Clinical evaluation
1. Patient history
Patients can present at any age. The chief complaint is lower back pain (mechanical back pain) following activity which typically resolves with rest.
Children may present with short stride gait secondary to nerve root irritability.
Associated symptoms include:
- L5 radiculopathy
- Cauda equina (only severe cases)
- Hamstring tightness/cramps
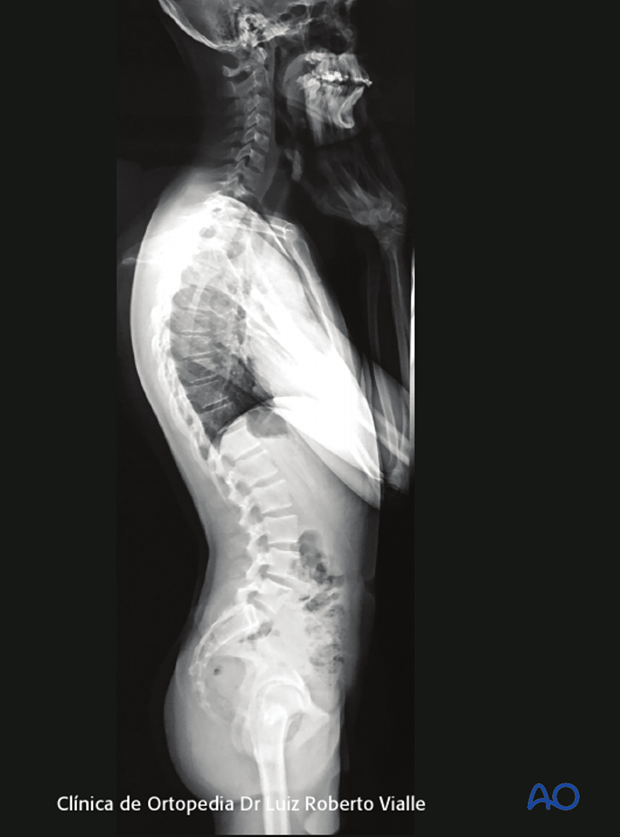
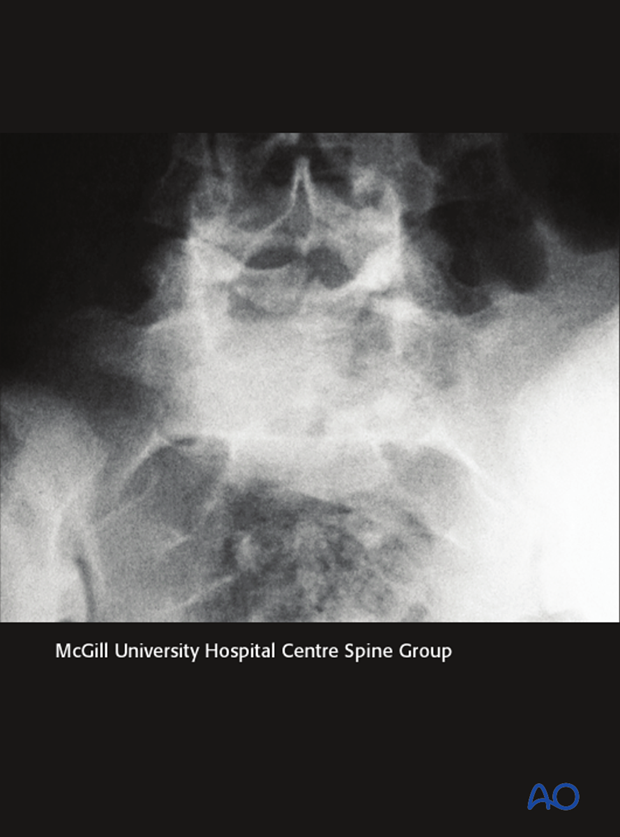
This patient presented with a type 6 spondylolisthesis. In the AP view one can see an accentuated abdominal crease. The sagittal imbalance is easily seen in the clinical lateral view.
Children and young adults involved in sports such as gymnastics, weight lifting, overhead sports such as volley ball and tennis, are at high risk of developing spondylolisthesis.

2. Etiology
Based on the patient history the underlying etiology can be identified based on the Wiltse, Newman and Macnab classification.
- Congenital
- Isthmic
- Degenerative
- Traumatic
- Pathologic
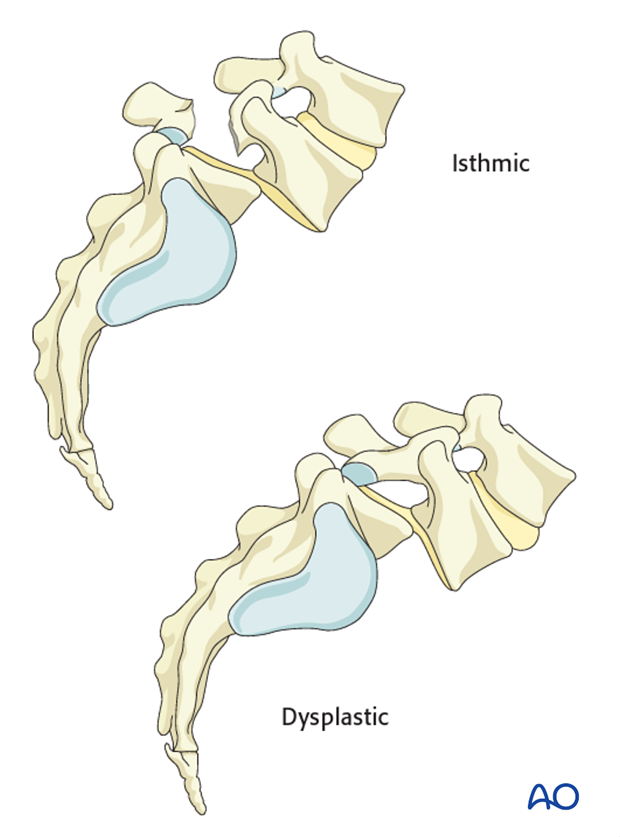
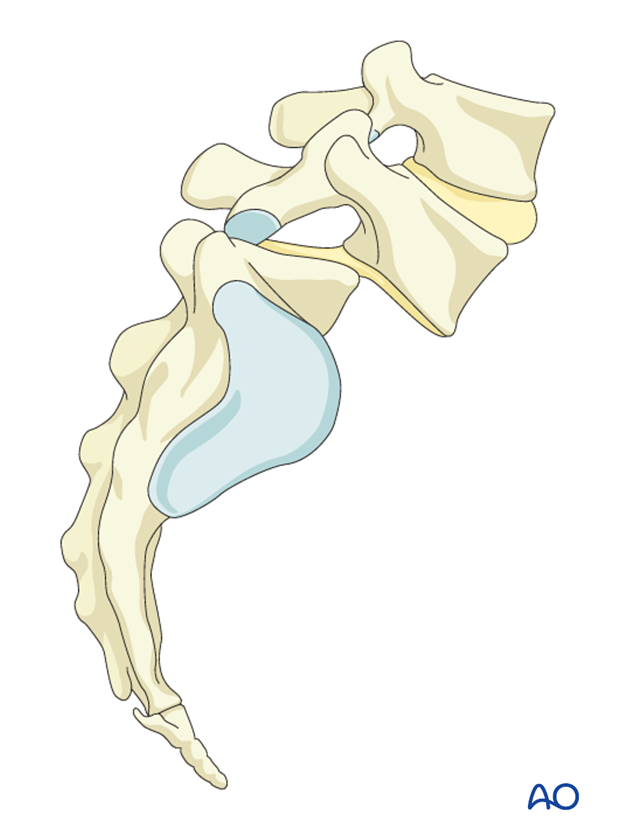
- Dysplastic spondylolisthesis is the result of a congenital deficiency in the L5-S1 facet joints. Elongation of the pars can be seen. The resultant intact pars articularis places the neural elements at risk of compression. Patients may present with cauda equina.
- Isthmic spondylolisthesis results from a stress fracture across the pars articularis. It is thought that repetitive hyperextension leading to impingement of the pars by the inferior facet of the level above causes this stress fracture.
- Degenerative spondylolisthesis is the most frequent type and occurs secondarily to disk degeneration followed by collapse and hypermobility. This results in facet subluxation and segmental slippage.
- Traumatic spondylolisthesis results from acute fracture of the pars intra articularis. Most commonly is associated with disruption of the facet complex.
- Pathologic spondylolisthesis results from metastatic disease leading to weakening of the pars. It is extremely rare.
3. Plain X-ray
X—rays of the lumbar spine are recorded in the following views:
- AP
- Lateral
- oblique
In addition a full lateral spine (including center of femoral heads) view should be obtained to evaluate spinal alignment, spinal balance and pelvic morphology.
4. AP view
What can be seen
- Napoleon hat sign
What it indicates
- High grade spondylolisthesis
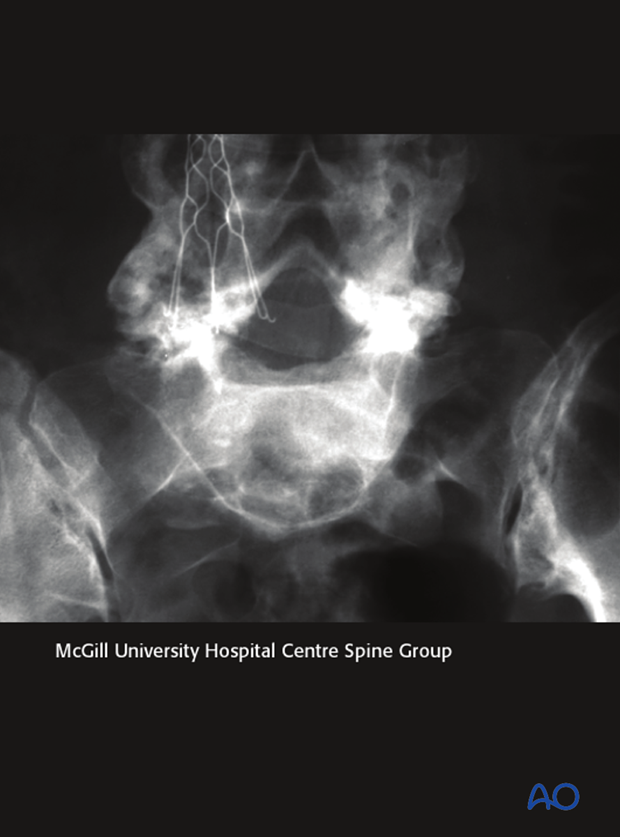
What can be seen
- Spinal bifida occulta
This may be a clue indicating spondylolysis
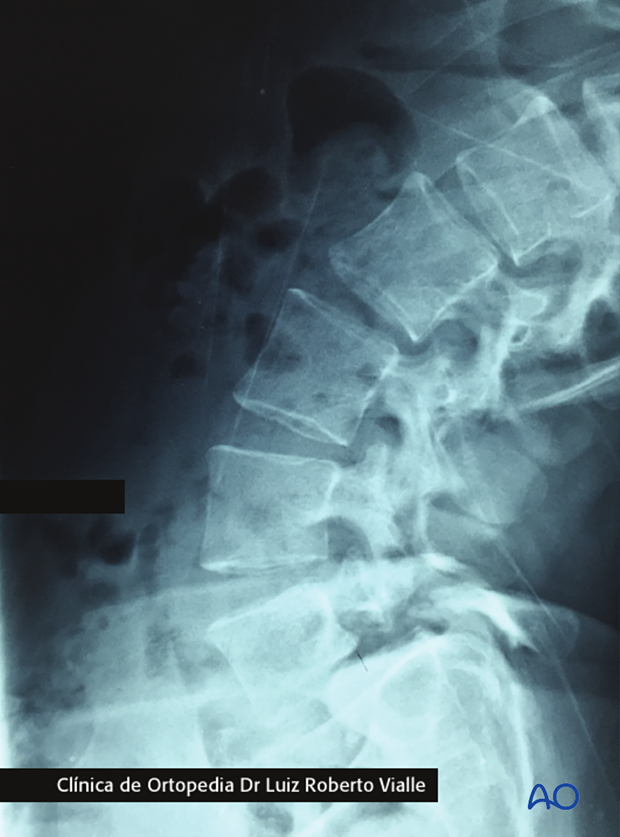
5. Lateral view
What can be seen
- Defect across the pars articularis
This indicates
- Isthmic lysis
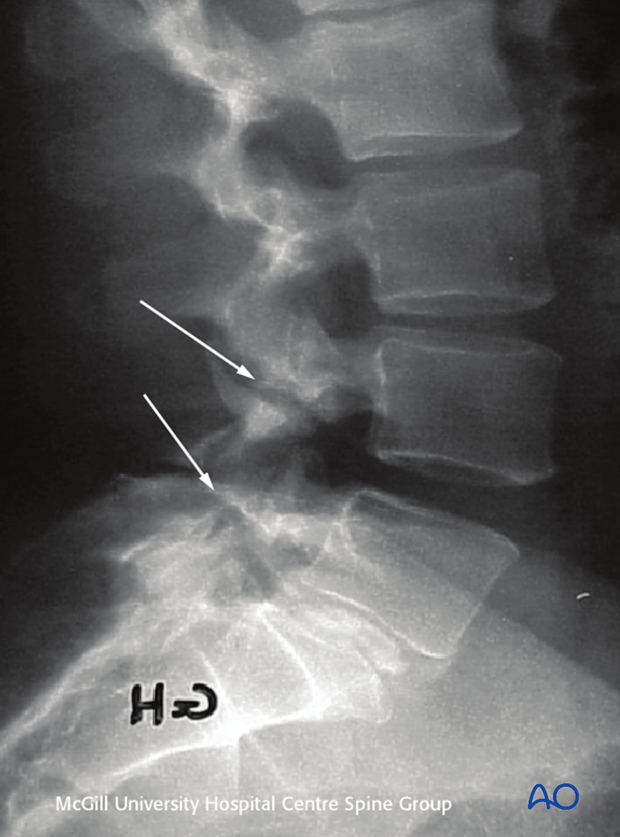
What can be seen
- Anterior displacement of L5 over S1
This indicates
- Spondylolisthesis
What can be seen
- Angulation between L5 and S1
This indicates
- Lumbosacral kyphosis
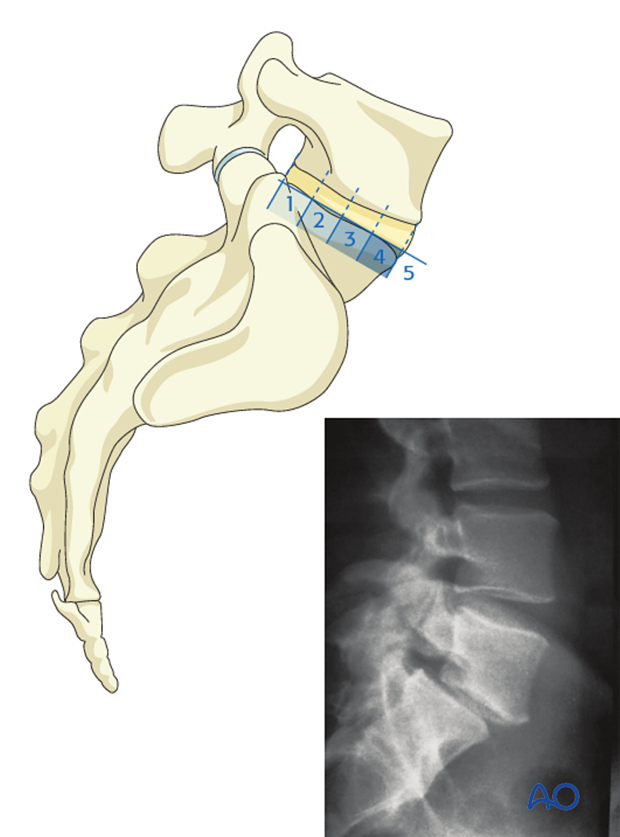
Slip angle: Angle between the end plates of S1 and L5
If the line of the L5 endplate crosses the S1 line anterior to the spine, there is a presence of lumbosacral kyphosis.
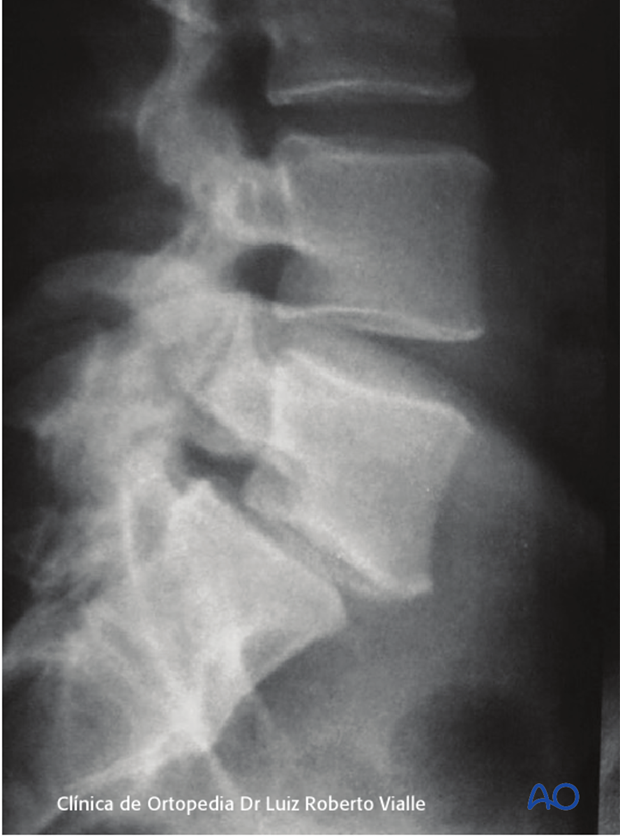
What can be seen
- Dooming of the sacrum, facet hypoplasia, vertical sacrum
This indicates
- Dysplastic spondylolisthesis
6. Radiological analysis
What can be seen
- L5 slip
What it provides
- The degree of listhesis
The degree of listhesis has been classified on a scale of 0-5 by Meyerding.
- Grade 0 is a pars defect only with no translation, also known as spondylolysis.
- Grade 1 is a slip of 0-25 %
- Grade 2 is a slip of 25-50% (x-ray)
- Grade 3 is a slip of 50-75%
- Grade 4 is a slip of 75-100%
- Grade 5 is a slip > 100%, also known as spondyloptosis
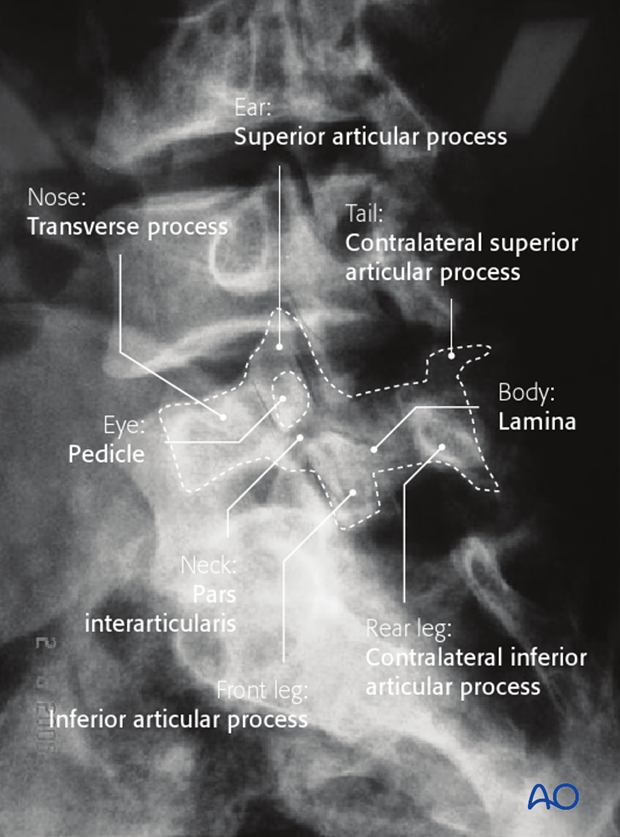
7. Oblique (30°)
What can be seen
- Scottish dog sign (neck discontinuity)
This indicates
- Spondylolysis
8. Full spine
The full lateral spine X-ray is used to evaluate
- Spinal alignment
- Spinal balance
- Pelvic morphology
When the full lateral spine X-ray is recorded, ensure that the patient's legs are fully extended.
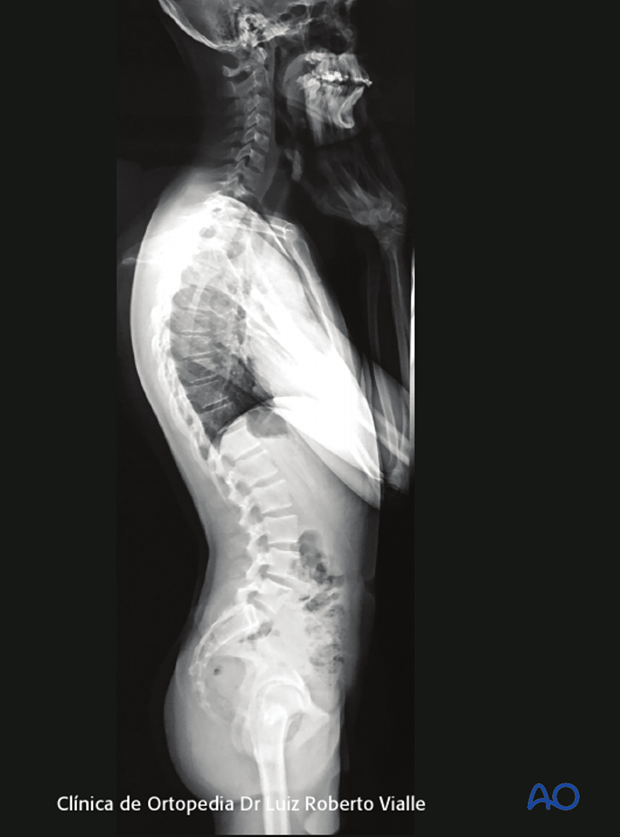
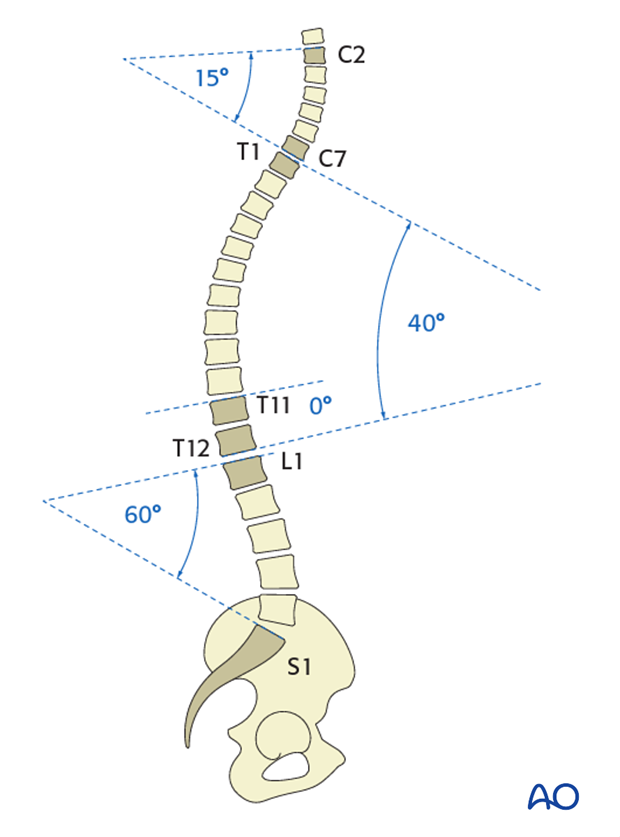
Normal sagittal alignment is as follows:
- 15° Cervical lordosis (C2–C7)
- 40° Thoracic kyphosis (T1–T12)
- 0° Thoracolumbar junction (T11–L1)
- 60° Lumbar lordosis (T12–S1)
Normally lumbar lordosis is 20° greater than the thoracic kyphosis.
If there is a mismatch in spinal alignment the spine will be at a higher risk of imbalance.
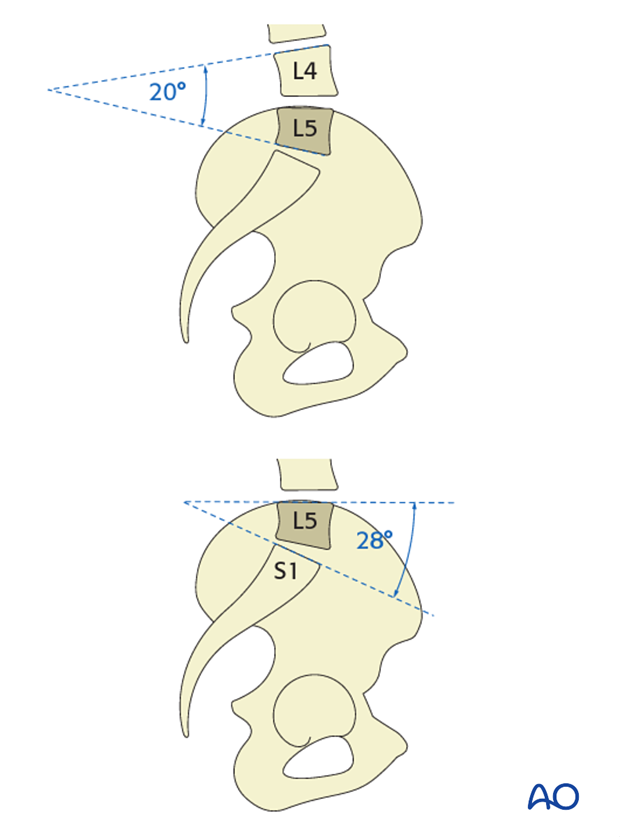
The majority of the lumbar lordosis can be found in the two lowest levels:
- L4–L5 20° of lordosis (representing 28% of total lumbar lordosis)
- L5–S1 28° of lordosis (representing 39% of total lumbar lordosis)
- A total of 48° representing 67% of the total lumbar lordosis
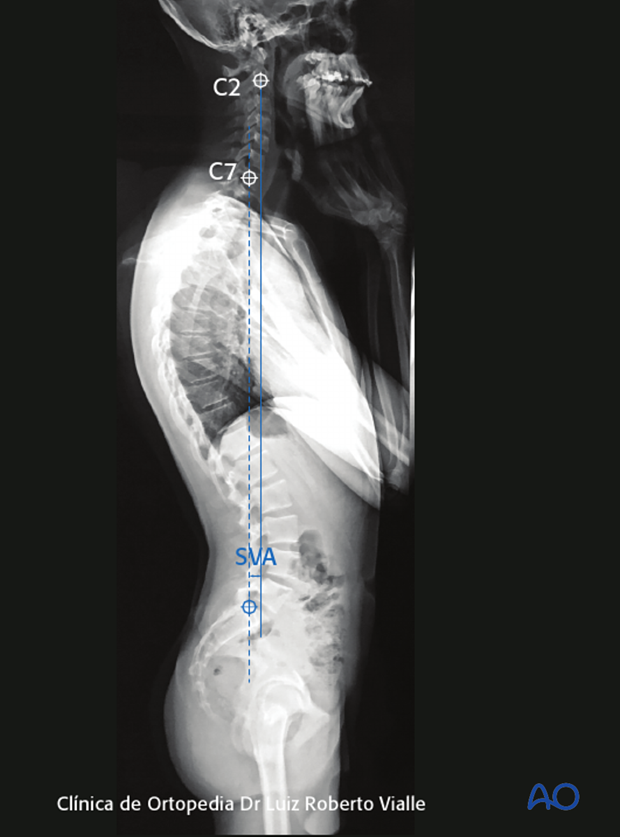
9. Spinal balance
The spine is said to be in balance when it requires the least amount of energy to remain in an upright position.
Measurement of spinal balance is undertaken by establishing the sagittal vertical axis. This is done by drawing a vertical line from the center of C2 or C7.
The distance from the posterior superior corner of S1 to the sagittal vertical axis quantifies sagittal balance:
- Neutral balance +/- 5 cm
- Positive balance SVA > 5 cm anterior to the posterior superior corner of S1
- Negative balance SVA < 5 cm anterior to the posterior superior corner of S1
The spine is said to be in balance when centre of gravity fall behind the centre of the hips.
The sagittal Vertical Axis must fall behind centre of the hips. Considering the hips lock in extension the body does not require to spend any energy to remain upright.
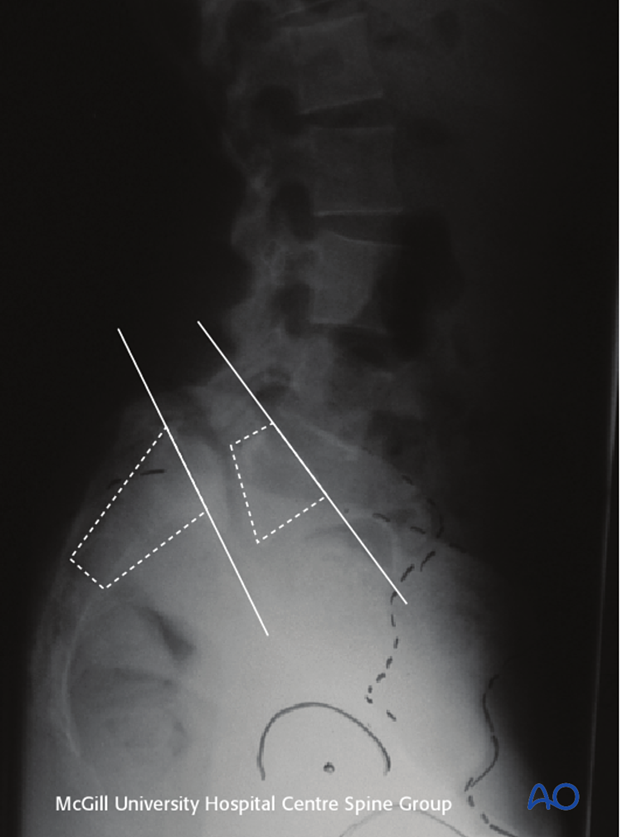
10. Pelvic morphology
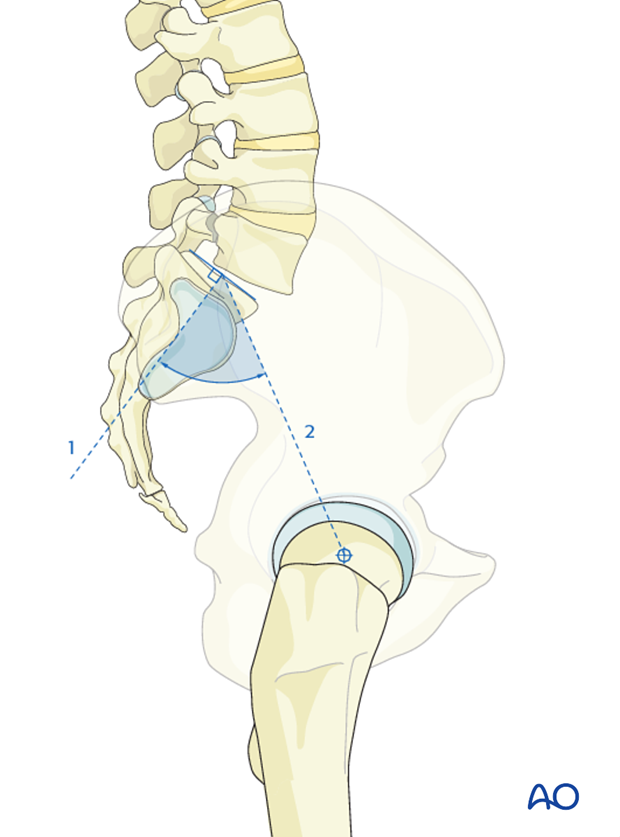
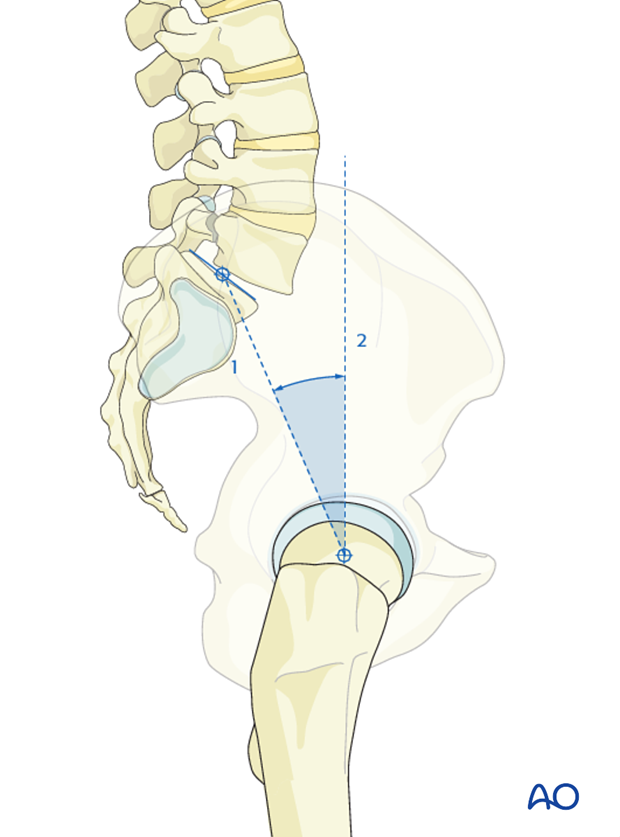
Pelvic incidence is a morphological characteristic of individuals lumbo sacro pelvic junction and is a fixed value.
To determine pelvic incidence identify the following landmarks:
- center of the femoral heads
- midpoint of S1 plate
Draw the two following lines:
- Draw line perpendicular to the sacral endplate from the center of the sacral endplate.
- Draw a line from the center of the sacral endplate to the center of the femoral head.
The angle between these lines is defined as the pelvic incidence.
Normal pelvic incidence is 45-60°
High pelvic incidence is associated with spondylolisthesis and spondylolysis.
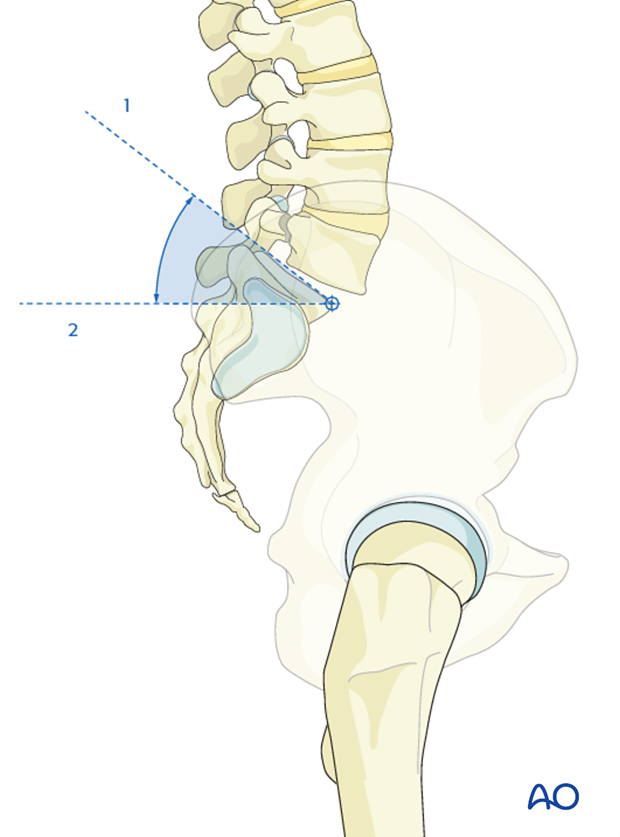
11. Pelvic tilt
Pelvic tilt represents the inclination forward or backward relative to the transverse axis between femoral heads.
It reflects the compensatory efforts to maintain upright position.
To determine pelvic tilt identify the following landmarks:
- center of the femoral heads
- midpoint of S1 plate
To determine pelvic tilt draw a
- line from the center of the sacral endplate to the center of the femoral head.
- vertical line through the femoral head.
The angle between these lines is defined as the pelvic tilt.
Normal pelvic tilt is 7-19° (average 13°)
According to patient's individual anatomy, pelvic tilt can be categorized as normal, small and high.
Sacral slope sets the pitch of L5, thus dictating the lordotic moment.
To determine pelvic slope draw a:
- line parallel to the sacral endplate.
- horizontal line.
The angle between these lines is defined as the pelvic slope.
Average pelvic slope is 41°
Pelvic incidence = Pelvic tilt + Pelvic slope
12. Flexion/extension lateral X-rays of the lumbar spine
Obtaining flexion extension films allows to identify instability as well as reducibility across the spondylolisthesis.
What can be seen
- Flexion extension films illustrates displacement of the L5 in relationship to S1. Motion greater than 5 mm of translation is significant. Resolution of the lumbosacral kyphosis illustrates ease of which intraoperative reduction will be achieve.
This indicates
- Instability

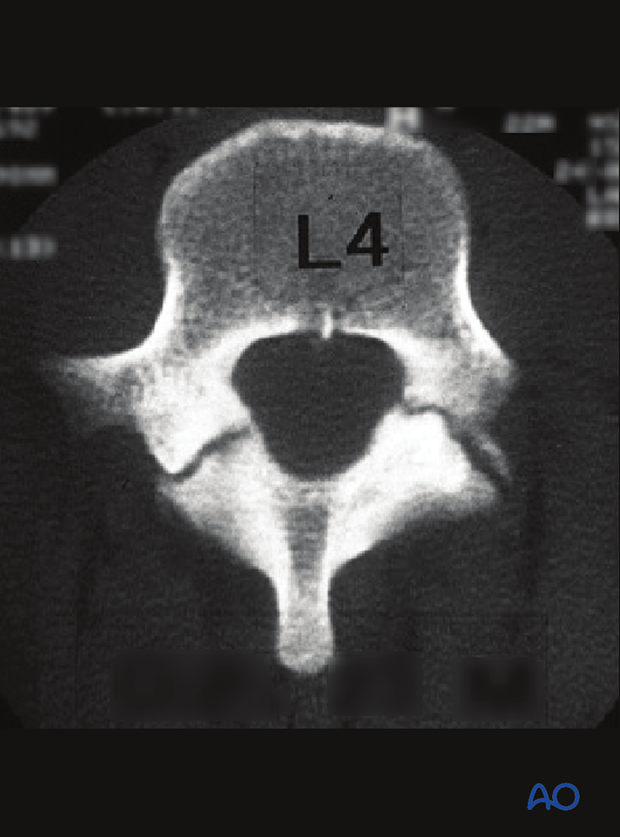
13. CT
CT scans are to be obtained to better delineate the focal anatomy at the lumbosacral junction defining pedicle screw orientation.
14. MRI
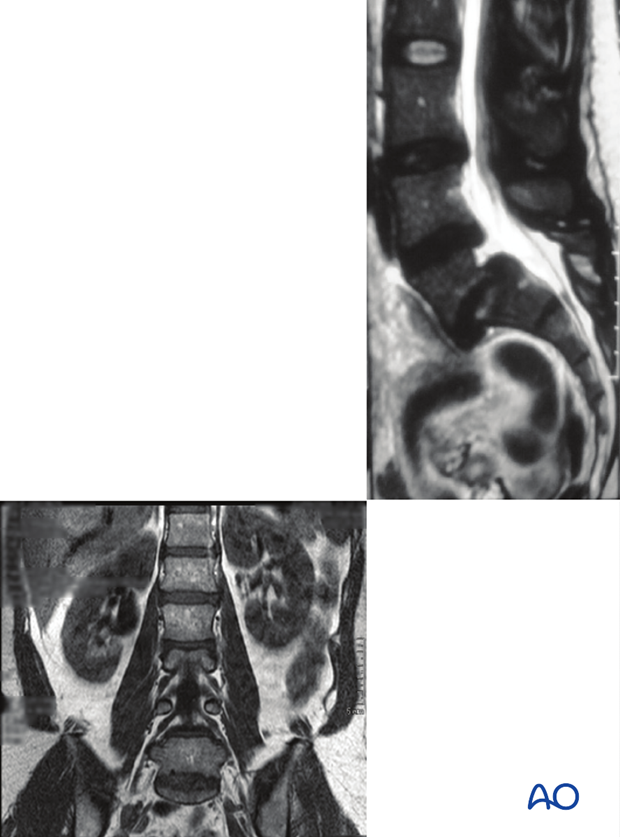
MRI scans are to be obtained to better visualize nerve root compression as well as intervertebral disk integrity.
Disks above spondylolisthesis have a high percentage of degenerative disk disease thus knowledge of this will influence fusion level.
If one contemplates a primary repair, a prerequisite dictates that the L5-S1 disk is healthy.
15. Spec scan
If acute process is thought to be at play, obtaining bone scan can help confirm the acute process.
Bone scans are more detailed than X-rays as they can be used to:
- identify pre-fracture stress reactions as well as small and partial fractures.
- determine whether a fracture is acute (metabolically active) or whether it is a nonunion (no active healing).