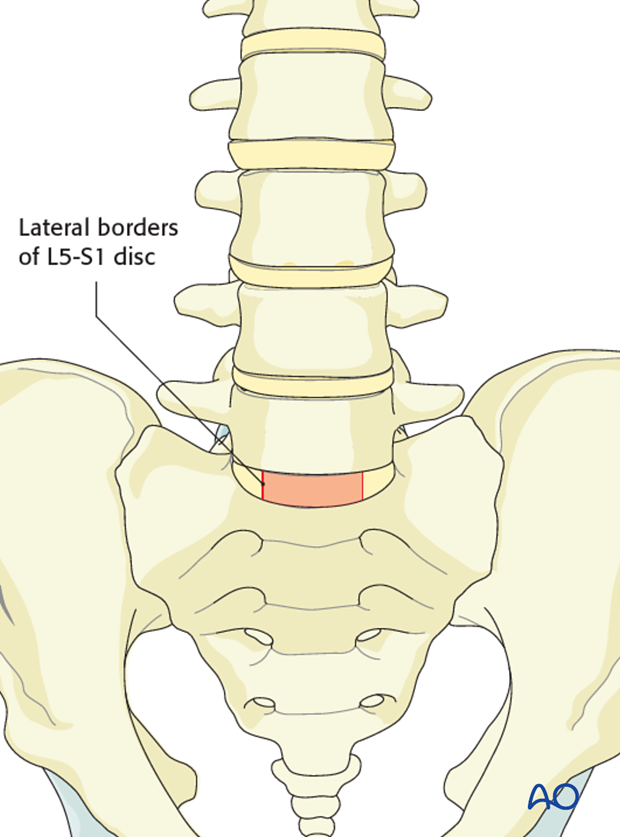
Proceed to remove the disk down to subcentral bone. Care must be taken not to enter epidural space.
The use of laminar spreaders will facilitate disk removal.
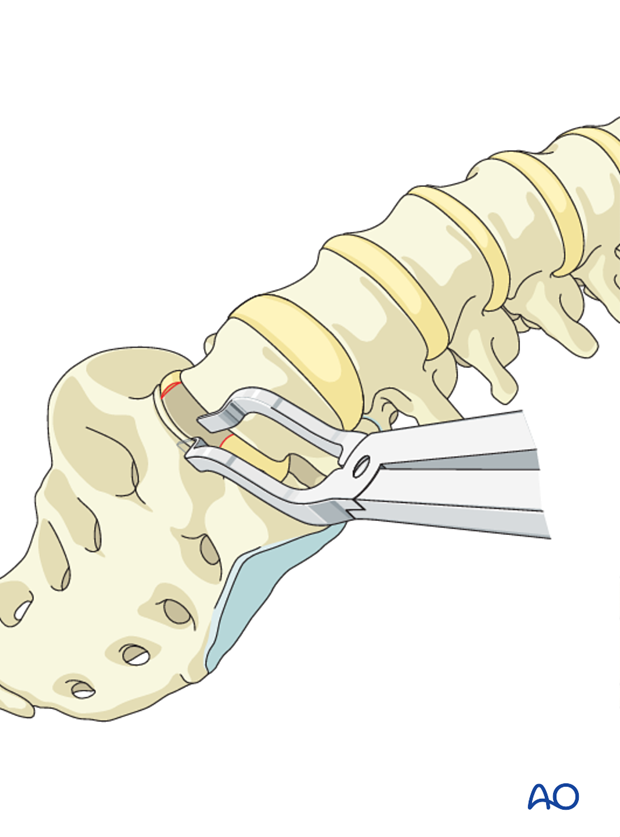
Meticulously remove all cartilage from the endplates. Pieces of cartilage may inhibit fusion if present either on the endplates or in the bony material used for the fusion.
4. Fusion
Once the intervertebral disk space has been mobilized the disk space is packed with cancellous bone.
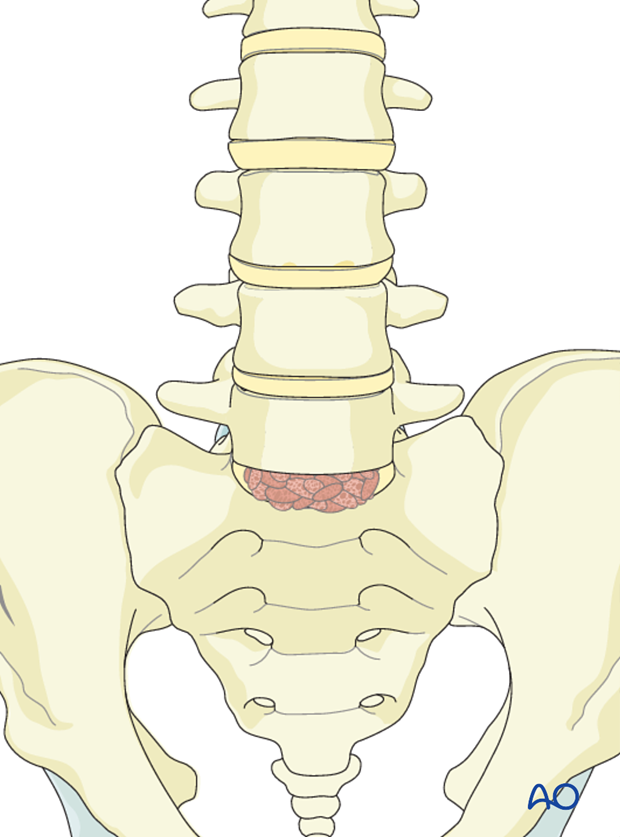
Tricortical graft is harvested from the iliac crest and impacted in to the disk space. Great care must be taken to trim the graft so that it shares axial load with the plate.
Alternatively, allograft or cages may be used.
Indirect decompression can be achieved by restoring maximum disk height.
Restoration of lordosis can be achieved by using wedged cages or allografts.
Solid anterior fixation is required considering that the posterior elements are incompetent due to the pars defect.
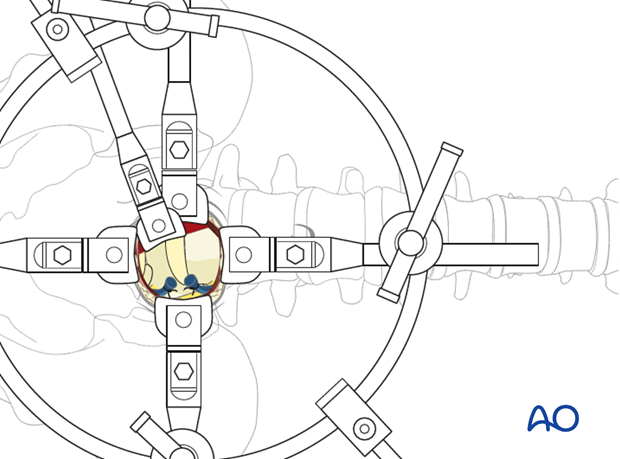
Cage technique
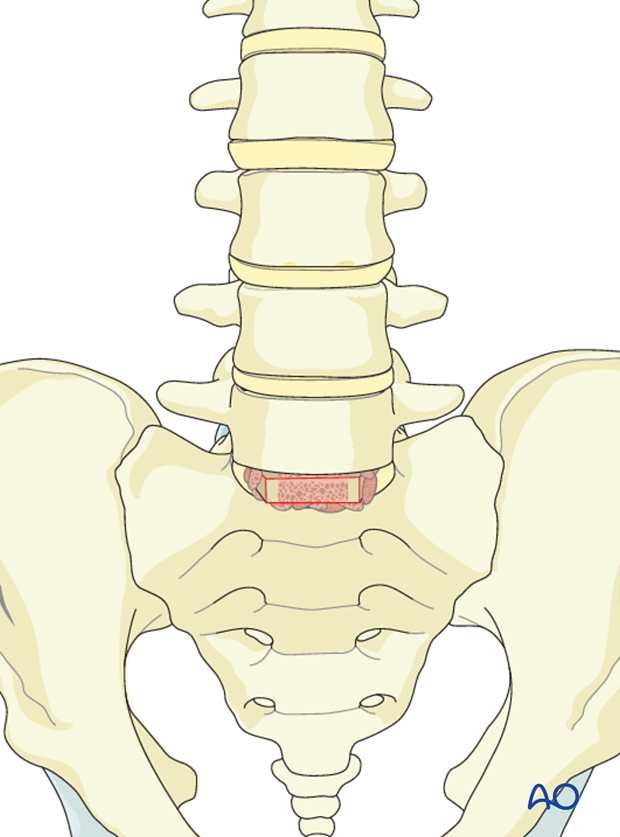
The estimated cage size can be determined from measurements of the patients X-ray using a plastic template.
The cage should be firmly seated in the disk space.
Test cages are used to determine the correct cage size.
The cage may be filled with bone or biomaterials.
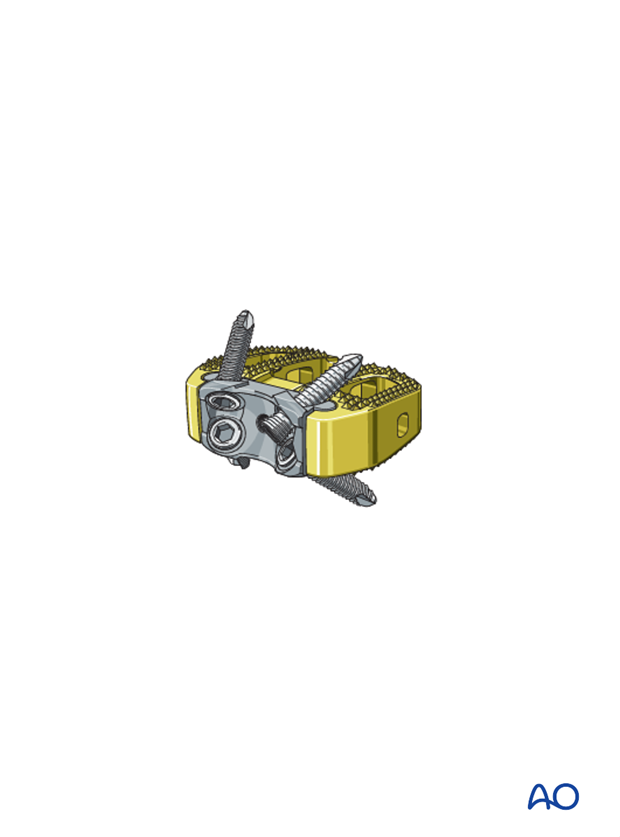
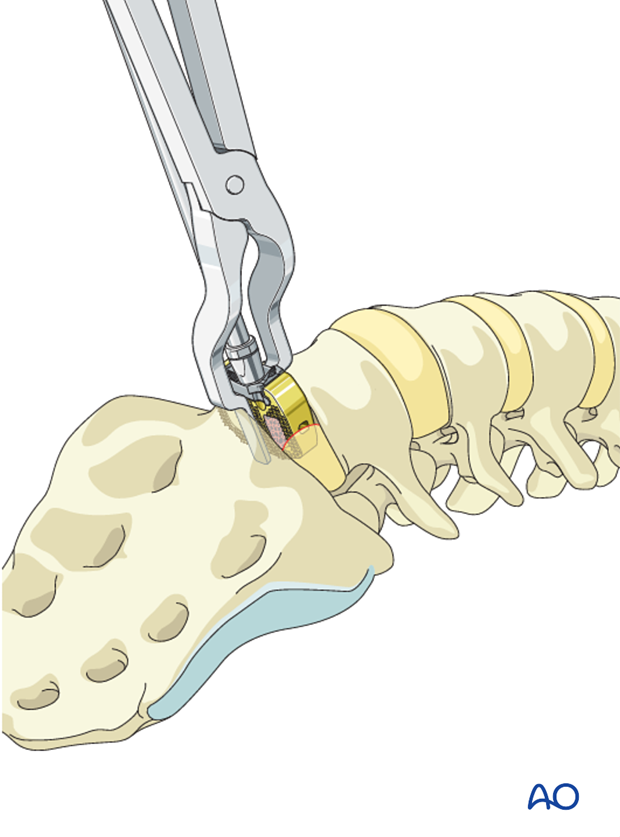
A spreader is used to increase the intervertebral distance and to slide the cage into the disc space.
A screw aiming device is attached to the cage and up to four screws are inserted, two in each vertebra.
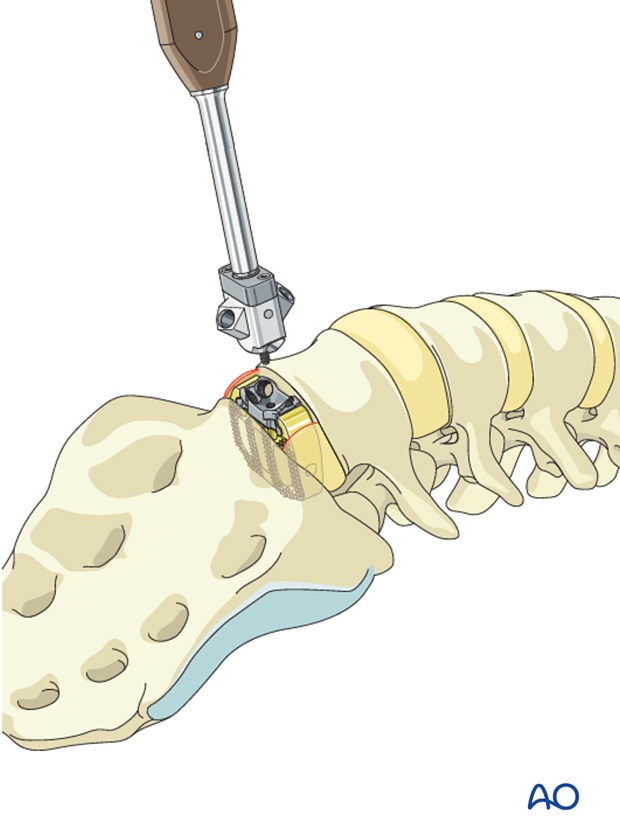
When the cage insertion is completed the flaps are reapproximated.

5. Aftercare following spinal fusion
Detailed postoperative neural assessment must be conducted, specifically looking at the integrity of the L5 nerve root as well as sacral nerves controlling bowel and bladder.
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional. Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year looking for spinal fusion.
Patients with a diagnosis of dysplastic spondylolisthesis run a higher risk of cauda equina and require closer monitoring of their neurological status during and after surgery.












