Primary repair with pars screw
1. Comment on approach
Fluoroscopy is used to confirm the correct level of L5 and S1.
With the patient in prone position, a midline skin incision is performed to access the L5-S1 joint.
The subperiosteal dissection is taken down onto the lamina of L5 exposing the L5-S1 joint
Care must be taken not to violate neither the L5-S1 joint nor the L4-L5 joint.
Dissection is carried laterally onto the transverse process of L5.
2. Decortication
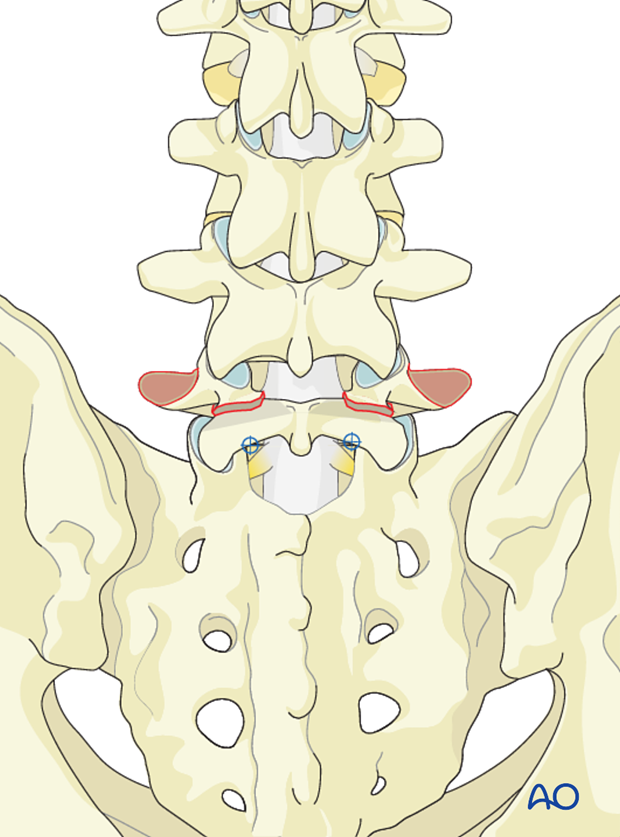
Using a high speed burr the defect in the pars articularis must be decorticated and the pseudoarthrosis excised down to bleeding bone.
Decortication is also taken to the transverse process of L5 along the lamina of L5.
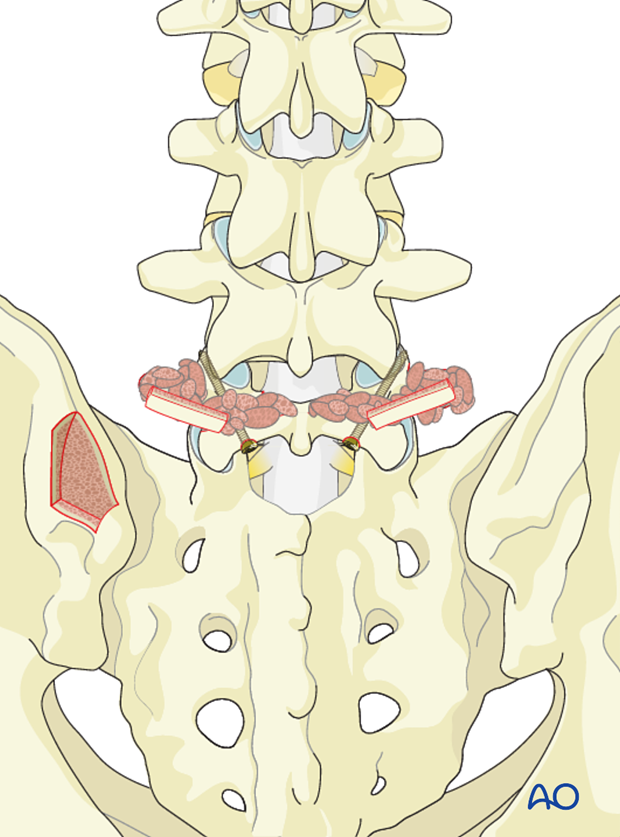
3. Instrumentation
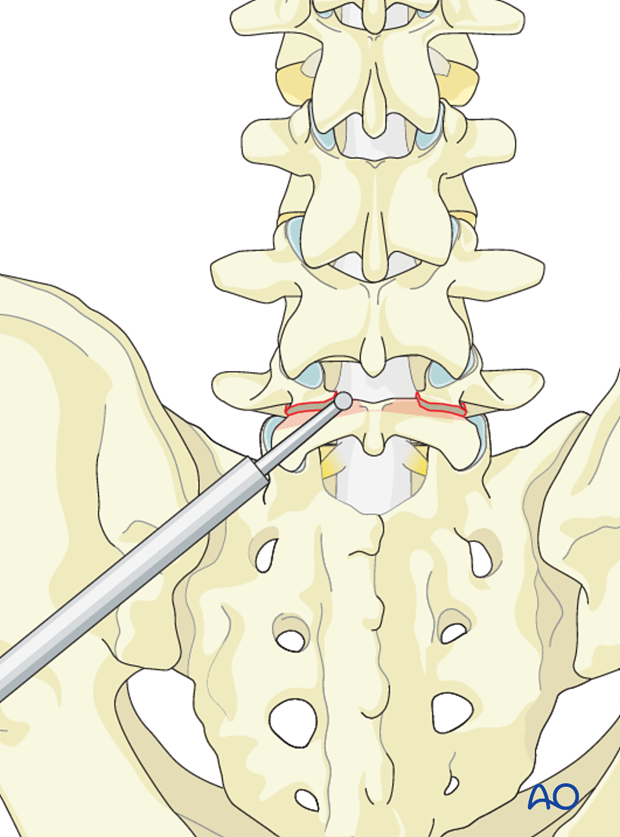
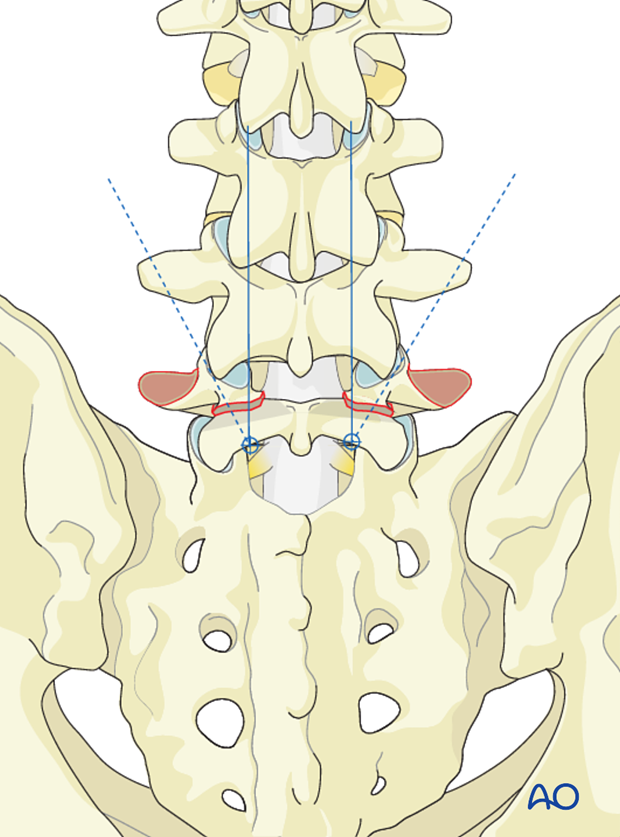
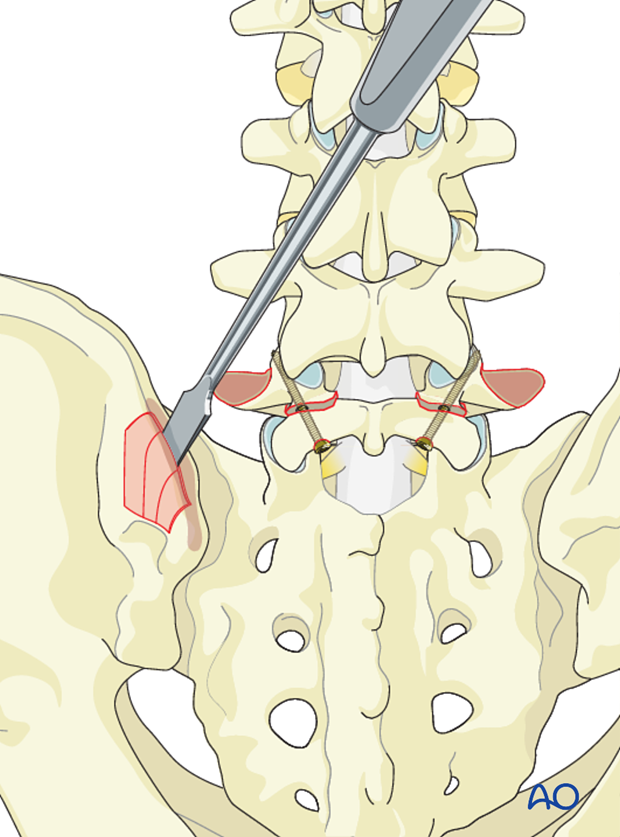
The screw entry point is at the trailing edge of the lamina just medial to the inferior facet of L5.
The screw trajectory runs along the part articularis into the base of the pedicle of L5 in a superolateral direction.
A too anterior screw trajectory may cause the screw to breach into the spinal canal.
A too inferior screw trajector may cause the screw to breach the foramen.
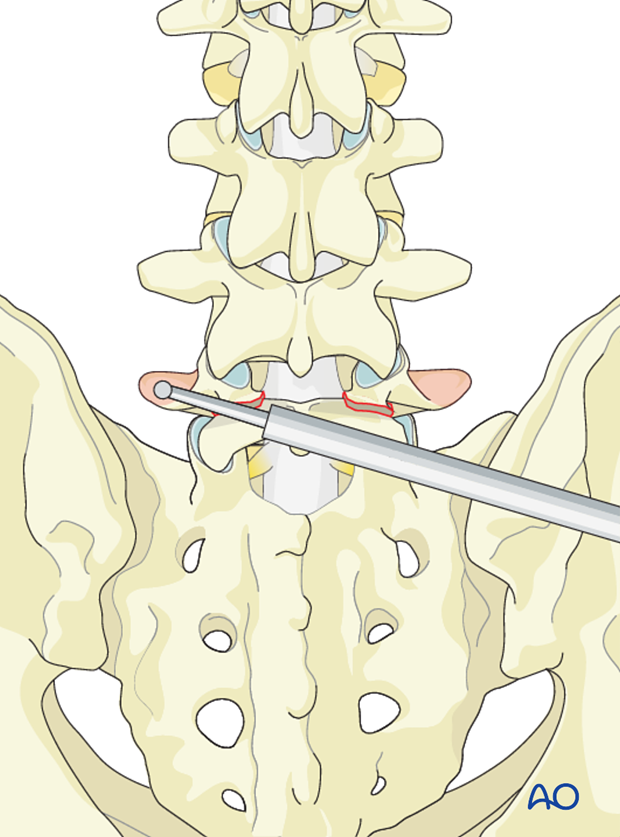
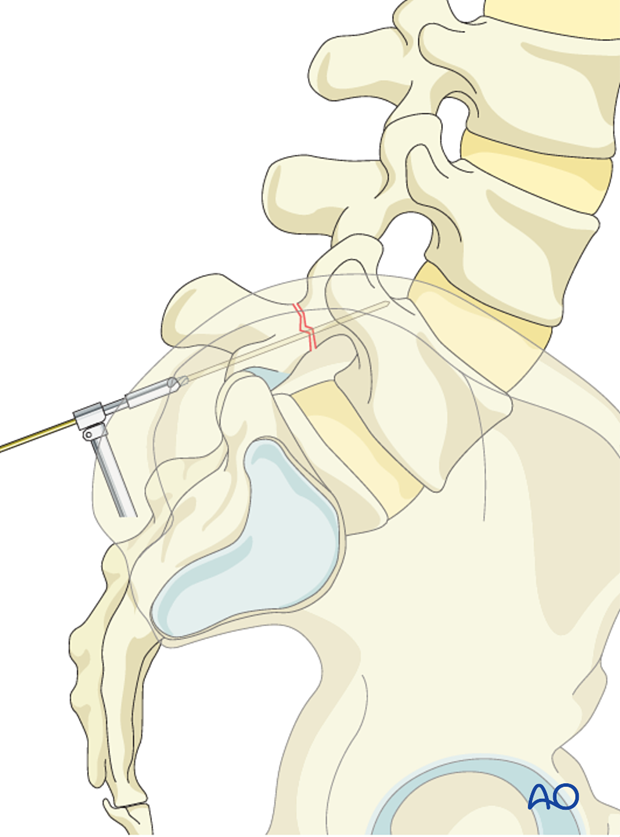
Use of cannulated screws may facilitate correct screw insertion.
The K-wire is inserted under fluoroscopic control.
To reduce the risk of nerve root entanglement an oscillating gear is used.
Once the correct trajectory of the K-wire is verified under fluoroscopical control, a self-tapping 4.5mm cortical screw is inserted over the K-wire and the K-wire removed.
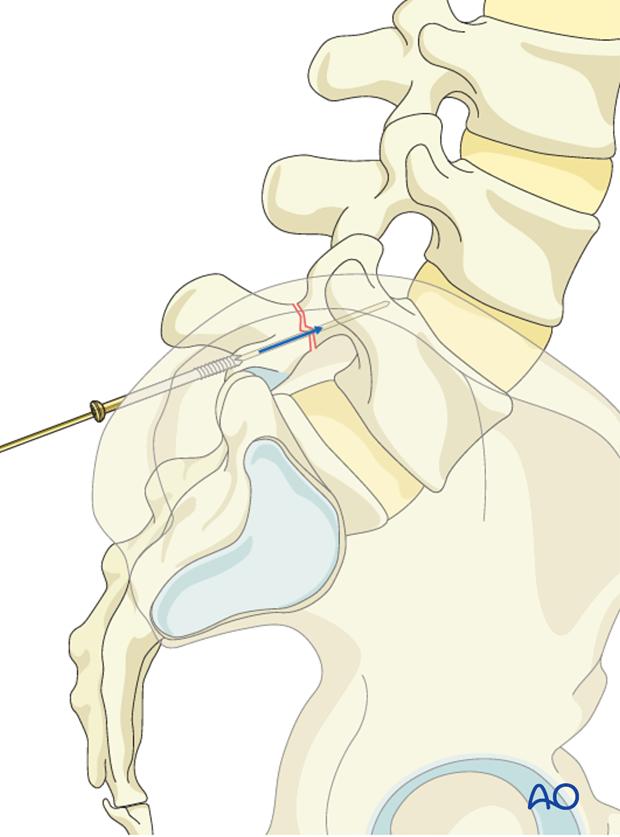
The drill hole is prepared using an oscillating mode to reduce the risk of nerve root entanglement.
A 4.5mm cortical screw is then inserted.
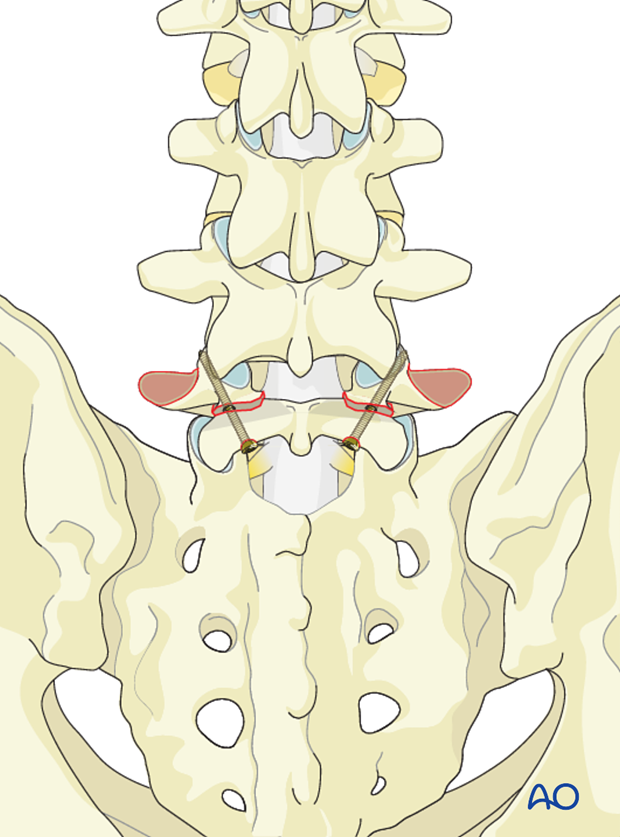
4. Bone grafting
A separate incision is made over the posterior superior iliac crest.
Muscle attached to the outer iliac crest is reflected in a blunt fashion exposing the outer iliac crest.
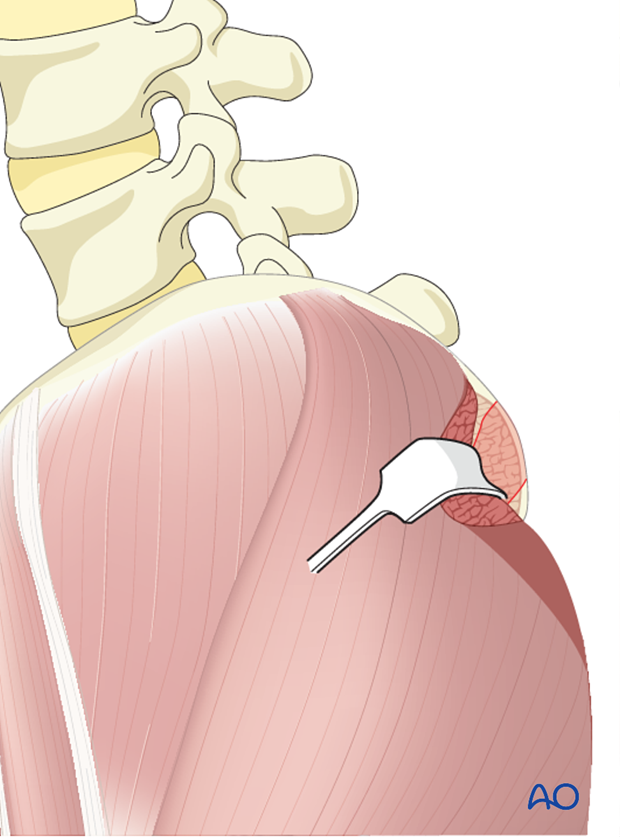
Using an osteotome or a gouge, corticocancellous strips are harvested in 4-5 cm length and 1 cm wide.
Smaller cancellous bone graft is also harvested from the iliac crest and impacted into the pars defect.
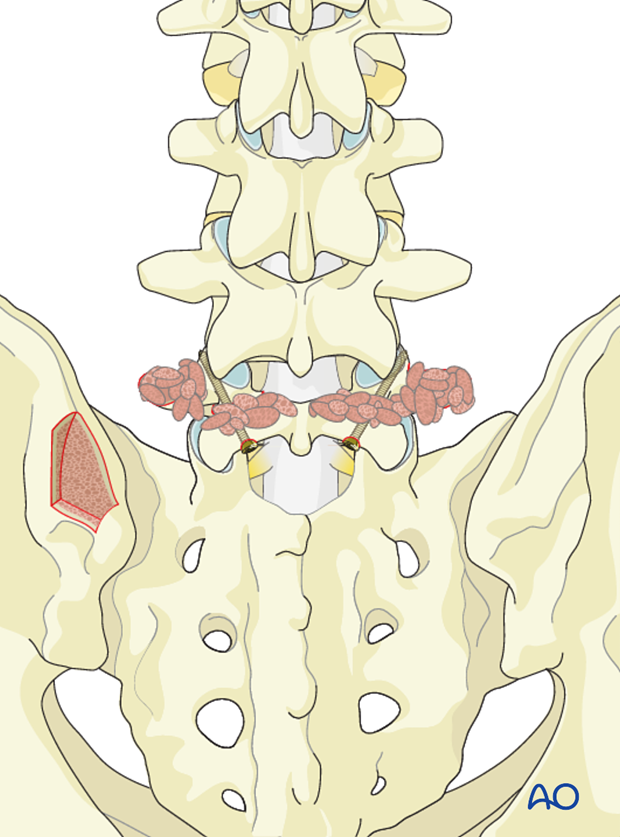
Cortico cancellous strips are laid across the lamina and transverse process.
5. Aftercare
Detailed postoperative neural assessment must be conducted, specifically looking at the integrity of the L5 nerve root as well as sacral nerves controlling bowel and bladder.
Patients with high grade spondylolisthesis that have been reduced are at high risk of postoperative foot drops secondary to neuro traction injury. To minimize such injuries patients are immediately placed in bed with knees and hips flexed. As long as no neuro injury can be identified the leg can be gradually extended after day two. If neuro injury can be identified, the period of flexion should be extended.
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional. Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year looking for spinal fusion.
Patients with a diagnosis of dysplastic spondylolisthesis run a higher risk of cauda equina and require closer monitoring of their neurological status during and after surgery.













